Diagnostic Tests and Procedures
Advances in diagnostic testing allow for earlier and easier diagnosis and treatment of cardiovascular disorders. For example, in some patients, echocardiography, a noninvasive and risk-free test, can provide as much diagnostic information about valvular heart disease as cardiac catheterization, an invasive and high-risk test. Monitoring and testing also help guide and evaluate treatment and identify complications. Before the patient undergoes testing, explain the procedure in terms he can easily understand. Make sure an informed consent form is signed, if necessary. Because these diagnostic tests may cause anxiety, be sure to provide emotional support.
Cardiac tests range from a relatively simple test that analyzes the patient’s blood for cardiac enzymes, proteins, and clotting time to very sophisticated imaging and radiographic tests that reveal a detailed image of the heart. Other cardiovascular tests include various forms of electrocardiography, ultrasound, and hemodynamic monitoring.
CARDIAC ENZYMES AND PROTEINS
Analyzing cardiac enzymes and proteins (markers) is an important step in diagnosing acute myocardial infarction (MI) and in evaluating other cardiac disorders. After an MI, damaged cardiac tissue releases significant amounts of enzymes and proteins into the blood. Specific blood tests help reveal the extent of cardiac damage and help monitor healing progress.
Creatine kinase and isoforms
Creatine kinase (CK) is present in heart muscle, skeletal muscle, and brain tissue. Its isoenzymes, CK-MB, is found specifically in the heart muscle. Elevated levels of CK-MB reliably indicate acute MI. Generally,
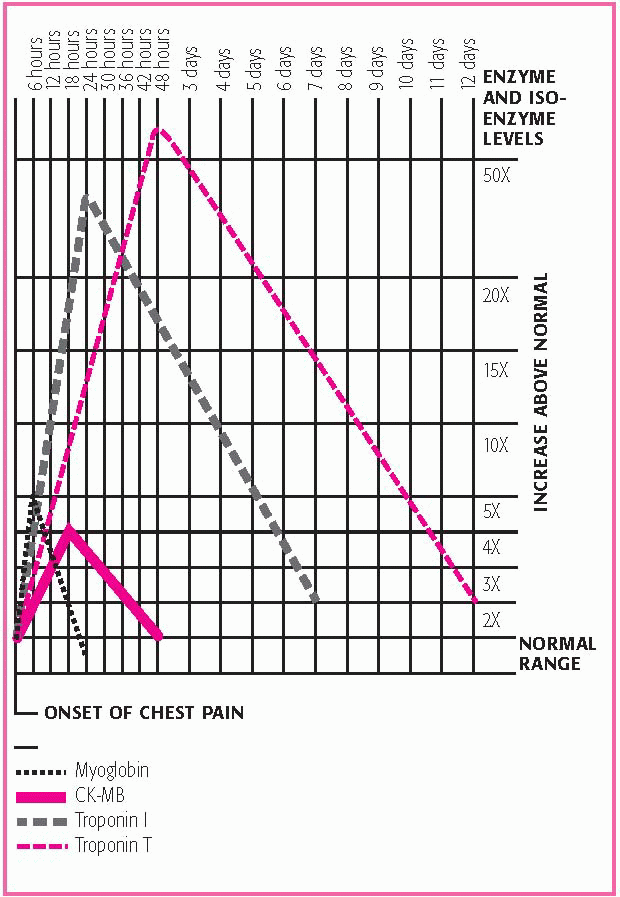
CK-MB levels rise 4 to 8 hours after the onset of an acute MI, peak after 20 hours, and may remain elevated for up to 72 hours. (See Cardiac enzyme and protein patterns.) Normal CK levels are 55 to 170 units/L for men and 30 to 135 units/L for women. CK-MB levels are normally less than 5% for men and women.
CK-MB levels rise 4 to 8 hours after the onset of an acute MI, peak after 20 hours, and may remain elevated for up to 72 hours. (See Cardiac enzyme and protein patterns.) Normal CK levels are 55 to 170 units/L for men and 30 to 135 units/L for women. CK-MB levels are normally less than 5% for men and women.
NURSING CONSIDERATIONS
Explain to the patient that the test will help confirm or rule out MI.
Inform the patient that blood samples will be drawn at timed intervals.
Muscle trauma caused by I.M. injections, cardioversion, or cardiopulmonary resuscitation can raise CK levels.
Patients who are muscular may have significantly higher CK levels.
Handle the collection tube gently to prevent hemolysis, and send the sample to the laboratory immediately after collection.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
Myoglobin
Myoglobin, which is normally found in skeletal and cardiac muscle, functions as an oxygen-bonding muscle protein. It’s released into the bloodstream when ischemia, trauma, and inflammation of the muscle occur. Normal myoglobin values are 0 to 0.09 mcg/ml.
Rising myoglobin levels are one of the first markers of cardiac injury after an acute MI. Levels may rise within 2 hours, peak within 4 hours, and return to baseline by 24 hours. However, because skeletal muscle damage may also cause myoglobin levels to rise, other tests (such as CK-MB or troponin) may be required to determine myocardial injury.
NURSING CONSIDERATIONS
I.M. injections, recent angina, or cardioversion can cause elevated myoglobin levels.
Handle the collection tube gently to prevent hemolysis, and send the sample to the laboratory immediately after collection.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
Troponin I and troponin T
Troponin is a protein found in skeletal and cardiac muscles. Two isotypes of troponin, troponin I and troponin T, are found in the myocardium. When injury occurs to the myocardial tissue, these proteins are released into the bloodstream. Troponin T can also be found in
skeletal muscle. Troponin I, however, is found only in the myocardium. In fact, it’s more specific to myocardial damage than CK, CK-MB isoenzymes, and myoglobin. Because troponin T levels can occur in certain muscle disorders or renal failure, they’re less specific for myocardial injury than troponin I levels.
skeletal muscle. Troponin I, however, is found only in the myocardium. In fact, it’s more specific to myocardial damage than CK, CK-MB isoenzymes, and myoglobin. Because troponin T levels can occur in certain muscle disorders or renal failure, they’re less specific for myocardial injury than troponin I levels.
CARDIAC ENZYME AND PROTEIN PATTERNS
Because they’re released by damaged tissue, serum proteins and isoenzymes (catalytic proteins that vary in concentration in specific organs) can help identify the compromised organ and assess the extent of damage. After acute myocardial infarction, cardiac enzymes and proteins rise and fall in a characteristic pattern, as shown in this graph.
 |
Normal troponin I levels are less than 0.35 mcg/L and normal troponin T levels are less than 0.1 mcg/L. Troponin I levels greater than 2 mcg/L suggest cardiac injury.
Troponin levels rise within 3 to 6 hours after myocardial damage. Troponin I peaks in 14 to 20 hours, with a return to baseline in 5 to 7 days, and troponin T peaks in 12 to 24 hours, with a return to baseline in 10 to 15 days. Because troponin levels stay elevated for a prolonged time, they can detect an infarction that occurred several days earlier. Troponin T levels can be determined at the bedside in minutes, making them a useful tool for determining treatment in acute MI.
NURSING CONSIDERATIONS
Inform the patient that he need not restrict food or fluids before the test.
Tell the patient that multiple blood samples may be drawn.
Sustained vigorous exercise, cardiotoxic drugs such as doxorubicin, renal disease, and certain surgical procedures can cause elevated troponin T levels.
Handle the collection tube gently to prevent hemolysis, and send the sample to the laboratory immediately after collection.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
Ischemia modified albumin
The ischemia modified albumin (IMA) test measures the changes in human serum albumin when it comes in contact with ischemic tissue. When ischemia occurs, IMA will rise rapidly. In over 80% of patients with acute coronary syndrome, IMA has been found to be elevated. However, IMA doesn’t rise in tissue necrosis.
Normally, there’s no IMA found in the blood. Increases in IMA are seen within 15 minutes of the onset of ischemia. This is significantly earlier than any other cardiac marker. When the ischemic event is resolved, IMA levels return to normal within several hours. The IMA test is used in conjunction with other cardiac markers, such as troponin, and an electrocardiogram (ECG). If the IMA test is negative and the troponin and ECG are negative, cardiac involvement is ruled out.
NURSING CONSIDERATIONS
Inform the patient that he need not restrict food or fluids before the test.
Tell the patient that other tests will be performed along with the IMA test.
Handle the collection tube gently to prevent hemolysis, and send the sample to the laboratory immediately after collection.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
Homocysteine
Homocysteine is an amino acid that’s produced by the body. High homocysteine levels can irritate blood vessels, leading to arteriosclerosis. High levels can also raise low-density lipoprotein levels and make blood clot more easily, increasing the risk of blood vessel blockages. In patients with type 2 diabetes, high homocysteine levels are seen when the patient has a decrease in renal function. Normal homocysteine levels are 4 to 17 μmol/L.
NURSING CONSIDERATIONS
Perform a venipuncture; collect the sample in a 5-ml tube containing EDTA.
Send the specimen to the laboratory immediately after collection in a plastic vial on ice.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
C-reactive protein
C-reactive protein (CRP) is a substance produced by the liver. A high CRP level indicates that inflammation exists at some location in the body. Other diagnostic tests are needed to determine the location of the inflammation and its cause. Elevated CRP levels can indicate such conditions as:
MI
angina
systemic lupus erythematosus
postoperative infection
trauma
heatstroke.
CRP appears in the blood 18 to 24 hours after the onset of tissue damage, and then declines rapidly when the inflammatory process regresses. Some studies have shown a correlation between increased CRP levels and coronary artery disease. Normally, CRP isn’t present in
the blood; however, levels less than 0.8 mg/dl may be reported as normal.
the blood; however, levels less than 0.8 mg/dl may be reported as normal.
NURSING CONSIDERATIONS
Have the patient withhold fluids, except water, for 8 hours before the test.
Perform a venipuncture and collect the sample in a 5-ml nonanticoagulated tube.
Handle the collection tube gently to prevent hemolysis, and send the sample to the laboratory immediately after collection.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
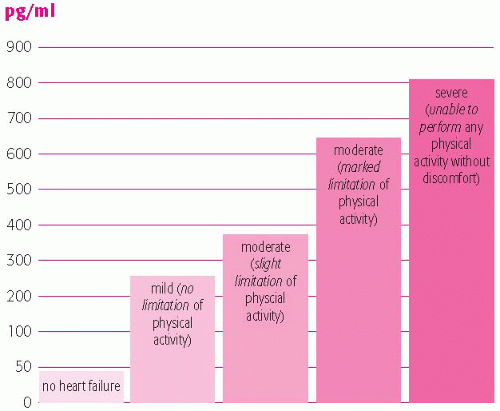
B-type natriuretic peptide
B-type natriuretic peptide (BNP) is a hormone polypeptide secreted by ventricular tissues in the heart. The substance is secreted as a response to the increased ventricular volume and pressure that occurs when a patient is in heart failure. It’s an excellent hormonal marker of ventricular systolic and diastolic dysfunction.
The normal BNP level in the blood is less than 100 pg/ml. Blood concentrations greater than 100 pg/ml are an accurate predictor of heart failure. The level of BNP in the blood is relative to the severity of heart failure. The higher the level, the worse the symptoms of heart failure. (See Linking BNP levels to heart failure symptom severity.)
NURSING CONSIDERATIONS
Perform a venipuncture, and collect the sample in a 5-ml tube containing EDTA.
Handle the collection tube gently to prevent hemolysis, and send the sample to the laboratory immediately after collection.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
Atrial natriuretic peptide
Atrial natriuretic peptide (ANP) is a neurohormone similar to BNP that’s released by the atria in response to increased atrial pressure. ANP helps:
promote sodium excretion
inhibit the renin-angiotensin system’s effects on aldosterone secretion
decrease venous return to the atria, thereby reducing blood pressure and volume.
Normal levels of ANP are 20 to 77 pg/ml. A patient with overt heart failure will have highly elevated levels of ANP. A patient with cardiovascular disease and elevated cardiac filling pressure but no heart failure will also have increased ANP levels.
NURSING CONSIDERATIONS
The patient must fast for 12 hours before the test.
Withhold drugs that may interfere with the test, such as beta-adrenergic blockers, diuretics, vasodilators, and cardiac glycosides.
Perform a venipuncture and collect the blood in a prechilled potassium-EDTA tube.
Handle the collection tube gently to prevent hemolysis, and send the sample to the laboratory immediately after collection.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
LIPID STUDIES
Lipid studies include triglycerides, total cholesterol, and lipoprotein fractionation. They measure lipid levels in the body and help evaluate the risk of coronary artery disease.
Triglycerides
Triglycerides are the main storage form of lipids and constitute about 95% of fatty tissue. Monitoring triglyceride levels in the blood helps with early identification of hyperlipidemia and identification of patients at risk for coronary artery disease (CAD).
Triglyceride values are age- and gender-related, and some controversy exists over the most appropriate normal ranges. The most widely accepted normal values are 44 to 180 mg/dl for men and 10 to 190 mg/dl for women.
Triglyceride levels above or below these values suggest a clinical abnormality; for a definitive diagnosis, you’ll need additional tests. For example, measuring cholesterol levels may also be necessary, because cholesterol and triglyceride levels vary independently. If both triglyceride and cholesterol levels are high, the patient is at risk for CAD.
NURSING CONSIDERATIONS
Because triglycerides are highly affected by a fat-containing meal, with levels rising and peaking 4 hours after ingesting a meal, tell the patient that he should abstain from food for 10 to 14 hours before the test and from alcohol for 24 hours before the test. The patient may drink water.
Perform a venipuncture, collect a sample in a 7-ml tube containing EDTA, and send the sample to the laboratory immediately after collection.
Avoid prolonged venous occlusion. Remove the tourniquet within 1 minute of application.
Total cholesterol
The total serum cholesterol test measures the circulating levels of the two forms in which cholesterol appears in the body—free cholesterol and cholesterol esters.
For adults, desirable cholesterol levels are less than 200 mg/dl. Levels are considered borderline high up to 240 mg/dl, and high if
they’re greater than 240 mg/dl. High serum cholesterol levels may be associated with an increased risk for CAD.
they’re greater than 240 mg/dl. High serum cholesterol levels may be associated with an increased risk for CAD.
NURSING CONSIDERATIONS
Fasting isn’t needed for isolated cholesterol checks or screening, but fasting is required if total cholesterol is part of a lipid profile. If fasting is required, instruct the patient to abstain from food and drink for 12 hours before the test.
Perform a venipuncture, and collect the sample in a 7-ml tube containing EDTA. The patient should be in a sitting position for 5 minutes before the blood is drawn. Fingersticks can also be used for initial screening when using an automated analyzer.
Document the drugs the patient is taking.
Handle the collection tube gently to prevent hemolysis, and send the sample to the laboratory immediately after collection.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
Lipoprotein fractionation
Lipoprotein fractionation tests are used to isolate and measure the two types of cholesterol in blood: high-density lipoproteins (HDLs) and low-density lipoproteins (LDLs).
The HDL level is inversely related to the risk of CAD—that is, the higher the HDL level, the lower the incidence of CAD. For men, HDL values range from 37 to 70 mg/dl; in women, from 40 to 85 mg/dl.
Conversely, the higher the LDL level, the higher the incidence of CAD. In individuals who don’t have CAD, desirable LDL levels are less than 130 mg/dl, borderline high levels are in the range of 130 to 159 mg/dl, and high levels are more than 160 mg/dl.
The American College of Cardiology recommends:
HDL levels of 40 mg/dl or higher for men
HDL levels of at least 45 mg/dl for women. (HDL levels greater than 60 mg/dl are considered heart healthy for all.)
LDL levels of less than 100 mg/dl (Levels of 60 mg/dl or more are considered high.)
Increased HDL levels can occur as a result of long-term aerobic and vigorous exercise. Rarely, a sharp rise (to as high as 100 mg/dl) in a second type of HDL (alpha2-HDL) may signal CAD. (See Predicting CAD with the PLAC test, page 94.)
NURSING CONSIDERATIONS
Tell the patient to maintain a normal diet for 2 weeks before the test.
Tell him to abstain from alcohol for 24 hours before the test.
Tell the patient to stop the use of thyroid hormone, hormonal contraceptives, and antilipemics until after the test because they alter results.
Perform a venipuncture, and collect the sample in a 7-ml tube containing EDTA.
Send the sample to the laboratory immediately after collection to avoid spontaneous redistributions among the lipoproteins. If the sample can’t be transported immediately, refrigerate it but don’t allow it to freeze.
If a hematoma develops at the venipuncture site, apply warm soaks to help ease discomfort.
PREDICTING CAD WITH THE PLAC TEST
The PLAC test, a blood test that can help determine who might be at risk for coronary artery disease (CAD), has been approved by the Food and Drug Administration (FDA). The FDA’s decision was based on a study of more than 1,300 patients, which was a part of a large multicenter study sponsored by the National Heart, Lung, and Blood Institute.
The PLAC test works by measuring lipoprotein-associated phospholipase A2, an enzyme produced by macrophages, a type of white blood cell. When heart disease is present, macrophages increase production of the enzyme. According to the FDA, an elevated PLAC test result, in conjunction with a low-density-lipoprotein (LDL) cholesterol level of less than 130 mg/dl, generally indicates that a patient has two to three times the risk of coronary heart disease compared to similar patients with lower PLAC test results. The study also found that those people with the highest PLAC test results and LDL cholesterol levels lower than 130mg/dL had the greatest risk of heart disease.
COAGULATION TESTS
Partial thromboplastin time, prothrombin time, international normalized ratio, and activated clotting time are tests that measure clotting time. They’re used to measure response to treatment and to screen for clotting disorders.
Partial thromboplastin time
The partial thromboplastin time (PTT) test evaluates all of the clotting factors of the intrinsic pathway except platelets. The test measures the
time it takes a clot to form after adding calcium and phospholipid emulsion to a plasma sample. Normally a clot forms 21 to 35 seconds after the reagents are added.
time it takes a clot to form after adding calcium and phospholipid emulsion to a plasma sample. Normally a clot forms 21 to 35 seconds after the reagents are added.
The PTT test also helps monitor a patient’s response to heparin therapy. For a patient on anticoagulant therapy, check with the practitioner to find out what PTT results to expect.
NURSING CONSIDERATIONS
Tell the patient receiving heparin therapy that this test may be repeated at regular intervals to assess response to treatment.
Perform a venipuncture, and collect the sample in a 7-ml tube containing sodium citrate.
Completely fill the collection tube, invert it gently several times, and send it to the laboratory on ice.
For a patient on anticoagulant therapy, additional pressure may be needed at the venipuncture site to control bleeding.
Prothrombin time
Prothrombin, or factor II, is a plasma protein produced by the liver. The prothrombin time (PT) test (also known as pro time) measures the time required for a clot to form in a citrated plasma sample after the addition of calcium ions and tissue thromboplastin (factor III).
The PT test is an excellent screening procedure for overall evaluation of extrinsic coagulation factors V, VII, and X and of prothrombin and fibrinogen. It’s also the test of choice for monitoring oral anticoagulant therapy.
Normally PT ranges from 10 to 14 seconds. In a patient receiving warfarin therapy, the goal of treatment is to attain a PT level 1 to 2.5 times the normal control value.
NURSING CONSIDERATIONS
Check the patient’s history for use of drugs that may affect test results, such as vitamin K or antibiotics.
Perform a venipuncture, and collect the sample in a 7-ml siliconized tube.
Completely fill the collection tube, and invert it gently several times to adequately mix the sample and anticoagulant. If the tube isn’t filled to the correct volume, an excess of citrate appears in the sample.
International normalized ratio
The international normalized ratio (INR) system is viewed as the best means of standardizing measurement of prothrombin time to monitor
oral anticoagulant therapy. It isn’t used as a screening test for coagulopathies.
oral anticoagulant therapy. It isn’t used as a screening test for coagulopathies.
A normal INR in patients receiving warfarin therapy is 2.0 to 3.0. For patients with mechanical prosthetic heart valves, an INR of 2.5 to 3.5 is suggested. Increased INR values may indicate disseminated intravascular coagulation, cirrhosis, hepatitis, vitamin K deficiency, salicylate intoxication, uncontrolled oral anticoagulation, or massive blood transfusion.
NURSING CONSIDERATIONS
Tell the patient that the test may be repeated at regular intervals until he reaches his target INR level.
Perform a venipuncture and collect the sample in a tube with sodium citrate added.
Completely fill the collection tube, and invert it gently several times to adequately mix the sample and anticoagulant. If the tube isn’t filled to the correct volume, an excess of citrate appears in the sample.
Place the sample on ice and send it to the laboratory immediately after collection.
Activated clotting time
Activated clotting time, or automated coagulation time, measures the time it takes whole blood to clot.
This test is commonly performed during procedures that require extracorporeal circulation, such as:
cardiopulmonary bypass
ultrafiltration
hemodialysis
extracorporeal membrane oxygenation (ECMO).
In a nonanticoagulated patient, the normal activated clotting time is 107 seconds. During cardiopulmonary bypass, heparin is titrated to maintain an activated clotting time between 400 and 600 seconds. During ECMO, heparin is titrated to maintain the activated clotting time between 220 and 260 seconds.
NURSING CONSIDERATIONS
Explain to the patient that the test requires a blood sample that’s usually drawn from an existing vascular access site; therefore, no venipuncture is necessary.
Explain that two samples will be drawn. The first one will be discarded so that heparin in the tubing doesn’t interfere with the results.
If the sample is drawn from a line with a continuous infusion, stop the infusion before drawing the sample.
Withdraw 5 to 10 ml of blood from the line and discard it.
Withdraw a clean sample of blood into the special tube containing the celite provided with the activated clotting time unit.
Turn on the activated clotting time unit, and wait for the signal to insert the tube.
Flush the vacular access site according to your facility’s protocol.
ELECTROCARDIOGRAPHY
The heart’s electrical conduction system can be recorded by using a number of different tests. The most common tests used are a 12-lead electrocardiogram, continuous cardiac monitoring, exercise electrocardiography, Holter monitoring, and signal-averaged electrocardiography.
12-lead electrocardiogram
The 12-lead electrocardiogram (ECG) measures the heart’s electrical activity and records it as waveforms. It’s one of the most valuable and commonly used diagnostic tools.
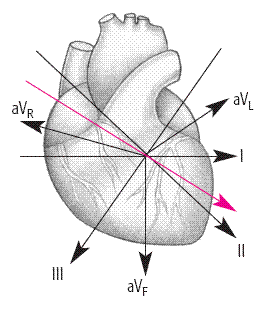
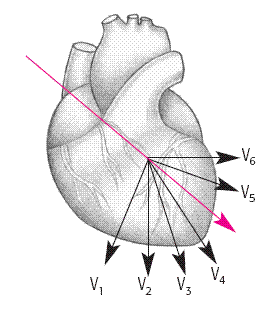
The standard 12-lead ECG uses a series of electrodes placed on the patient’s extremities and chest wall to assess the heart from 12 different views (leads). The 12 leads include:
three bipolar limb leads (I, II, and III)
three unipolar augmented limb leads (aVR, aVL, and aVF)
six unipolar precordial leads (V1 to V6).
The limb leads and augmented leads show the heart from the frontal plane. The precordial leads show the heart from the horizontal plane. (See Understanding ECG leads, page 98.)
ECG can be used to identify myocardial ischemia and infarction, rhythm and conduction disturbances, chamber enlargement, electrolyte imbalances, and drug toxicity.
NURSING CONSIDERATIONS
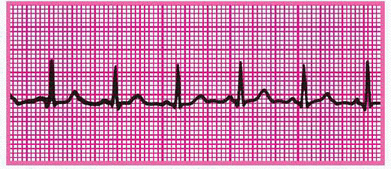
Use a systematic approach to interpret the ECG recording. (See Visualizing normal ECG waveforms, pages 99 and 100.) Compare the patient’s previous ECG with the current one, if available. This will help you identify changes.
P waves should be upright; however they may be inverted in lead aVR or biphasic or inverted in leads III, aVL, and V1.
UNDERSTANDING ECG LEADS
Each of the leads on a 12-lead ECG views the heart from a different angle. These illustrations show the direction of electrical activity (depolarization) monitored by each lead and the 12 views of the heart.
VIEWS REFLECTED | LEAD | VIEW OF THE HEART |
|---|---|---|
| STANDARD LIMB LEADS (BIPOLAR) | |
I | lateral wall | |
II | inferior wall | |
III | inferior wall | |
AUGMENTED LIMB LEADS (UNIPOLAR) | ||
aVR | no specific view | |
aVL | lateral wall | |
aVF | inferior wall | |
| PRECORDIAL, OR CHEST, LEADS (UNIPOLAR) | |
V1 | septal wall | |
V2 | septal wall | |
V3 | anterior wall | |
V4 | anterior wall | |
V5 | lateral wall | |
V6 | lateral wall | |
PR intervals should always be constant, like QRS-complex durations.
QRS-complex deflections vary in different leads.
ST segments should be isoelectric or have minimal deviation.
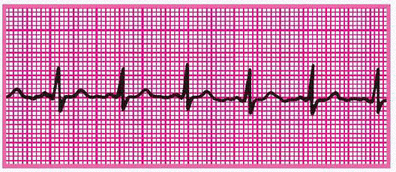
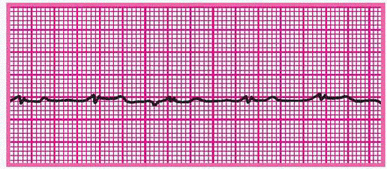
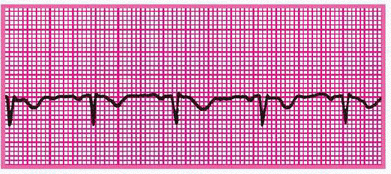
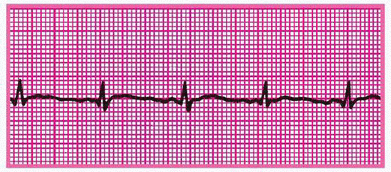
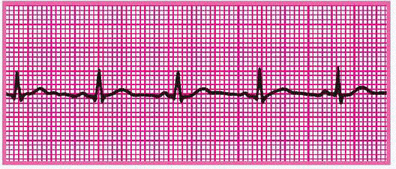
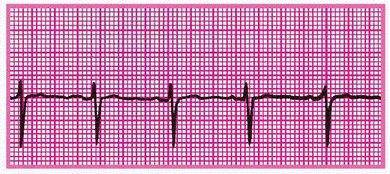
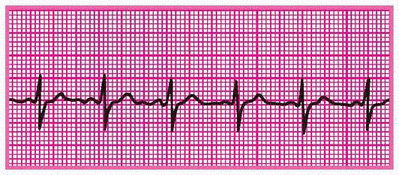
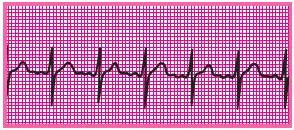
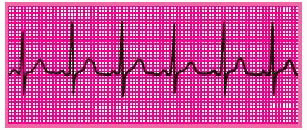
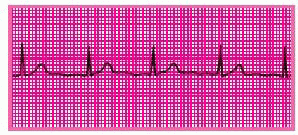
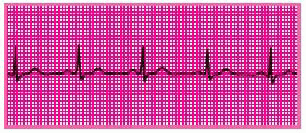
VISUALIZING NORMAL ECG WAVEFORMS
Each of the 12 standard leads of an electrocardiogram (ECG) takes a different view of heart activity, and each generates its own characteristic tracing. The tracings shown here represent a normal heart rhythm viewed from each of the 12 leads. Keep in mind:
An upward (positive) deflection indicates that the wave of depolarization flows toward the positive electrode.
A downward (negative) deflection indicates that the wave of depolarization flows away from the positive electrode.
An equally positive and negative (biphasic) deflection indicates that the wave of depolarization flows perpendicularly to the positive electrode.
Each lead represents a picture of a different anatomic area; when you find abnormal tracings, compare information from the different leads to pinpoint areas of cardiac damage.
LEAD I | LEAD II |
|
|
LEAD III | LEAD aVR |
|
|
LEAD aVL | LEAD aVF |
|
|
LEAD V1 | LEAD V2 |
|
|
LEAD V3 | LEAD V4 |
|
|
LEAD V5 | LEAD V6 |
|
|
The T wave normally deflects upward in leads I, II, and V3 through V6. It’s inverted in lead aVR and variable in the other leads. T-wave changes have many causes and aren’t always a reason for alarm. Excessively tall, flat, or inverted T waves occurring with such symptoms as chest pain may indicate ischemia.
A normal Q wave generally has a duration of less than 0.04 second. An abnormal Q wave has a duration of 0.04 second or more, a depth greater than 4 mm, or a height one-fourth of the R wave. Abnormal Q waves indicate myocardial necrosis, developing when depolarization can’t follow its normal path because of damaged tissue in the area.
Remember that aVR normally has a large Q wave, so disregard this lead when searching for abnormal Q waves.
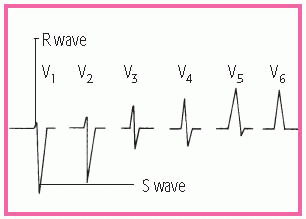
The R wave in lead II should be taller than in lead I. The R wave in lead III should be a smaller version of the R wave in lead I. Normally, the R waves get progressively taller from lead V1 to V5 and get slightly smaller in lead V6. (See R-wave progression.)
Continuous cardiac monitoring
Because it allows continuous observation of the heart’s electrical activity, cardiac monitoring is used in patients at risk for life-threatening arrhythmias.
Like other forms of electrocardiography, cardiac monitoring uses electrodes placed on the patient’s chest to transmit electrical signals that are converted into a cardiac rhythm tracing on an oscilloscope. (See Positioning monitor leads, pages 102 and 103.)
Like other forms of electrocardiography, cardiac monitoring uses electrodes placed on the patient’s chest to transmit electrical signals that are converted into a cardiac rhythm tracing on an oscilloscope. (See Positioning monitor leads, pages 102 and 103.)
Two types of monitoring may be performed: hardwire or telemetry. In hardwire monitoring, the patient is connected to a monitor at the bedside. The rhythm display appears at the bedside, or it may be transmitted to a console at a remote location. Telemetry uses a small transmitter connected to the ambulatory patient to send electrical signals to another location, where they’re displayed on a monitor screen. Regardless of the type, cardiac monitors can display the patient’s heart rate and rhythm, produce a printed record of cardiac rhythm, and sound an alarm if the heart rate exceeds or falls below specified limits. Monitors also recognize and count abnormal heartbeats as well as changes. (See Identifying cardiac monitor problems, page 104.)
NURSING CONSIDERATIONS
Make sure that all electrical equipment and outlets are grounded to avoid electrical shock and interference (artifacts). Also ensure that the patient is clean and dry to prevent electric shock.
If the patient’s skin is very oily, scaly, or diaphoretic, rub the electrode site with a dry 4″ × 4″ gauze pad before applying the electrode, to help reduce interference in the tracing.
Assess skin integrity and reposition the electrodes every 24 hours or as necessary.
Document a rhythm strip at least every 8 hours and with any change in the patient’s condition (or as stated by your facility’s policy).
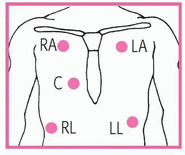
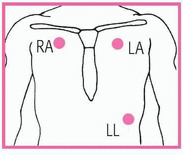
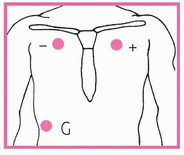
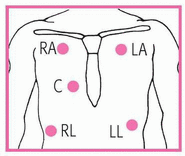
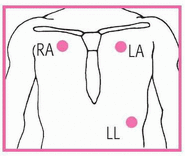
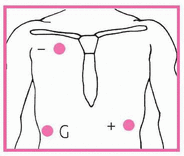
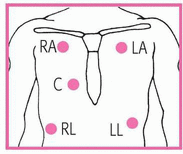
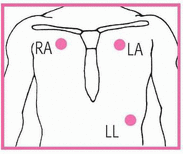
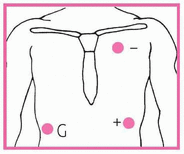
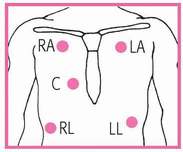
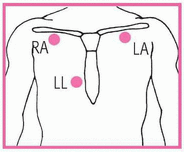
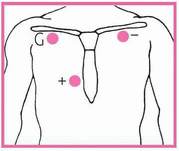
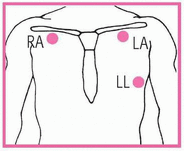
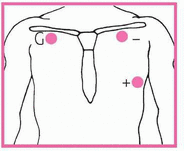
POSITIONING MONITOR LEADS
This chart shows the correct electrode positions for some of the leads you’ll use most often—the five-leadwire, three-leadwire, and telemetry systems. The chart uses the abbreviations RA for the right arm, LA for the left arm, RL for the right leg, LL for the left leg, C for the chest, and G for the ground.
Electrode positions
In the three- and five-leadwire systems, electrode positions for one lead may be identical to those for another lead. When that happens, change the lead selector switch to the setting that corresponds to the lead you want. In some cases, you’ll need to reposition the electrodes.
Exercise electrocardiography
Exercise electrocardiography is a noninvasive test that helps the practitioner assess cardiovascular response to an increased workload. Commonly known as a stress test, it provides diagnostic information that can’t be obtained from a resting electrocardiogram (ECG). This test may also assess response to treatment.
An ECG and blood pressure readings are taken while the patient walks on a treadmill or pedals a stationary bicycle, and his response to a constant or increasing workload is observed. Unless complications develop, the test continues until the patient reaches the target heart rate (determined by an established protocol) or experiences chest pain or fatigue.
Stop the test if the patient experiences chest pain, fatigue, or other signs and symptoms that reflect exercise intolerance. These may include:
severe dyspnea
claudication
weakness
dizziness
hypotension
IDENTIFYING CARDIAC MONITOR PROBLEMS
PROBLEM | POSSIBLE CAUSES | SOLUTIONS |
|---|---|---|
FALSE-HIGH-RATE ALARM | • Monitor interpreting large T waves as QRS complexes, which doubles the rate | • Reposition electrodes to lead where QRS complexes are taller than T waves. |
• Skeletal muscle activity |