High pressures in the first breaths
Expulsion of lung fluid
Decrease in lung vascular resistance
Constriction and functional closure of the arteriosus ductus
High distensibility of the rib cage
Low functional residual capacity
Increased pulmonary resistance
Low lung distension
High respiratory rate
Nasal breathing
Lower CO2 ventilatory response in preterm infants
Paradoxical hypoxemia response
High minute ventilation
Increase of dead space in preterm infant
High oxygen consumption
Active Hering-Breuer’s and Head’s reflexes
Pulmonary arteries with larger muscles
Distensibility of the rib cage is greater in the newborn, especially in the preterm infant, which makes it difficult to maintain an adequate lung residual capacity, and can also ease alveolar collapse when there is a low lung distension.
Of the resistance forces, 20% correspond to the friction of the lung against the rib cage and 80% correspond to airway resistance. In the newborn, the nostrils are the point of greatest airflow resistance in the airway. This is important, considering that during this period, breathing is done mostly through the nose. Lung airway resistance is greater in the newborn than in the adult. In addition, because of the small size of the airway in the newborn, any obstructive process will noticeably increase lung resistance.
Comparison of respiratory variables per age
Newborn | Adult | |||
|---|---|---|---|---|
Respiratory frequency | (f) | 34–45 | 13 | rpm |
Tidal volume | (Vt or Vc) | 6–8 | 7 | ml/kg |
Alveolar volume | (Va) | 3.8–5.8 | 4.8 | ml/kg |
Anatomical dead space | (VD) | 2–2.2 | 2.2 | ml/kg |
Minute ventilation | (Ve) | 200–260 | 90 | ml/kg/min |
Alveolar ventilation | (Va) | 100–150 | 60 | ml/kg/min |
Functional dead space | (VD) | 77–99 | 30 | ml/kg/min |
Dead space/tidal volume | (VD/Vt) | 0.27–0.37 | 0.3 | |
Oxygen consumption | (VO2) | 6–8 | 3.2 | ml/kg/min |
Lung resistance | (R) | 20–30 | 3–4 | cm H2O/l/s |
Dynamic lung distensibility | (Cd) | 4–6 | 100–150 | ml/cm H2O |
Functional residual capacity | (FRC) | 20–30 | 34 | ml/kg |
Approaching the Newborn with Respiratory Disease
Differential diagnosis for RDS
Conatal pneumonia : Masculine sex, feverish mother, chorioamnionitis, premature labor, prolonged membrane rupture, prolonged labor, streptococcal maternal colonization, Guillain–Barré syndrome, tracheoesophageal fistula.
Meconium aspiration syndrome : (TTN) Amniotic fluid stained by meconium, fetal distress, post maturity, small for gestational age.
Transient tachypnea of the newborn: Cesarean section, fast labor, neonatal depression, maternal sedation.
Pneumothorax : History of resuscitation through manual ventilation.
Persistent pulmonary hypertension : (PPH) Meconium aspiration syndrome, neonatal depression, pneumonia, polycythemia, congenital diaphragmatic hernia, ingestion of aspirin or antiinflammatories, hyaline membrane disease, cold stress.
Maternal history : Health state before pregnancy and during previous pregnancies, prenatal care, prenatal ultrasound, family diseases, pregnancy diseases, drugs and medications, cause of hospital admittance, labor time, fetal state, amount of amniotic fluid (maturity, infection signs, meconium), bleeding, fetal distress, type of labor, approximate gestational age.
Newborn history : General condition at birth, need for resuscitation, Apgar score, vital signs, evaluation during transition period.
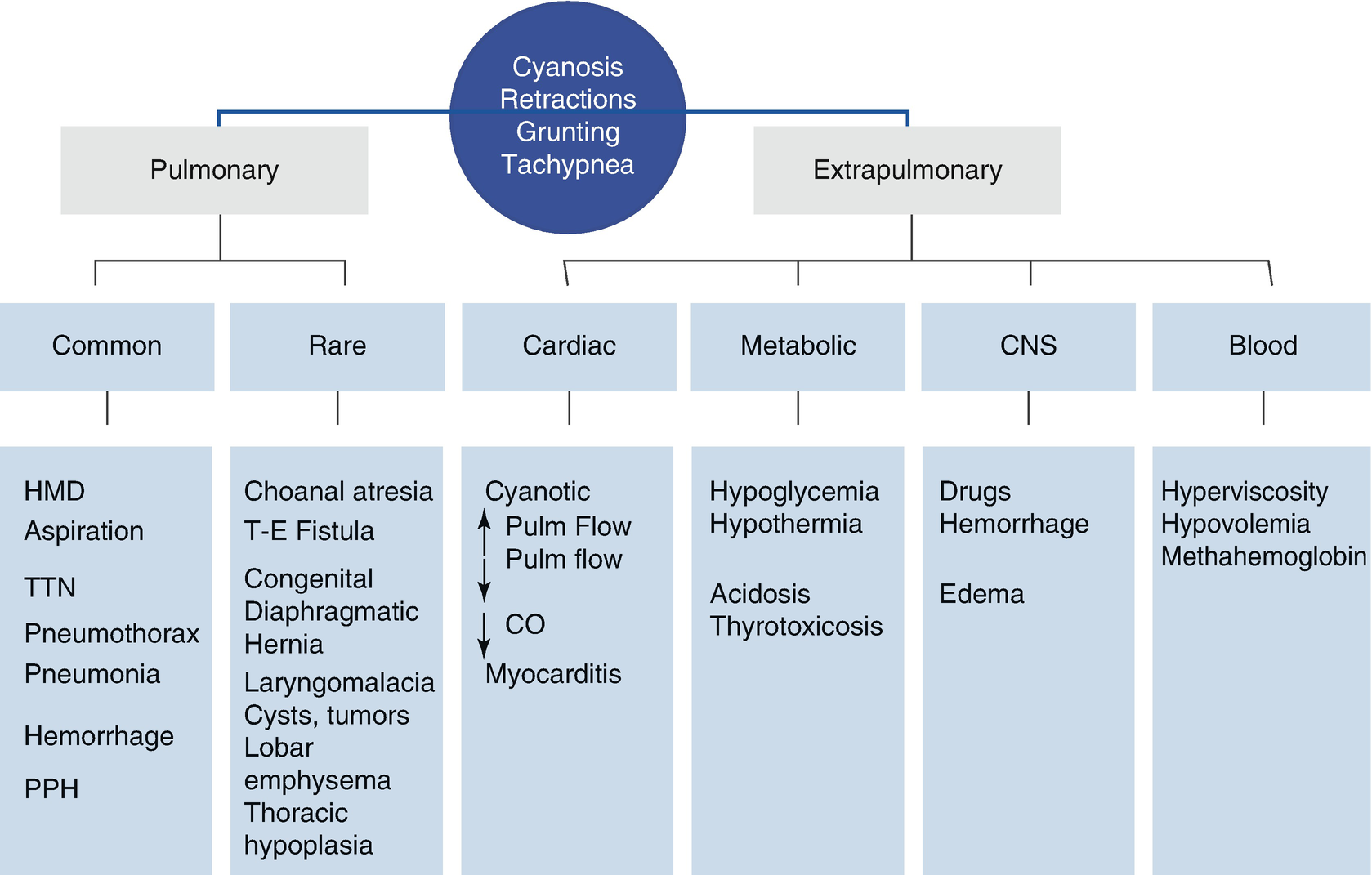
Physical examination : Nutritional state, presence and distribution of cyanosis. Acrocyanosis or distal cyanosis in feet and hands are common findings within the first days of life. However, central cyanosis is always abnormal, and it is evident when deoxygenated hemoglobin exceeds 3 g/dl, and this suggests the presence of hypoxemia. Cyanosis from crying is possible because a short circuit is caused by the Valsalva maneuver through the foramen ovale. Paleness may suggest shock, vasoconstriction, anemia, and obstruction of the cardiac outflow tract. Polycythemia may be suspected if the child looks plethoric; if the child has meconium stains, then meconium aspiration is suspected, and if there is exanthema or a bad smell, it must be considered that the cause of the breathing difficulty is a pneumonia. Nasal flaring shows the newborn’s need for air. The shape of a barrel chest suggests a volume increase, and a bell-shaped chest suggests a volume decrease (Table 36.3). Extremely preterm newborns (<1000 g) have a very compliant thoracic wall. During normal breathing a negative interpleural pressure is created, but it goes even further when the lung is sick, causing an evident intercostal and xiphoid retraction, with a tendency to collapse. This collapsing and protruding of the abdominal content, caused by the diaphragm moving downward, are the factors that cause “swing” or paradoxical breathing, which is typical of the severe breathing difficulty syndrome. Tachypnea is considered when the newborn has more than 60 breaths per minute and is the most sensible sign. Normal premature and term newborns will present a respiratory pattern called periodical breathing, which consists of shallow breaths followed by the cease of respiratory efforts or short apneas, which lasts from 5 to 10 s. It is important to notice the height of the tip of the heart, as it will be displaced if there are pulmonary masses, pneumothorax, or pulmonary hypoplasia. A scaphoid abdomen is typical of diaphragmatic hernias, where part of the abdominal content is placed in the thoracic cavity, which does not allow an adequate development of abdominal cavity, but it looks similar to the abdomen of a child who has eliminated meconium in the uterus. Abdomen distension can be seen when there is a tracheoesophageal fistula, especially when positive pressure has been used. If the belly button moves toward one side during inspiration or presents a “belly button dance” sign, it may be a sign of diaphragmatic paralysis in the side to which it is moving. When there is pulmonary hyperinsufflation , the liver and spleen can be easily palpated.
Causes of changes in thoracic volume
Bilateral | |
Volume increase | Transient tachypnea, meconium aspiration syndrome, pulmonary hypertension, cystic lung diseases |
Volume reduction | Hyaline membrane disease, pulmonary hypoplasia, thoracic wall restricted |
Unilateral | |
Low-volume disease | Atelectasis, unilateral pulmonary hypoplasia |
High-volume disease | Pneumothorax, unilateral interstitial emphysema, pulmonary cystic disease, Diaphragmatic disease, chylothorax |
Stridor suggests an obstruction of large airways. If the obstruction is extrathoracic, stridor will be greater at inspiration, although it can be heard in both inspiration and expiration when the obstruction is severe. Pulmonary murmur can be evaluated according to its intensity, length, symmetry, presence of crepitus, ronchi, or wheezing, although these alterations are less frequent in newborns.
Laboratory tests
Chest X-rays: Very useful in the differential diagnosis of respiratory and nonrespiratory diseases. Lateral and anteroposterior projections are essential for a good evaluation of pneumothorax, catheter position, and pleural tubes. Bones, soft tissues, and the visible portion of the abdomen must be systemically evaluated before focusing on the heart and lungs. Also, each chest X-ray film must be used to reevaluate the position of tubes and catheters because they usually migrate.
The trachea is easily curved because of its great flexibility, and it can even seem to have a mass effect, through its compression by other abnormal structures (Table 36.4).
Cell blood count and cultures: Infections must be actively sought, because of what a prompt treatment involves and also because of the difficulty of making a differential diagnosis, especially when differentiating from hyaline membrane disease.
Pulmonary function test: Initially it was only performed under investigative conditions, but today many ventilators are equipped with sensors that allow measuring this function. It is very useful to determine tidal volumes (if they are not increased) and pulmonary overdistension signs, which can contribute to neonatal lung damage.
Blood gases: One of the most useful tests to determine the physiopathology of the disease. It can also be used for treatment, as there are different goals, depending on the gestational age and the type of disease.
Hyperoxy test: Hypoxemia is considered when extrapulmonary short circuits from right to left are suspected (congenital heart disease and pulmonary hypertension). Oxygen is provided at 100% and gases are controlled. If the disease is pulmonary, PaO2 increases significantly.
General tests: Hematocrit must be controlled, because polyglobulic conditions may cause hypoxemia, and acute anemia may cause difficulties in starting spontaneous breathing during resuscitation. In every pathological process glycemia must be controlled because of the immaturity of the regulation systems, which is related to a greater energetic expenditure and reduced intake.
Common findings and variants in neonatal chest X-ray
Normal findings | Normal variants |
|---|---|
Uniform lung fields | Pleural fissures |
Less prominence of pulmonary hilums | Tracheal twisting and indentation |
8–9 ribs expansion | Mediastinal lines |
Tracheal deviation to the right | Pseudohyperlucid lung |
Air bronchogram | Apical or intercostal hernia |
Cardiac silhouette <60% of thorax | Radiolucency of the suprasternal space |
Classification of the Respiratory Problems of the Newborn
- I.
Respiratory problems caused by perinatal asphyxia.
- II.
Respiratory problems related to immaturity and lung liquid reabsorption.
- III.
Respiratory problems related to lung circulation. Respiratory problems conditioned by lung circulation diseases.
- IV.
Respiratory infections in the newborn: pneumonia.
- V.
Respiratory problems caused by congenital alterations of the airway and lungs.
Respiratory Problems Related to Perinatal Asphyxia
Cardiorespiratory Depression at Birth
As many as 10% of newborns requires some kind of support to start breathing spontaneously. It is crucial to anticipate this situation by determining which childbirths may produce depression at birth. Because of this, it is important to have at each childbirth at least one qualified person who may provide the initial resuscitation steps, and another person who may perform advanced resuscitation. The action flowchart is taught at the Neonatal Resuscitation Program, which is regulated by the American Academy of Pediatrics and the American Heart Association.
During childbirth the fetus may be exposed to periods of temporary hypoxia, caused by the decrease of the placenta blood flow. The fetus adapts to these periods by redistributing the blood flow to favor the brain, heart, and adrenal glands. During hypoxic periods, the respiratory system has adaptation mechanisms that are not efficient in either the fetus or the newborn: this is called paradoxical response to hypoxia. It happens when the fetus and newborns who have suffered hypoxia increase their respiratory rate and respiratory effort (tidal and minute volume increase), but this is transitory, and it rapidly progresses into apnea. Therefore, it is not uncommon to face a perinatal hypoxia sign consisting of no respiratory effort at birth, which will require resuscitation techniques to start spontaneous breathing. Depending on how long the fetus has been hypoxic, the apnea may be primary or secondary. Secondary apnea implies a greater time suffering hypoxia, wherein compensatory vascular mechanisms have been overwhelmed, and this is reflected in the fall of arterial pressure. When resuscitating a child with secondary apnea it is crucial to provide ventilation with effective positive pressure, and, less frequently, to use cardiac massage and drugs.
Perinatal Asphyxia and Respiratory Distress Syndrome Caused by Meconium Aspiration
Respiratory distress syndrome caused by aspiration of meconium is a common complication of perinatal asphyxia, and sometimes it is a serious one; this is frequently found in a postterm newborn. Its prevention depends on good control and perinatal management.
Intrauterine asphyxia stimulates gastrointestinal motility and the relaxation of the anal sphincter, which allows the meconium to enter the amniotic fluid, but this is uncommon before 37 weeks of gestation. If the fetus is younger than 34 weeks, the anal sphincter does not relax during asphyxia. Hypoxemia also causes the fetus to initiate deep breathing efforts, and so the fetus aspirates the amniotic fluid containing meconium. During birth the risk of meconium aspiration is greater, as a consequence of the first breaths. Meconium impacts different levels of the thinner airways, which causes an obstructive respiratory disease with entrapped air, and alteration of alveolar stability, along with its inflammatory reaction. Entrapped air is one of the causes of the high rate of pneumothorax in this disease. In almost 50% of the cases, respiratory failure is related and complicated by an important degree of pulmonary hypertension. Ventilatory mechanics are altered: airway resistance is increased, functional residual capacity is also increased because of the entrapped air, pulmonary distensibility is reduced, and there is compromise of the ventilation/perfusion ratio. The result is a respiratory distress situation with hypoxemia and hypercarbia.
Generally, the patient is a term or postterm newborn. Sometimes they are small considering their gestational age, with a history of perinatal asphyxia, which has been certified through the presence of meconium in the amniotic fluid, as well as alteration in the fetal heartbeat and cardiorespiratory depression at birth, which requires resuscitation. There can be meconium in the umbilical cord, and the skin of the newborn may have meconium impregnations. Polypnea and respiratory distress signs appear early: chest retraction, grunting, and nasal flaring. The thorax curves outward, with increased anteroposterior diameter. There is a noticeable cyanosis, which, at the beginning of the clinical presentation, usually responds to an increase in the oxygen inspired fraction, unless there is a serious pulmonary hypertension. During auscultation there can be a reduction of the pulmonary murmur and crackles. Other concomitant complications caused by asphyxia, and which may require specific treatment, must be investigated, such as hypoxic-ischemic encephalopathy, renal impairment, cardiogenic shock, and alterations of the coagulation process.
If the aforementioned clinical history and signs are considered, diagnosis is generally clear. The aim of the laboratory examinations is to corroborate the diagnose of meconium aspiration, evaluate the presence of other complications from asphyxia, and for follow-up.
Anteroposterior and lateral chest X-ray. X-rays will show irregular opacities as nodules or cords, following the distribution of the bronchial tree next to hyperinsufflation zones. The diaphragm is sometimes flat. It is important to rule out the presence of pneumothorax (Fig. 36.2).
Arterial gases. Arterial gases will show the degree of respiratory failure. These measures must be serially controlled every 48 h, as needed. This information will be key for delivering a prompt and adequate treatment, to evaluate its efficacy as well as the progression of the disease.
Cell blood count and blood culture. These tests are important to obtain hematocrit values and detect a possible infection. Meconium is a good culture medium.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


