45 Diagnostic Techniques in Vascular Disease
Etiology and Pathogenesis
A large number of pathologic processes result in arterial occlusive and aneurysm diseases. By far the most common etiology is atherosclerotic plaque formation in the vessel wall leading to luminal narrowing, wall calcification, plaque destabilization and hemorrhage with rupture, thrombosis, and end-organ damage or showering of emboli distally with resulting tissue damage and necrosis. In other circumstances, atherosclerosis leads to weakening of the vessel lumen leading to true aneurysms, defined as a vessel diameter greater than 1.5 times its normal diameter involving all layers. Genetic abnormalities and environmental exposures are almost always contributory in individuals with advanced vascular pathology. Specific genetic abnormalities have been elucidated in Marfan’s syndrome (fibrillin-1), Ehlers-Danlos syndrome, William’s syndrome (hypercalcemia), Loeys-Dietz syndrome (transforming growth factor-β receptor), and homocysteinuria. Thromboangiitis obliterans (Buerger’s disease), which is usually associated with heavy nicotine use, is also seen with PVD. Other risk factors for atherosclerosis (e.g., hypertension, diabetes, lipid abnormalities) all accelerate disease progression and may lead to a need for surgical or percutaneous intervention. Extrinsic mass effects or vessel encasement in the case of popliteal artery entrapment by the gastrocnemius muscle, celiac artery by the diaphragmatic crus (median arcuate ligament syndrome), or renal artery by neurofibromatosis may lead to similar occlusive symptoms. Clinical manifestations depend on the location and severity of the vessel disease and presence of collateral circulation (see Chapter 44 for additional information on the pathogenesis of atherosclerosis).
Lower Extremity Peripheral Vascular Disease
Diagnostic Approach
Duplex Ultrasonography
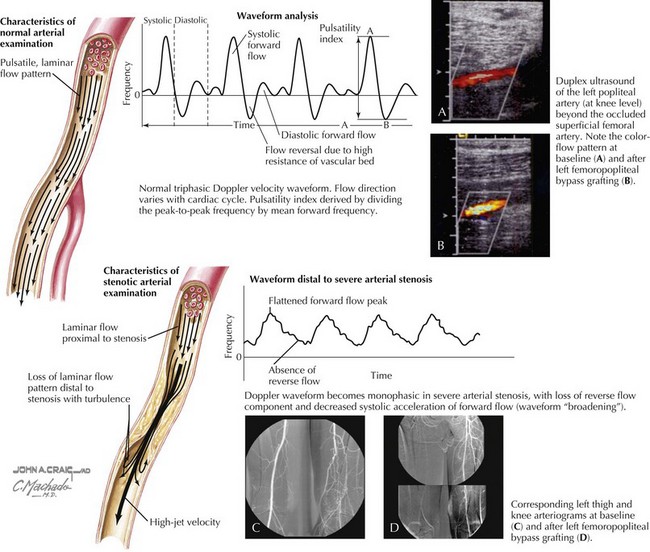
Doppler waveform analysis is an accurate method for defining arterial lesion location and severity (Fig. 45-1). Significant arterial stenoses alter the pattern of flow velocity, as assessed by continuous-wave Doppler analysis. A change in the flow velocity waveform—an increase in peak systolic velocity at the site of the lesion, turbulence, loss of the reverse flow component, or a decrease in pulse velocity distal to the lesion—is diagnostic of a flow-limiting arterial lesion. Color Doppler imaging is able to identify the vessel(s) of interest. A critical stenosis (>50%) is characterized by poststenotic turbulence on color imaging (see Fig. 45-1) and a doubling of the peak systolic velocity on continuous-wave Doppler.