Diffuse Tracheobronchial Wall Thickening
Jeffrey P. Kanne, MD
DIFFERENTIAL DIAGNOSIS
Common
Tracheal Neoplasms
Acute Bronchitis
Chronic Bronchitis
Less Common
Relapsing Polychondritis
Wegener Granulomatosis
Amyloidosis
Sarcoidosis
Rare but Important
Laryngeal Papillomatosis
Tracheopathia Osteochondroplastica
Rhinoscleroma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Diffuse or focal abnormality
Involvement or sparing of posterior tracheal membrane
Expiratory CT useful for detecting tracheomalacia
Helpful Clues for Common Diagnoses
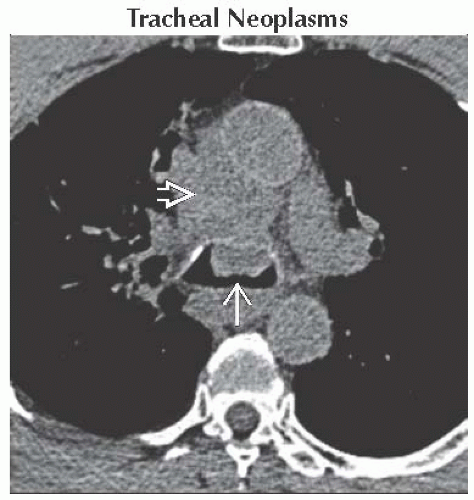
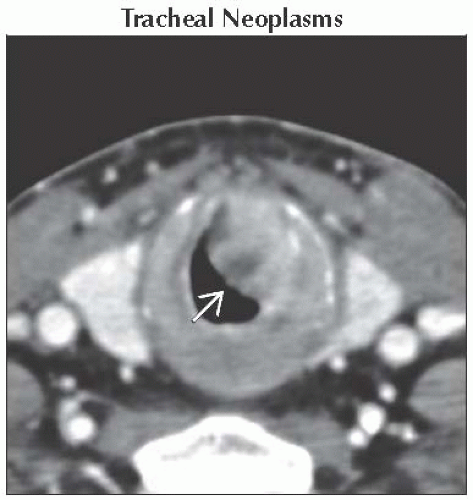
Tracheal Neoplasms
Uncommon
< 1% of all lower respiratory tract neoplasms
Squamous cell carcinoma and adenoid cystic carcinoma account for > 80%
Other tumor types rare
Polypoid intraluminal mass most common appearance
Squamous cell carcinomas often large at presentation (up to 4 cm)
Eccentric nodular wall thickening or diffuse tracheal wall infiltrating uncommon
Frequently extend into mediastinum and adjacent structures
Tracheoesophageal fistula in 15%
Main bronchial invasion in 25%
Regional lymph node metastases common
Adenoid cystic carcinomas most commonly occur near tracheal carina
Acute Bronchitis
Viral most common cause
Bronchial wall thickening
Retained secretions
Patchy atelectasis
Peribronchial consolidation may indicate bronchopneumonia
Acute bacterial tracheitis
Most common in children
Less commonly immunocompromised adults
Diffuse tracheal wall edema
Edema of surrounding mediastinal tissues
Chronic Bronchitis
Related to cigarette smoking
Clinical diagnosis
Tracheobronchial wall thickening
No significant stenosis
Retained secretions
Centrilobular pulmonary emphysema may be present
Helpful Clues for Less Common Diagnoses
Relapsing Polychondritis
Involves only cartilaginous portions of trachea and main bronchi
Spares posterior membrane
Increased attenuation of tracheal wall
May become diffusely calcified
Smooth tracheal wall thickening
Tracheal stenosis
Occurs in 33-89% of patients
Diffuse or focal
Associated with bronchial narrowing
Tracheomalacia
Result of cartilaginous inflammation and destruction
Suggested by > 70% reduction of cross-sectional area on expiration
Wegener Granulomatosis
Tracheal wall thickening in 15%
Bronchial wall thickening in 50-60%
Focal > diffuse
Subglottic narrowing most common
Tracheobronchial narrowing smooth or irregular
Associated lung findings may be present
Nodules and masses
Cavitary lesions
Consolidation
Ground-glass opacity
Amyloidosis
Tracheobronchial tree most commonly affected
Smooth or nodular calcification in up to 50%
Circumferential tracheal or tracheobronchial wall thickening
Associated lung findings (from airway obstruction)
Atelectasis or obstructive pneumonitis
Pulmonary amyloid
Sarcoidosis
Tracheal involvement very uncommon
Larynx often affected
Stenosis smooth, irregular, nodular, or mass-like
Other typical findings usually present
Lymphadenopathy
Perilymphatic nodules
Helpful Clues for Rare Diagnoses
Laryngeal Papillomatosis
Tracheobronchial involvement in 5-10%
Usually develops 10 years after laryngeal disease
May affect lungs
Nodules
Cavitary lesions
Degeneration into squamous cell carcinoma rare
Tracheopathia Osteochondroplastica
Mild diffuse tracheobronchial stenosis with nodularity
Calcified nodules arising from tracheal cartilage protruding into lumen
Range in size from 3-8 mm
Lower trachea most commonly involved
May extend into bronchi to segmental level
Can cause atelectasis
Sparing of posterior tracheal membrane characteristic
Often associated with “saber-sheath” tracheal deformity
Slowly progressive
Older men with chronic obstructive lung disease most commonly affected
Rhinoscleroma
Slowly progressive granulomatous infection caused by Klebsiella rhinoscleromatis
Endemic in tropical and subtropical regions
Upper respiratory tract most commonly involved
Especially nose, upper lip, hard palate, and maxillary sinuses
Trachea and proximal bronchi affected in up to 10%
Thickening of trachea and main bronchi with luminal stenosis
Stenoses usually concentric
Smooth or nodular
Diffuse uniform narrowing uncommon
Occasional mediastinal and hilar lymphadenopathy
Atelectasis and obstructive pneumonitis may develop
Image Gallery
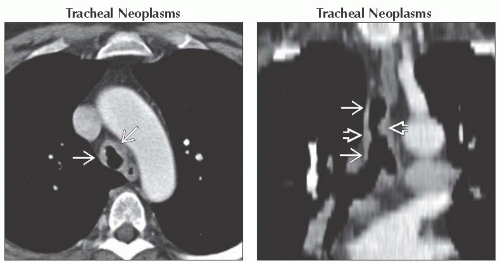 (Left) Axial CECT shows nodular thickening of the tracheal wall
 in this patient with adenoid cystic carcinoma. Following resection, adenoid cystic carcinomas, while lower grade than squamous cell carcinoma, often recur because of submucosal growth. (Right) Coronal oblique CT reconstruction shows tracheal wall thickening in this patient with adenoid cystic carcinoma. Following resection, adenoid cystic carcinomas, while lower grade than squamous cell carcinoma, often recur because of submucosal growth. (Right) Coronal oblique CT reconstruction shows tracheal wall thickening  with nodular protrusions into the tracheal lumen with nodular protrusions into the tracheal lumen  in this patient with adenoid cystic carcinoma. in this patient with adenoid cystic carcinoma.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|