The aim of this study was to determine the diagnostic value of cardiac magnetic resonance (CMR) imaging with late gadolinium enhancement (LGE), cine imaging, and resting first-pass perfusion (FPP) in the evaluation for ischemic (IC) versus nonischemic (NIC) cardiomyopathy in new-onset heart failure with reduced (≤40%) left ventricular ejection fraction (HFrEF). A retrospective chart review analysis identified 83 patients from January 2009 to June 2012 referred for CMR imaging evaluation for new-onset HFrEF with coronary angiography performed within 6 months of CMR. The diagnosis of IC was established using Felker criteria on coronary angiography. CMR sequences were evaluated for the presence of patterns suggestive of severe underlying coronary artery disease as the cause of HFrEF (subendocardial and/or transmural LGE, regional wall motion abnormality on cine, regional hypoperfusion defect on resting FPP). Discriminative power was assessed using receiver operator characteristics curve analysis. Coronary angiography identified 36 patients (43%) with IC. Presence of subendocardial and/or transmural LGE alone demonstrated good discriminative power (C-statistic 0.85, 95% confidence interval 0.76 to 0.94) for the diagnosis of IC. The presence of an ischemic pattern on both LGE and cine sequences resulted in a specificity of 87% for the diagnosis of IC, whereas the absence of an ischemic pattern on both LGE and cine sequences resulted in a specificity of 94% for the diagnosis of NIC. Addition of resting FPP on a subset of patients did not improve diagnostic values. In conclusion, CMR has potential value in the diagnostic evaluation of IC versus NIC.
Heart failure affects 5.1 million people in the United States, and the prevalence is expected to increase as the population ages and the prognosis after acute coronary events improves. Over 650,000 new diagnoses of heart failure are made yearly, more than half of which are associated with a reduced ejection fraction. Heart failure with reduced ejection fraction (HFrEF) may be secondary to severe coronary artery disease (CAD) in up to 2/3 of cases, leading to the categorization of ischemic cardiomyopathy (IC) versus nonischemic cardiomyopathy (NIC). Early diagnosis and identification of cause is crucial because the prognosis of patients with IC may improve following revascularization. Current guidelines recommend invasive coronary angiography in all patients presenting with new-onset heart failure. However, as invasive angiography presents a small risk of serious morbidity, alternative noninvasive strategies to diagnose IC versus NIC should be explored. Cardiac magnetic resonance (CMR) imaging has superior safety profile and the ability to identify myocardial fibrosis or scar. In this study, we aimed to evaluate the utility of CMR in the diagnosis of IC versus NIC in patients presenting with newly diagnosed HFrEF.
Methods
This was a retrospective study of patients undergoing CMR within 2 months of a new diagnosis of heart failure with left ventricular ejection fraction ≤40% and a coronary angiogram within 6 months of the CMR scan. Consecutive patients were included from January 2009 to June 2012 at 2 tertiary care sites, New York University (NYU) Langone Medical Center and Bellevue Hospital Center (BHC). The former is a private academic tertiary referral center, whereas the latter serves as the cardiac referral center for the underserved population within the New York City Health and Hospital Corporation system. Both hospitals are affiliated with the NYU School of Medicine. CMR images and coronary angiograms were interpreted by the same group of cardiac radiologists and interventional cardiologists at both sites. Patients were excluded if they met one of the following criteria: (1) known history of severe CAD, previous myocardial infarction, or previous coronary revascularization; (2) known history of structural heart disease such as hypertrophic cardiomyopathy or congenital heart disease; (3) evidence of severe left-sided valvular disease; or (4) diagnosis of ST-segment elevation myocardial infarction on admission. The study was approved by the NYU School of Medicine and BHC Institutional Review Boards.
Baseline demographic, clinical, and CMR variables were recorded from review of the electronic medical record (EMR). Obesity was defined as a body mass index ≥30 kg/m 2 . History of hypertension was defined per previous documentation in the EMR. Dyslipidemia was defined as a low-density lipoprotein cholesterol >130 mg/dl or previous documentation in the EMR. Diabetes mellitus was defined HbA1c ≥6.5% or previous documentation in the EMR.
Coronary angiograms were evaluated by 2 independent board-certified practicing interventional cardiologists blinded to all clinical, echocardiographic, and CMR data. Significant CAD was defined as a ≥70% diameter stenosis in a coronary artery ≥2 mm in caliber by visual assessment of coronary angiogram or pressure gradient <0.80 if fractional flow reserve measurement was performed. The gold standard etiology of IC was determined using the definition established by Felker et al: presence of ≥70% diameter stenosis in the left main coronary artery, proximal left anterior descending (LAD) artery, or ≥2 epicardial coronary arteries. For those angiograms not categorized to the same IC or NIC classification by the 2 readers (n = 5), a third independent blinded interventional cardiologist served as the final reader.
Patients were imaged using a 1.5T or 3.0T MRI system (Avanto, TimTrio, or Verio; Siemens, Erlangen, Germany). CMR was performed using a standard clinical protocol for evaluation of patients with cardiomyopathy, including use of late gadolinium enhancement (LGE) sequences, cine images, and, when applicable, resting first-pass perfusion (FPP). Imaging was performed in standard 2-, 3-, and 4-chamber long-axis views and a short-axis series (base to apex) that was acquired every 10 mm to cover the entire left ventricle.
Per standard clinical protocol, CMR images were analyzed using the American Heart Association 17-segment model, and each segment was evaluated qualitatively on LGE and cine sequences. LGE sequences were used to identify myocardial scar in a pattern suggestive of significant coronary artery disease (ischemic pattern with subendocardial and/or transmural LGE) versus other cause (nonischemic pattern with midwall and/or subepicardial LGE or absence of LGE). Because previous reports differ regarding the optimal number of segments used to diagnose IC, separate analyses of LGE were performed using both 1-and 3-segment thresholds. Cine sequences were used to identify regional versus global abnormal myocardial wall motion, with each segment reported as normal, mild/moderate/severe hypokinesia, akinesia, or dyskinesia. In the subset of patients who underwent FPP, resting FPP sequences were used to identify presence versus absence of regional myocardial perfusion defects. All imaging data were obtained from retrospective review of clinical CMR reports, which were generated by the same group of CMR readers at both sites.
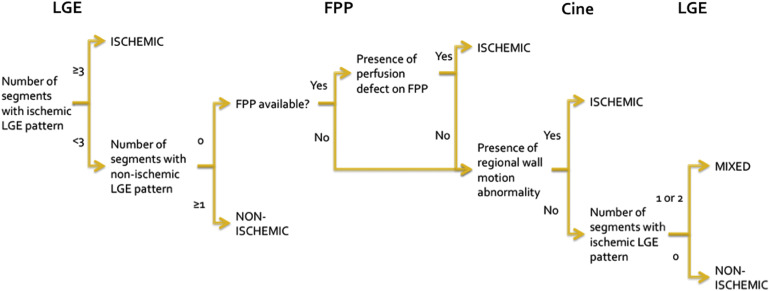
CMR sequences were evaluated independently and in combination to diagnose IC versus NIC. A diagnostic algorithm incorporating all 3 sequences, in accordance with current clinical practice, was also used ( Figure 1 ). In this clinically based CMR algorithm, a third category, termed “mixed” cardiomyopathy, was created for patients with 1 or 2 ischemic LGE segments without perfusion defect on resting FPP and without regional wall motion abnormality on cine.
All continuous variables were evaluated for normality using the Shapiro–Wilk test and determined to be normally distributed. Continuous variables, presented as mean ± standard deviation, were compared between IC and NIC groups using independent sample t test. Categorical variables, presented as proportions, were compared between IC and NIC groups using Fisher’s exact or the chi-square test. To evaluate CMR’s diagnostic utility in differentiating IC versus NIC, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), diagnostic accuracy, and discriminative power were calculated for different CMR sequences using Felker’s criteria on coronary angiography as the gold standard for diagnosis. Diagnostic accuracy was calculated as a percentage of diagnoses that were equivalent between CMR and coronary angiography. Discriminative power was assessed using receiver operator characteristics curve analysis.
Results
Eighty-three consecutive patients met inclusion/exclusion criteria. Approximately 61% (n = 51) were from the BHC site, and the proportion of patients with IC was similar between both sites (45% at NYU Langone Medical Center and 41% at BHC, p = 0.86). Most patients had a coronary angiogram performed before CMR in the IC and NIC groups (69% and 55%, p = 0.28). Baseline characteristics are provided in Table 1 .
| Variable | Total (n=83) | Type of Cardiomyopathy | p-value † | |
|---|---|---|---|---|
| Ischemic ∗ (n=36) | Non-ischemic ∗ (n=47) | |||
| Age (years) | 58.8 ± 12.1 | 61.7 ± 11.1 | 56.5 ± 12.5 | 0.06 |
| Men | 59 (71%) | 29 (81%) | 30 (64%) | 0.14 |
| White, not Hispanic | 28 (34%) | 12 (33%) | 16 (34%) | 0.03 |
| Black, not Hispanic | 24 (29%) | 5 (14%) | 19 (40%) | |
| Hispanic | 20 (24%) | 11 (31%) | 9 (19%) | |
| Asian | 6 (7%) | 5 (14%) | 1 (2%) | |
| Other | 5 (6%) | 3 (8%) | 2 (4%) | |
| Body mass index (kg/m 2 ) | 29.5 ± 7.5 | 28.4 ± 4.6 | 30.4 ± 9.1 | 0.23 |
| Obesity ‡ | 32 (39%) | 12 (33%) | 20 (43%) | 0.50 |
| Hypertension | 49 (59%) | 24 (67%) | 25 (53%) | 0.26 |
| Dyslipidemia § | 40 (48%) | 24 (67%) | 16 (34%) | 0.004 |
| Diabetes mellitus | 29 (35%) | 20 (56%) | 9 (19%) | 0.001 |
| Chest pain | 39 (47%) | 16 (44%) | 23 (49%) | 0.83 |
| Smoker | 45 (56%) | 22 (61%) | 23 (51%) | 0.50 |
| Troponin >99 th percentile of the upper reference limit | 54 (70%) | 26 (84%) | 28 (61%) | 0.04 |
∗ Diagnosed using Felker’s criteria on coronary angiography.
† Ischemic versus non-ischemic cardiomyopathy cohort comparison.
‡ Obesity defined as body mass index ≥30 kg/m 2 .
§ Dyslipidemia defined as low-density lipoprotein-cholesterol >130 mg/dL or prior documentation in the electronic medical record.
All 83 patients had results available for LGE and cine sequences, whereas 68 (82%) had a resting FPP sequence performed as part of their CMR protocol. Left ventricular characteristics by CMR are provided in Table 2 . Of the 4 patients in the IC group who did not demonstrate an ischemic pattern on LGE, 3 had nonproximal coronary artery stenoses and 1 had a severe stenosis in the proximal LAD artery.
| Variable | Total (n=83) | Type of Cardiomyopathy | p-value † | |
|---|---|---|---|---|
| Ischemic ∗ (n=36) | Non-ischemic ∗ (n=47) | |||
| Ejection fraction (%) | 27.1 ± 8.1 | 26.7 ± 6.9 | 27.4 ± 8.9 | 0.71 |
| End-diastolic volume (mL) | 240.0 ± 80.3 | 226.2 ± 62.3 | 250.3 ± 91.0 | 0.18 |
| End-systolic volume (mL) | 178.2 ± 74.2 | 167.9 ± 57.7 | 186.2 ± 84.4 | 0.27 |
| Late gadolinium enhancement ‡ | ||||
| Absent | 19 (23%) | 3 (8%) | 16 (34%) | 0.01 |
| Non-ischemic only pattern | 17 (20%) | 1 (3%) | 16 (34%) | <0.001 |
| Ischemic only pattern | 38 (46%) | 27 (75%) | 11 (23%) | <0.001 |
| Ischemic and non-ischemic patterns | 9 (11%) | 5 (14%) | 4 (9%) | 0.50 |
| Cine (regional wall motion abnormality) | 30 (36%) | 20 (56%) | 10 (21%) | 0.003 |
| FPP (presence of hypoperfusion) (n=68) | 34 (50%) | 20 (69%) | 14 (36%) | 0.01 |
| Clinical algorithm § | 47 (57%) | 31 (86%) | 16 (34%) | <0.001 |
∗ Diagnosed using Felker’s criteria on coronary angiography.
† Ischemic versus non-ischemic cardiomyopathy cohort comparison.
‡ Non-ischemic pattern is defined as midwall and/or subepicardial late gadolinium enhancement, and ischemic pattern is defined as subendocardial and/or transmural late gadolinium enhancement.
§ Patients categorized as mixed cardiomyopathy by the clinical algorithm (see Figure 1 ) are categorized as ischemic cardiomyopathy by CMR.
The sensitivity, specificity, PPV, NPV, and diagnostic accuracy of the individual CMR sequences and in combination are provided in Tables 3 and 4 . LGE-CMR had the highest diagnostic accuracy for the diagnosis of IC, with good discriminative power (c-statistic 0.85, 95% confidence interval 0.76 to 0.94).
| Variable | n | Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Diagnostic Accuracy (%) |
|---|---|---|---|---|---|---|
| LGE ∗ | 47/83 | 89 | 68 | 68 | 89 | 77 |
| LGE † | 39/83 | 78 | 77 | 72 | 82 | 77 |
| Cine ‡ | 30/83 | 56 | 79 | 67 | 70 | 69 |
| LGE ∗ or cine | 53/83 | 94 | 60 | 64 | 93 | 75 |
| LGE ∗ and cine | 24/83 | 50 | 87 | 75 | 69 | 71 |
| LGE ∗ , cine, or FPP | 46/68 | 93 | 51 | 59 | 91 | 69 |
| LGE ∗ , cine, and FPP | 17/68 | 41 | 87 | 71 | 67 | 67 |
| Clinical algorithm | 47/83 | 86 | 66 | 66 | 86 | 75 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


