Patients with repaired pulmonary stenosis (PS) or tetralogy of Fallot (TOF) both develop pulmonary regurgitation (PR) leading to right ventricular (RV) dilatation and dysfunction. We aimed to characterize differential effects of chronic PR in these populations. Patients with surgically repaired PS were matched 1:2 by age and PR fraction with patients with TOF. Patients with previous pulmonary valve replacement were excluded. Cardiovascular magnetic resonance data were compared; peak longitudinal and circumferential systolic strain by feature tracking were compared to evaluate differential contribution of the RV sinus and outflow tract, respectively. PS (n = 24, 41 ± 13 years old) and TOF (n = 47, 39 ± 13 years old) patients did not differ in RV end-diastolic volume (153 ± 45 vs 154 ± 45 ml/m 2 , p = 0.99) or diastolic function. However, patients with PS had preserved RV ejection fraction (54.3 ± 4.4% vs 48.0 ± 7.1%, p <0.0001). Differences were greater in RV circumferential (−15.8 ± 3.3 vs −11.8 ± 3.4, p <0.0001) than longitudinal strain (−18.0 ± 3.8 vs −15.9 ± 3.8, p = 0.04), with particular decrease in the infundibulum (−17.4 ± 7.5 vs −6.8 ± 6.3, p <0.0001). Late gadolinium enhancement in the RV outflow tract was more frequent in patients with TOF (70.2% vs 45.8%, p = 0.001). In conclusion, surgical repair of PS leads to similar RV dilatation and diastolic dysfunction compared to patients with TOF, but differential effects on ventricular systolic function, largely related to differences in the outflow tract. With different patterns of scarring and ventricular remodeling, further study is needed to clarify whether criteria for pulmonary valve replacement in patients with PS should differ from those with TOF.
Pulmonary stenosis (PS) is a common congenital cardiac defect, which can be treated through surgical pulmonary valvotomy or balloon valvuloplasty, often resulting in pulmonary regurgitation (PR) and subsequent right ventricular (RV) dilatation. Surgical repair of tetralogy of Fallot (TOF), the most common cyanotic congenital heart lesion, also typically results in significant PR, which is associated with long-term morbidity and mortality secondary to heart failure, arrhythmia, and sudden cardiac death. Cardiac magnetic resonance (CMR) is a vital tool in determining timing of pulmonary valve replacement (PVR) after repair of TOF. However, few data exist for patients with PS, and it is unclear whether they demonstrate the same degree of RV dilatation and dysfunction in response to chronic PR, and thus, whether guidelines for PVR in patients with TOF may apply to this population. We aimed to characterize long-term changes in ventricular size and function in patients with PS, compared to those with TOF with similar degrees of PR.
Methods
A retrospective chart review was performed for all patients with valvar PS status after surgical pulmonary valvotomy, pulmonary valvectomy, or RV transannular patch augmentation, who underwent clinically indicated CMR at the University of Michigan from 2007 to 2013, and were aged ≥18 years at the time of CMR. Patients were excluded if they had undergone PVR (surgical or transcatheter) before CMR, placement of a right ventricle to pulmonary artery conduit, balloon pulmonary valvuloplasty as initial therapy, or other cardiac catheterization interventions to relieve RV outflow tract (RVOT) obstruction. This study was approved by the University of Michigan Institutional Review Board, and requirement for informed consent for this retrospective study was waived.
Patients with TOF who underwent clinically indicated CMR from 2007 to 2013 after initial surgical repair were frequency-matched 2:1 with patients with PS on the basis of pulmonary regurgitant fraction (0 to 19, 20 to 40, >40%) and age at the time of CMR (18 to 30, 31 to 50, and >50 years). Similar to patients with PS, those with TOF were excluded if they had undergone PVR (surgical or transcatheter) before CMR or had placement of a right ventricle to pulmonary artery conduit. Patients with pulmonary atresia or absent pulmonary valve, or with other significant associated cardiac defects (e.g., atrioventricular septal defect) were excluded.
CMR was performed using a commercially available 1.5 T scanner (Intera Achieva or Ingenia; Philips, Best, The Netherlands). Cine images were obtained with a breath-hold, vectorcardiographic-gated, segmented k-space, steady-state free precession sequence. Left ventricular and right ventricular end-diastolic volume (RVEDV) and end-systolic volume were measured in the short-axis plane by consensus of 2 readers, using commercially available software (QMass; Medis, Leiden, The Netherlands). Volumes were indexed to body surface area and compared with normative data. PR was measured from a free-breathing, through-plane velocity-encoded phase contrast sequence orthogonal to the main pulmonary artery. PR fraction was defined as the ratio of regurgitant flow to total forward flow.
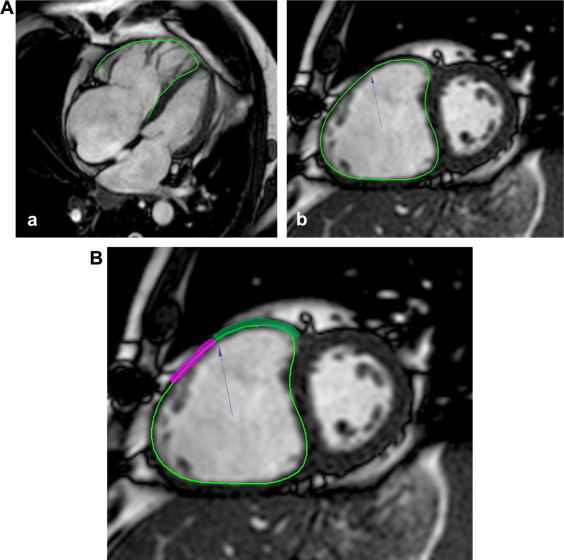
To differentiate the relative contribution of the RVOT and RV sinus in RV dysfunction, RV peak longitudinal systolic strain and RV peak circumferential strain ( Figure 1 ) were measured by a single observer blinded to volumetric data, using feature tracking software (Cardiac Performance Analysis; TomTec, Unterschleissheim, Germany). RV circumferential and longitudinal strain measurements by feature tracking have been validated against speckle tracking echocardiography in patients with TOF and related to exercise capacity. Longitudinal strain was measured from a 4-chamber slice, to evaluate the RV sinus. Circumferential strain was measured from the most basal short-axis slice with circumferential RV myocardium, to incorporate the RVOT. Points were manually selected along the endocardial contour, with subsequent automated tracking. Contours were visually evaluated for adequate tracking and redrawn as necessary. To further localize differences, segmental circumferential strain was measured at the superior aspect of the RVOT, and the superior aspect of the RV free wall ( Figure 1 ).
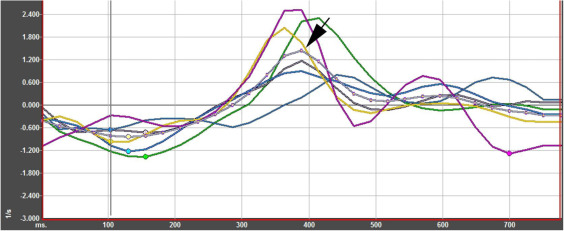
RV diastolic function was evaluated by the presence of end-diastolic forward flow (EDFF) in the main pulmonary artery and by measurement of peak early diastolic longitudinal strain. EDFF was considered present if there was anterograde flow on phase contrast imaging in the main pulmonary artery in end diastole before the onset of systolic anterograde flow. Peak early diastolic longitudinal strain rate was measured from a 4-chamber slice with feature tracking software ( Figure 2 ).
Late gadolinium enhancement (LGE) was performed with breath-hold phase-sensitive inversion recovery in the 4-chamber and short-axis planes, 12 to 15 minutes after administration of 0.2 mmol/kg of gadoteridol (ProHance; Bracco, Monroe Township, New Jersey) or gadopentetate dimeglumine (Magnevist; Bayer, Leverkusen, Germany). The presence of LGE was qualitatively evaluated by an experienced reader and included LGE in any portion of the right ventricle excluding the superior or inferior insertion points of the interventricular septum.
Residual RVOT obstruction was quantified from echocardiograms performed closest to the time of CMR within a 6-month period. Peak instantaneous pressure gradient was dichotomized as <20 or ≥20 mm Hg.
Data are presented as frequency (percentage) for categorical variables and mean ± SD or median (interquartile range) as appropriate for continuous variables. Demographics and CMR and echocardiographic measurements were compared between patients with PS and those with TOF using the chi-square test for categorical variables and t test or Wilcoxon rank-sum test for continuous variables. A p value <0.05 was considered statistically significant.
Results
Of a total of 45 patients with PS who underwent CMR during the study period, 24 patients (53.3%) were included in the analysis; 12 patients who underwent balloon angioplasty rather than surgical intervention and 9 patients who underwent PVR before CMR were excluded. There was no significant difference between patients with PS and TOF in age at the time of initial repair, time from initial repair to CMR, body surface area, or body mass index ( Table 1 ). Multiple patients in both groups had small atrial septal defects that did not require intervention. No patients had significant genetic abnormalities. Although both groups had little residual RVOT obstruction, the median peak gradient on echocardiogram was smaller in the patients with PS (6.5 vs 16.5 mm Hg, p = 0.0004). More TOF patients had a residual gradient of ≥20 mm Hg (38.3% vs 8.3%, p = 0.01). In 2 patients with TOF, phase contrast data could not be obtained.
| Characteristics | PS (n = 24) | TOF (n = 47) | p-value |
|---|---|---|---|
| Age at CMR (years) | 40.7 ± 13.3 | 39.1 ± 12.5 | 0.61 |
| Age at repair (years) | 3.5 (1.5-7) | 5 (2-9) | 0.47 |
| Type of repair | |||
| Commissurotomy | 2 (8.3%) | 1 (2.1%) | N/A |
| Trans-annular Patch | 4 (16.7%) | 40 (85.1%) | |
| Valvectomy | 4 (16.7%) | 0 | |
| Valvotomy | 14 (58.3%) | 1 (2.1%) | |
| Unknown/missing | 0 | 5 (10.6%) | |
| Time from repair to CMR (years) | 34.2 ± 8.7 | 33.5 ± 9.3 | 0.75 |
| Male sex | 10 (41.7%) | 26 (55.3%) | 0.28 |
| Weight (kg) | 68.0 ± 15.2 | 76.3 ± 22.0 | 0.10 |
| Height (cm) | 167.3 ± 11.3 | 167.7 ± 11.7 | 0.90 |
| Body Mass Index (kg/m 2 ) | 24.1 ± 4.4 | 26.9 ± 6.1 | 0.06 |
| Body surface area (m 2 ) | 1.77 ± 0.24 | 1.87 ± 0.31 | 0.16 |
There was no difference in indexed RVEDV or RVEDV z-score between the 2 groups and no difference in RV diastolic function ( Table 2 ).
| Measurement | PS (n = 24) | TOF (n = 47) | p-value |
|---|---|---|---|
| Regurgitant fraction (%) | 41.5 ± 17.1 | 40.9 ± 16.3 | 0.89 |
| Right ventricular end-diastolic volume (ml/m 2 ) | 153.3 ± 44.8 | 153.5 ± 44.9 | 0.99 |
| Right ventricular end-diastolic volume (Z-score) | 5.26 ± 3.07 | 5.17 ± 3.18 | 0.91 |
| End-diastolic Forward Flow | |||
| Present | 20 (83.3%) | 29 (61.7%) | 0.10 |
| Absent | 4 (16.7%) | 16 (34.0%) | |
| Unknown | 0 | 2 (4.3%) | |
| Right ventricular longitudinal diastolic strain rate | 1.27 ± 0.35 | 1.13 ± 0.37 | 0.13 |
Right ventricular ejection fraction (RVEF) was higher in patients with PS than in those with TOF, with a trend toward higher left ventricular ejection fraction ( Table 3 ). Differences in RV strain were greater for circumferential than longitudinal strain, with marked difference in the RVOT and RV free wall. LGE was more common in patients with TOF than in those with PS, particularly in the RVOT (70.2% vs 45.8%, p = 0.001).



