and Alessandra Cancellieri2
(1)
Department of Radiology, Bellaria Hospital, Bologna, Italy
(2)
Department of Pathology, Maggiore Hospital, Bologna, Italy
Radiology | Giorgia Dalpiaz Sara Piciucchi |
Asbestosis | Asbestos-induced pneumoconiosis | Page 80 |
CVD | Collagen vascular diseases – scleroderma | Page 82 |
Drug toxicity, chronic | Methotrexate | Page 84 |
HP, chronic | Hypersensitivity pneumonitis, chronic | Page 86 |
IPF | Idiopathic pulmonary fibrosis | Page 88 |
NSIP | Nonspecific interstitial pneumonia | Page 90 |
PPFE | Pleuropulmonary fibroelastosis | Page 92 |
Sarcoidosis, chronic | Sarcoidosis, chronic | Page 94 |

Asbestosis
Definition
Asbestosis is a pneumoconiosis that occurs secondary to the inhalation of asbestos fibers. Disease usually occurs approximately 20 years following the initial exposure.
Histologically, asbestosis is defined as an interstitial pulmonary fibrosis associated with the presence of intrapulmonary asbestos bodies or asbestos fibers. The earliest changes of fibrosis occur in the peribronchiolar region of the lobular core. As the fibrosis progresses, it involves alveolar walls and lobular periphery and interlobular septa. Visceral pleural thickening often overlies areas of parenchymal fibrosis.
Pneumoconiosis
Ross RM (2003) The clinical diagnosis of asbestosis in this century requires more than a chest radiograph. Chest 124:1120
High-Resolution CT: HRCT
Key Signs
In patients with early asbestosis, dot-like opacities are visible in the subpleural lung (►). Subpleural, confluent curvilinear opacities are also present. These correlate with the presence of peribronchiolar fibrosis extending to involve the contiguous airspaces and alveolar interstitium.
Fine fibrosing reticulation such as intralobular interstitial thickening ( ).
).
Irregular thickening of interlobular lines and irregular interfaces.
Traction bronchiolectases.
Architectural distortion.
Parenchymal bands, with possible “Crow’s foot” appearance (50–80 %).
Subpleural lines.
Distribution
Basal predominance of pulmonary abnormalities. It is also characteristic for these lung abnormalities being most severe in the posterior lung and subpleural regions (sagittal image  ). The abnormalities are usually bilateral and symmetric.
). The abnormalities are usually bilateral and symmetric.
 ). The abnormalities are usually bilateral and symmetric.
). The abnormalities are usually bilateral and symmetric.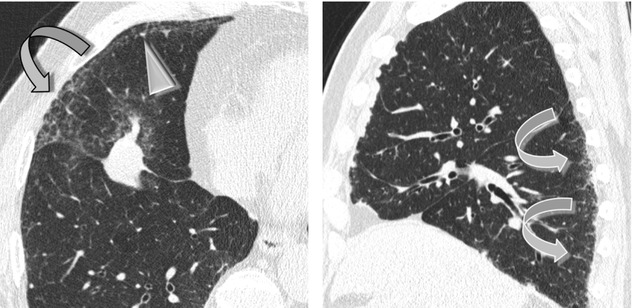
CT scans obtained in a prone position may be useful for distinguishing normal increased opacity from dependent lung regions and mild fibrosis.
Ancillary Signs
Ground-glass opacity (GGO), when present, is usually seen in association with reticulation (see the axial image above) and traction bronchiectases and reflects fibrosis. When seen in isolation, GGO correlates with the presence of mild alveolar wall and interlobular septal fibrosis or edema.
Non-parenchymal Signs
Pleural thickening or plaques (➨): these may be bilateral, of varying length, but with a thickness <1 cm and calcified in 10–15 % of cases. They are typically absent in the apices or in the costophrenic sinuses and tend to be arranged in a spiral pattern extending superoanterior to posteroinferior (“propeller blade” distribution). The presence of pleural plaques often lends support to the radiologic diagnosis of asbestosis. Pleural disease is often present (80 %). The diaphragmatic pleura is commonly involved in patients who have asbestos-related pleural disease.
Rounded atelectasis () is a form of peripheral lobar collapse that develops in patients with pleural disease and in 80 % of patients with asbestos exposure. It usually occurs in the subpleural, posterior, or basal region of the lower lobes. This lesion has oval morphology and is strictly adhering to a pleural plaque. It has a curvilinear tail, frequently referred to as the “comet tail sign”. Volume loss of the involved area is also visible. The contrast enhancement of the “nodule” is homogenous. Rounded atelectasis is often unilateral (please also refer to Comet tail sign in the “Case-Based Glossary with Tips and Tricks”).
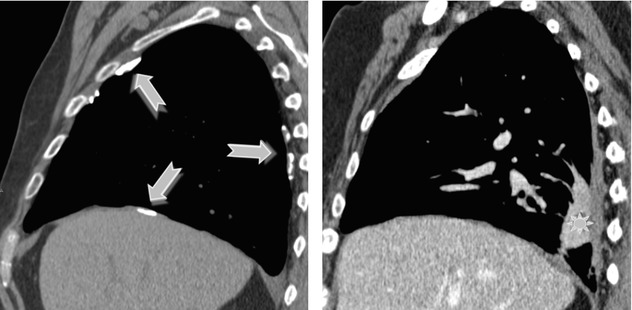
It is important to distinguish rounded atelectasis from lung cancer, which has an increased incidence in asbestos-exposed individuals. For the differential diagnosis contrast-enhanced CT scan and CT-PET can be useful in making differential diagnosis. Because rounded atelectasis represents collapsed parenchyma, it appears vascularized (hyperdense) and with little SUV on CT-PET.
Course and Complications
The early stage may progress to severe fibrosis with honeycombing and traction bronchiectases with complete destruction of the alveolar architecture.
Pleuropulmonary malignancy may occur, with a period of latency of at least 20 years between the initial exposure to asbestos and the development of a pulmonary carcinoma or pleural mesothelioma.
HRCT findings of advanced asbestosis are similar to those seen in patients with IPF. However, when the lung fibrosis is associated with typical asbestos-related pleural abnormalities, the diagnosis of asbestosis may be suggested.
Chong S (2006) Pneumoconiosis: comparison of imaging and pathologic findings. Radiographics 26(1):59–77
Kim KI (2001) Imaging of occupational lung disease. Radiographics 21(6):1371
Collagen Vascular Disease (CVD): Scleroderma
Definition
Collagen vascular disease (CVD) is a heterogeneous group of diseases, with a pleomorphic involvement of various organs or tissues, characterized by the presence of circulating autoantibodies. CVD can cause variety of ILDs, with an histology identical to the idiopathic interstitial pneumonias. The most common patterns include NSIP (the most frequent), UIP, OP, and LIP. The pattern of scleroderma, including also the pleuritic and vasculitis form, will be covered in this Chapter as the representative example of a fibrosing CVD. Based on international collaborative data, interstitial lung disease is considered as the most frequent cause of death in progressive systemic sclerosis (scleroderma).
CVD – progressive systemic sclerosis (PSS)
Other collagen vascular diseases which can induce a fibrosing alveolitis are systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), CREST syndrome, Sjögren’s syndrome, dermatomyositis–polymyositis (DM/PM), and mixed connective tissue disease (MCTD). Lung fibrosis is the most common pattern of abnormality, with NSIP pattern as much more common than UIP pattern (the so-called “secondary” NSIP or UIP pattern).
Tanaka N (2004) Collagen vascular disease-related lung disease: high-resolution computed tomography findings based on the pathologic classification. J Comput Assist Tomogr 28(3):351
High-Resolution CT: HRCT
Key Signs
Findings reflect the frequent NSIP histological pattern (80 %) related to scleroderma and are characterized by:
Confluent ground-glass opacity (GGO)
Fine fibrosing reticulation (80–90 %) and irregular interface sign
Traction bronchiectasis and bronchiolectasis ( )
)
Volume loss of different entity associated to angulation and low-displacement of the fissure. The finding assumes a festooned course (►): possible traction effect of the mediastinal outline ( )
)
Distribution
Often symmetric lower lobe distribution. It is variously distributed in its axial plane (peripherally predominant or diffuse).
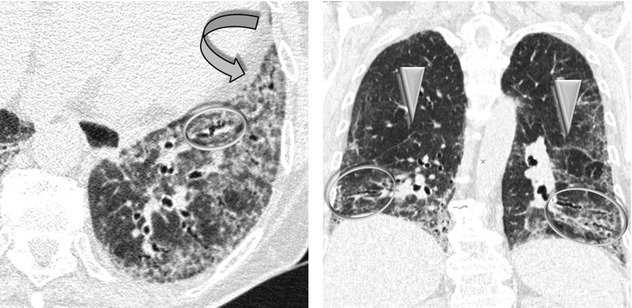
Predominant GGO often correlates with the presence of inflammation. On the other hand, the presence of a reticular pattern correlates with the presence of fibrosis on the pathologic specimens. However, keep in mind that GGO may also represent fibrosis in a context of fibrosing reticulation, traction bronchiectasis, and bronchiolectasis (“fibrotic GGO”). The lung fibrosis related with scleroderma is associated with a much better prognosis than that found in IPF, most likely due to predominant NSIP histology.
Lynch DA (2009) Lung disease related to collagen vascular disease. J Thorac Imaging 24(4):299
Ancillary Signs
Honeycombing, when present, is usually mild. In patients with pathologic UIP pattern, honeycombing is more frequent.
Possible small nodules have been reported in association to follicular bronchiolitis.
Consolidation.
Non-parenchymal Signs
Esophageal dilation is found in up to 80 % of cases (➨).
Pulmonary arterial hypertension confirmed by cardiac catheterization is present in about 10–30 % of patients. It is also present especially in the limited form of scleroderma (CREST syndrome). Usually, it causes enlargement of the main and proximal pulmonary arteries ( ); however, normal-sized pulmonary arteries do not exclude the diagnosis.
); however, normal-sized pulmonary arteries do not exclude the diagnosis.
Pleural thickening or effusion is not a common manifestation, and when it occurs, it is usually accompanied by parenchymal lung disease. Asymptomatic pericardial effusions commonly occur in scleroderma.
Enlarged mediastinal nodes (60 %).
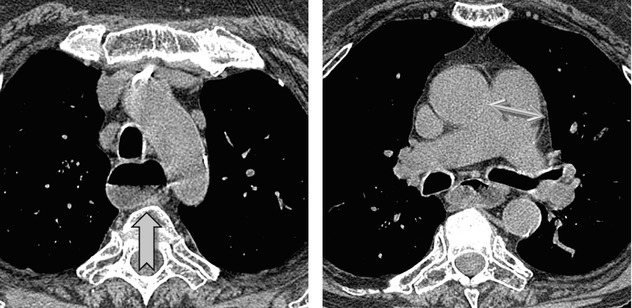
Parenchymal consolidation can be present in association with organizing pneumonia (OP) or aspiration pneumonia.
In the majority of these patients, the degree of pulmonary hypertension (and degree of pulmonary arterial involvement) is out of proportion to the extent of lung disease, because CVD directly affect the pulmonary vasculature.
Pleural or pericardial involvement is not present in IPF and therefore it results useful in the differential diagnosis of PPS from this disease.
Course and Complications
In the majority of cases, the fibrosis progresses on long-term follow-up with worsening due to an increasing extent of GGO and honeycombing. The latter correlates with the decrease of DLCO.
Pulmonary arterial hypertension is a leading cause of death related to progressive systemic sclerosis.
Several studies have demonstrated an increased frequency of some malignancies.
Mayberry JP (2000) Thoracic manifestations of systemic autoimmune diseases: radiographic and high-resolution CT findings. Radiographics 20(6):1623
Capobianco J (2012) Thoracic manifestations of collagen vascular diseases. Radiographics 32(1):33
Drug Toxicity, Chronic: Methotrexate
Definition
Initially administrated as antineoplastic drug, methotrexate (MTX) has been shown as an effective anti-inflammatory agent and is now widely used in nonneoplastic inflammatory conditions, including psoriasis, primary biliary cirrhosis, inflammatory bowel diseases, and, most commonly, rheumatoid arthritis. Methotrexate-induced pulmonary toxicity occurs in 5–10 % of patients and is unrelated to the duration of treatment or cumulative dose.
MTX pneumonitis
It should be noted that the same drug may cause different types of damage in the lung tissue, even in sequence. For example, methotrexate itself may cause pulmonary edema (PE), organizing pneumonia (OP), diffuse alveolar damage (DAD), and hypersensitivity pneumonitis (HP), although less frequently than chronic interstitial pneumonia such as nonspecific interstitial pneumonia (NSIP).
Bonniaud P (2014) Drug-induced interstitial lung diseases. Rev Prat 64(7):951 www.pneumotox.com
High-Resolution CT: HRCT
Key Signs
Histological NSIP pattern is the most common manifestation of MTX-induced lung disease appearing as:
Scattered or diffuse areas of ground-glass opacity (GGO)
Fine fibrosing reticulation and architectural distortion ( )
)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


