Atopic march
From the physiopathological aspect, the syndromes are characterized by the capacity of the affected person to manifest an allergic hypersensitivity, whether it is mediated by IgE or not. This capacity has a strong genetic basis, which allows the person to respond to different antigens that are common environmental proteins.
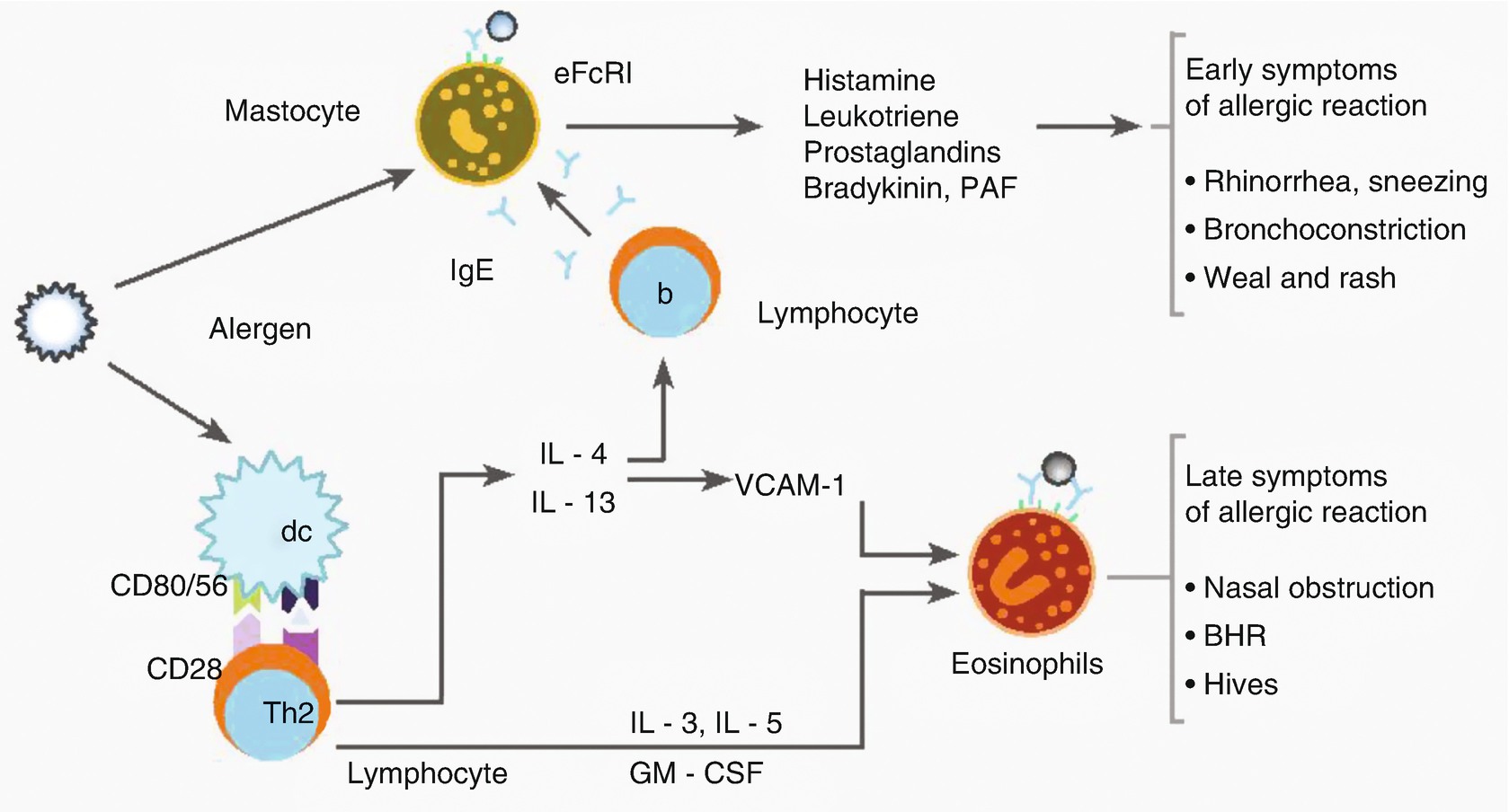
Allergic reaction
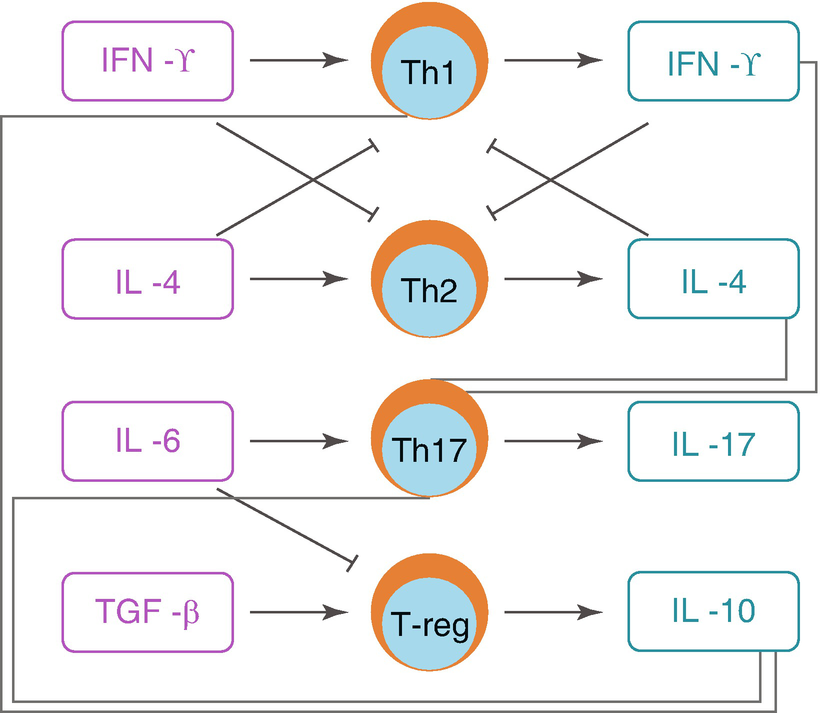
Interregulation among the different subgroups of T-CD4+ cells
Clinical Manifestations
Allergic diseases can appear at any time in the life of a child, and the clinical manifestation depends on the age of the patient. A chronological analysis of these manifestations follows.
Newborn Period
Allergic reactions in a child under 1 month old are very uncommon, and when they are present they can be FA (cow’s milk proteins) or AD, which are further analyzed in the infant stage section. During intrauterine life, in the maternofetal interface, the period of response to specific antigens begins between the fourth to seventh month of pregnancy. It has been confirmed that the fetus may produce specific IgE from the 11th week of intrauterine life. Reactivity to different allergens in the blood of the fetus is seen by week 22 of gestation, when IL-4 and INF-γ are already present. At 16–17 weeks, IL-10 predominates over INF-γ in the human amniotic fluid, which predisposes to a Th2 response. The tissues of the fetus that are more exposed to the antigens present in the amniotic fluid are the skin and the intestine, and secondarily the respiratory system, which would explain why the first allergic manifestations of extrauterine life are in these organs.
Infant Period
As already mentioned, FA and AD are the earliest manifestations of allergies, constituting the first clinical elements that allow us to suspect atopy in a patient. At 2 years old, 50% of the atopic patients present with symptoms of FA and AD, and at 5 years old, 60% of them; in this same age group, 40% of the atopic patients have symptoms of BA and 25% of AR.
FA has an early onset during the first months of life, beginning an important decrease, depending on the problematic food, between 2 and 3 years old. Its prevalence is greater during the first years of life, around 6% in patients who are under 3 years old. It is infrequent in patients over 5 years old, and its frequency continues to be low until adolescence.
FA is the immunological reaction mediated by IgE or another hypersensitivity mechanism to one or more components of a food, and it must be differentiated from the adverse reactions to certain foods, which is the abnormal clinical response caused by some food or additive, caused by nonimmunological mechanisms. Its clinical manifestations are characterized by a wide variety of symptoms and signs, which may be localized or systemic. In infants the most common signs are irritability and gastrointestinal symptoms, such as nausea, vomiting, recurring abdominal pain such as colic, diarrhea, and eventually blood in the stools. It may be present along a stationary growth curve, or show weight loss, in most severe cases. The foods most likely to cause food allergy are the following.
Milk: Milk contains several potentially allergen proteins, and the manifestations of the allergy are presented in about 2.5% of infants; about 85% achieve tolerance when the patient is between 3 and 5 years old. These patients have more than 50% of possibilities to develop other allergies, and more than 80% of chances of developing allergies to inhaled allergens later in life.
Egg: The manifestation frequency of egg allergy in infants is estimated as 2.5%; it contains the most allergen proteins, mainly in the egg white, and its tolerance is achieved around the third year of life. As happens with milk, sensitization to egg is related to an increased risk of developing allergies to inhaled allergens.
Peanut: In countries where the consumption of peanut begins early (incorporated into other foods or as butter), an allergy frequency of 0.6% is reported, and this tends to last during several years, or even for the lifetime. Its tolerance is described as less than 20% at the second year of life.
Less frequent: Soy (0.3–0.4%), wheat, fish, fruits, and vegetables, which are more frequent later in life and during adulthood.
Allergy to cow’s milk generally remits at the third year of life, and allergy to egg usually remits before puberty, although if it severe it may last for the lifetime. Allergies to fish, crustaceans, nuts, and peanuts may not totally improve, but they can be less severe later in life.
AD is a recurrent chronic skin disease characterized by reddish lesions, intense pruritus, and usually patches of dry skin in different parts of the body. These lesions usually present at first in the cheeks, and after that they may expand to the forehead, ears, scalp, chest, genitals, and limbs. Later in life the lesions tend to be drier and to be located in skin folds (retroauricular fold, neck, wrists, cubital fossa, and popliteal fossa). Atopy in the family background may or may not be present. Food allergy to the aforementioned foods is one of the frequent causes of AD. The NICE clinical guide includes the signs for its clinical diagnosis, diagnostic criteria, and evaluation of degree of seriousness.
Different follow-up prospective studies have determined the risk factor these pathologies may have in the posterior development of BA or AR. So, if an infant with AD at 3 months has the background of one of the parents or a sibling having atopy, this patient has a more than 50% chance of presenting BA when he is 5–6 years old and about 75% of suffering from this disease during the school years.
AR and AB , along with anaphylaxis, are less common symptoms in infants. Even though they can be present in infants, these symptoms tend to appear later in life.
Asthma predictive index (API)
Original APIa | Modified APIb |
|---|---|
Major criteria | Major criteria |
Asthma family history | Asthma family history |
Medical diagnosis of AD | AD |
Sensitizing to (Björkstén 1999) 1 air allergen | |
Minor criteria | Minor criteria |
AR medical diagnosis | Sensitivity to milk, peanut, or egg |
Wheezing without flu | Wheezing without flu |
Hematic eosinophilia (Björkstén 1999), 4% | Hematic eosinophilia (Björkstén 1999), 4% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


