Diastolic Murmurs
ANATOMY AND PHYSIOLOGY
At the end of ventricular systole and the beginning of diastole, the aortic and pulmonic valves close. During this time, the A2-P2 interval can usually be auscultated. After a brief period of isovolumic relaxation, the mitral and tricuspid valves open, and blood flows from the atria into the ventricles. During this early filling period, a third heart sound (S3)—which sounds like “Ken-Tuc-Key”—can sometimes be heard in healthy individuals younger than age 20. Late in diastole, the atria contract, increasing blood flow into the ventricles. Occasionally, a fourth heart sound can be heard during this late filling period. Except for these brief heart sounds, diastole is normally silent. When diastolic murmurs occur, they are heard between the second and first heart sounds (S2 and S1) or between the end of the T wave and the beginning of the QRS complex on the electrocardiogram (ECG) waveform.
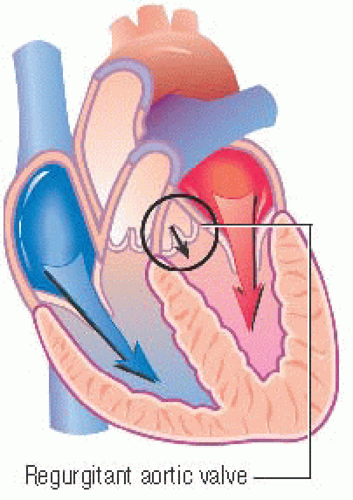
The regurgitation of blood through the aortic and pulmonic valves may cause diastolic murmurs. Because both valves close at the beginning of diastole, murmurs produced by dysfunctional aortic and pulmonic valves begin early in diastole, immediately after the affected valve closes.
Mitral and tricuspid valve stenosis and conditions that produce turbulent blood flow across normal mitral or tricuspid valves also cause diastolic murmurs. Because these valves open after a period of isovolumic relaxation, these murmurs are heard during mid-diastole.
AORTIC REGURGITATION MURMURS
Early diastolic aortic regurgitation murmurs
The early diastolic aortic regurgitation murmur, also called aortic insufficiency, can result from rheumatic heart disease, Marfan syndrome, osteogenesis imperfecta, a congenital bicuspid valve, or
a dissecting aortic aneurysm. Leakage around a prosthetic aortic valve can also produce this murmur.
a dissecting aortic aneurysm. Leakage around a prosthetic aortic valve can also produce this murmur.
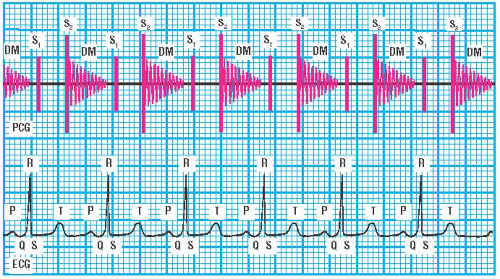 PCG and ECG showing early diastolic aortic regurgitation murmur |
Because the aortic pressure normally exceeds the left ventricular pressure at the beginning of diastole, it forces a retrograde, or backward, flow of blood across an incompetent aortic valve. The turbulent blood flow produces the murmur. In this murmur, A2 may sound normal, or it may be accentuated if the patient has severe systemic hypertension. (♦Sound 38) This murmur is commonly associated with a systolic ejection murmur produced by increased left ventricular stroke volume.
Sound characteristics
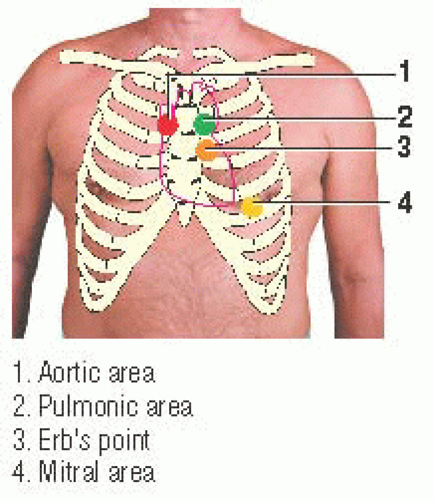
The early diastolic aortic regurgitation murmur is usually heard best near the heart’s base over the aortic and pulmonic areas, over Erb’s point, and near the heart’s apex over the mitral area. Because of its usually soft intensity, it’s heard best in a quiet environment. The murmur can last throughout most of diastole. It has a high pitch that’s heard best using the diaphragm of the stethoscope, and it has a blowing or musical quality. Its timing is diastolic, beginning with A2. On the ECG waveform, the murmur begins after the T wave and ends just before the QRS complex. It has a decrescendo configuration. (♦Sound 38)
If aortic regurgitation is associated with aortic root dilation or with a dissecting aneurysm of the ascending aorta, the diastolic murmur may be louder along the right sternal border between the second and fourth intercostal spaces than along the left sternal border between the second and fourth intercostal spaces, respectively. If the patient is elderly or has chronic obstructive pulmonary disease, the murmur may be heard best near the heart’s
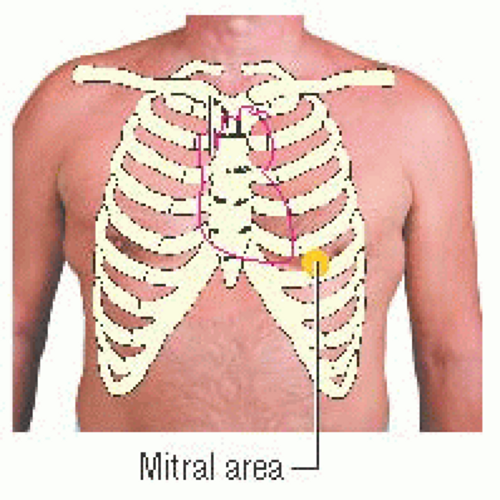
apex over the mitral area. If the murmur is loud, it may be heard over most of the precordium.
apex over the mitral area. If the murmur is loud, it may be heard over most of the precordium.
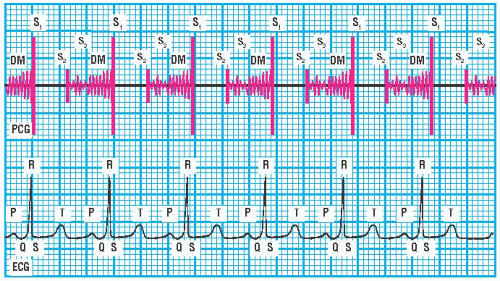 PCG and ECG showing middiastolic aortic regurgitation (Austin Flint) murmur |
Enhancement techniques
This murmur can be enhanced by having the patient sit down, lean forward, and hold his breath after expiration or perform maneuvers that increase aortic diastolic pressure, such as squatting or performing the handgrip exercise.
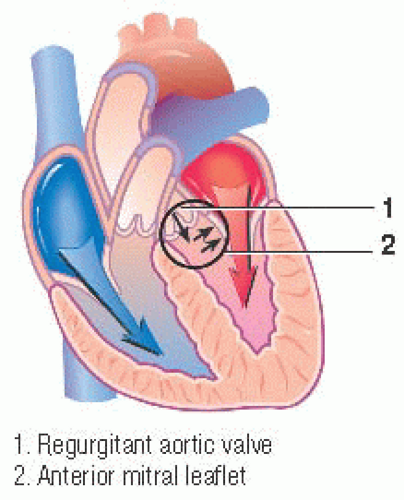
Middiastolic aortic regurgitation (Austin Flint) murmurs
Severe aortic regurgitation may be associated with a middiastolic and presystolic rumbling murmur. This murmur is caused by the aortic regurgitant jet impinging on the normal mitral inflow and augmenting mitral inflow turbulence. The murmur generated by the turbulent blood flow across the mitral valve is called an Austin Flint murmur; it may be confused with a murmur of mitral stenosis. (♦Sound 39)
Sound characteristics
The Austin Flint murmur is usually heard best near the heart’s apex over the mitral area. It’s introduced with an S3 rather than an opening snap (OS), as occurs in mitral stenosis. Its intensity is usually soft. It has a low pitch that’s heard best using the bell of the stethoscope. The murmur has a rumbling quality. Its timing is confined to middiastole or presystolic. It’s heard just before the QRS complex on the ECG waveform. The murmur has a presystolic crescendo configuration; its middiastolic component has a crescendo-decrescendo configuration. (♦Sound 39)
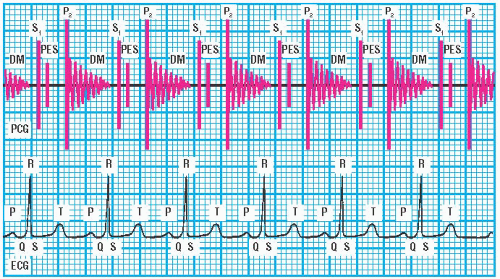 PCG and ECG showing Graham Steell murmur |
PULMONIC REGURGITATION MURMURS
Graham Steell murmurs
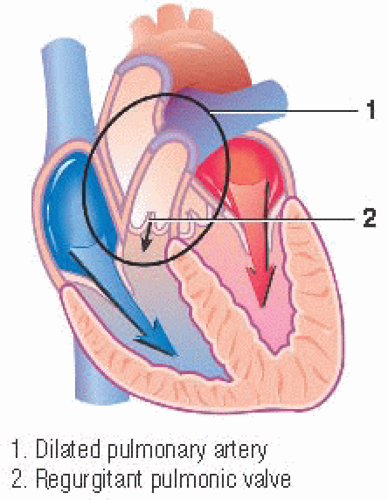
Because the pulmonary artery pressure is normally quite low during diastole, significant regurgitation from a normal pulmonic valve rarely occurs without pulmonary hypertension. Pulmonary hypertension produces pulmonary artery dilation and a relative pulmonic insufficiency because of dilation of the pulmonic valve ring. (♦Sound 40) A pulmonic regurgitation murmur resulting from pulmonary hypertension is called a Graham Steell murmur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree