■ The superficial palmar arch is completed by either the branches of the deep palmar arch, radial artery, or median artery in about 80% of patients. The deep palmar arch is completed by the superior branch of the ulnar artery, the inferior branch of the ulnar artery, or both in about 97% of patients.
■ The main branches from the superficial palmar arch are the three common digital arteries, which go to the index-middle, middle-ring, and ring-small finger webspaces, as well as the proper digital artery to the ulnar aspect of the small finger. Each digit has a dual blood supply from the radial and ulnar proper digital vessels.
■ The thumb has blood supply from the princeps pollicis artery, which variably arises from the radial artery, the deep palmar, or superficial palmar arch.
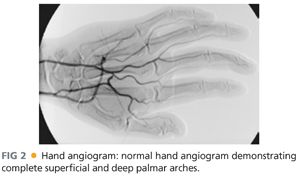
■ Catheter-directed, contrast-enhanced, digital subtraction hand arteriography provides highly detailed anatomic information and represents the gold standard in vascular imaging (FIG 2). However, there are risks from this invasive procedure, which include contrast allergic reaction, vasospasm, contrast-induced nephropathy, thromboembolic events including digital embolization and stroke, and drug reactions precipitated by intraarterial injection of vasoactive agents including Priscoline and nitroglycerin. Hence, catheter-based arteriography is best suited to operative planning in patients already determined to need reconstructive surgery.
■ Magnetic resonance arteriography (MRA) is another option for imaging that is noninvasive, eliminating risks of radiation, contrast reaction, and vasospasm. However, the resolution of MRA is not sufficient for detailed surgical planning.
■ Computed tomographic arteriography (CTA) is also noninvasive, although contrast and (significant) radiation exposure are required for image acquisition. Similar to MRA imaging, the resolution of CTA is typically not sufficient to support detailed surgical planning.
■ Measuring compartment pressures of the hand can be performed with the Stryker Intra-Compartmental Pressure Monitor (Kalamazoo, Michigan), which involves placing the device needle perpendicular to the skin and evaluating individual compartments including sites of maximum swelling of the thenar, hypothenar, and interosseous compartments. The compartment being measured should be at the level of the heart. In an intensive care unit setting, using an arterial pressure line connected to a strain gauge, zeroed at the level of needle entry into the hand, can also provide rapid and accurate compartmental measurements. A 20-gauge needle is inserted into the compartment and flushed, with measurement acquired after the flush bolus has disseminated in the compartment and the pressure spike from the flush returns to baseline.
SURGICAL MANAGEMENT
Preoperative Planning
■ The overall goal is to restore distal blood flow to baseline/maximal levels, given anatomic constraints, available arterial conduit, central arterial perfusion pressure and cardiac output, and end-organ (hand) viability.
■ Treatment of thromboembolic disease can include medical management and catheter-based chemical and mechanical thrombolysis, angioplasty, and stenting to maximize arteriolar outflow and arterial inflow, respectively. Upper extremity revascularization techniques are discussed in Chapter 10.
■ End-to-end primary vascular repair can be performed if arteries are tension free after mobilization, and the zone of injury is accurately identified to be uninvolved in the site of anastomosis. If there is any difficulty in approximating the vessels ends, then vascular grafts are preferred.
■ In ulnar or radial artery thrombosis, reconstruction is preferred over ligation. Proximal reconstructions are attempted even in the setting of more distal occlusions, based on the rationale of augmenting collateral flow via direct or indirect means.3
■ Determining venous or arterial graft harvest site is important for preoperative planning. Dorsal hand or foot veins provide the most appropriate size match for intrinsic arteries of the hand (and feet). Donor sites for arterial graft conduits include the deep inferior epigastric artery, subscapular artery, thoracodorsal artery, or descending branch of the lateral femoral circumflex artery. Typically, arterial grafts patency rates are superior to those obtained with venous grafts.4
■ For chronic ischemia, medical management including pharmacologic treatment with vasodilators, topical nitroglycerin, calcium channel blockers, or botulinum toxin should be attempted first, prior to surgical management.5 Evidence of gangrene, osteomyelitis, and so forth of the involved digit may require debridement or digital amputation.
■ Periarterial sympathectomy in the hand, which involves stripping the adventitial layers from affected arteries, removes sympathetic nerve input to the media and has proven effective in promoting distal finger lesion healing in scleroderma patients. In scleroderma specifically, the thickened adventitia apparently contributes to decreased digital arterial flow.6,7
Positioning
■ Hand surgery is usually performed with the patient in the supine position. The operated hand is placed on a hand surgery table, which is stabilized by two legs. Reconstructive surgery may be performed under tourniquet, depending on systemic comorbidities and the adequacy of arterial inflow. For tourniquet control, the upper arm is well padded with Webril (cotton) wrapped circumferentially, and then an 18-in (or appropriately sized) pneumatic tourniquet is secured around the upper arm (FIG 3). Alternatively, depending on inflow status, the tourniquet may be placed at the forearm or wrist. Finally, an impervious barrier (3M Steri-Drape 1000) is placed circumferentially just distal to the tourniquet to prevent see page of the sterile prep solution. The arm/hand are then sterilely prepped and draped.

■ Intraoperatively, the arm is exsanguinated with an elastic bandage (Esmarch bandage) wrap and elevation immediately prior to tourniquet inflation. In adults, the tourniquet is typically inflated to 250 mmHg; in children, it is set 100 mmHg above the systolic pressure. The tourniquet inflation should last no more than 2 hours and must be deflated for a 20-minute interval to allow reperfusion prior to reinflation, if needed. Consideration should be made to establishing systemic anticoagulation prior to tourniquet inflation when indicated.
■ Appropriate concurrent sterile prep should be performed on graft harvest sites as necessary.
■ Microsurgery prep includes ensuring that the operating scope is working properly and sterilely draped. Positioning is extremely important to reduce surgeon fatigue, which includes ensuring good table height, working height (with appropriate padding support of the wrists with stacks of surgical towels), and sitting position. Microsurgery instruments should be available as necessary, depending on the level of revascularization considered. 9-0 and 10-0 sutures are employed for more distal reconstructive procedures and digital reimplantation. For proximal radial and ulnar reconstruction procedures, at or immediately adjacent to the wrist, 2.5× to 3.5× surgical loupe magnification will provide adequate anatomic resolution and suture placement for operators with normal visual acuity.



