We assessed the performance of a new-generation, 256-row computed tomography (CT) scanner for detection of obstructive coronary artery disease (CAD) compared to invasive quantitative coronary angiography. A total 121 consecutive symptomatic patients without known CAD referred for invasive coronary angiography (age 59 ± 12 years, 37% women) underwent clinically driven 256-row coronary computed tomographic angiography (CCTA) before the invasive procedure. Obstructive CAD (>50% diameter stenosis) was assessed visually on CCTA by 2 independent observers using the 18-segment society of cardiovascular CT model and on invasive angiograms using quantitative coronary angiography (the reference standard). Observers were unaware of the findings from the alternate modality. Nonassessable coronary computed tomographic angiographic segments were considered obstructive for the purpose of analysis. Quantitative coronary angiography demonstrated obstructive CAD in 145 segments in 82 of 121 patients (68%). Overall, 1,677 coronary segments were available for comparative analysis, of which 39 (2.3%) were nonassessable by CCTA, mostly because of heavy calcification. Patient-based and segment-based analysis showed a sensitivity of 100% and 97% (95% confidence interval 95% to 100%) and specificity of 69% (95% confidence interval 55% to 84%) and 97% (confidence interval 96% to 98%), respectively. Four segments with obstructive CAD in 4 patients were not detected by CCTA. All 4 patients had additional coronary obstructions identified by CCTA. The predictive accuracy was 90% (range 85% to 95%) for patient based and 97% (96% to 98%) for segment based analysis. In conclusion, 256-row CCTA showed high sensitivity and high predictive accuracy for detection of obstructive CAD in patients without previously known disease. Although coronary calcification might still interfere with analysis, the rate of nonassessable segments was low.
Coronary computed tomographic angiography (CCTA) allows rapid scanning of the heart and great vessels, requires minimal patient cooperation, and has high diagnostic accuracy for identifying coronary stenosis and coronary atheromatous plaques. Multicenter studies evaluating the accuracy of 64-slice computed tomography (CT) for diagnosing obstructive coronary artery disease (CAD), reported high sensitivity in relation to the commonly used reference standard for diagnosis—invasive coronary angiography (ICA). The newest generation computed tomography (CT) scanners have introduced new techniques to improve spatial and temporal resolution and therefore image quality and might allow improved diagnostic accuracy. However, few data are available assessing the performance characteristics of new-generation CT scanners in general and specifically of the new-generation 256-row CT scanners. The purpose of the present study was to evaluate the diagnostic accuracy of 256-row CCTA in the detection of obstructive CAD in symptomatic patients without previously known disease using quantitative coronary angiography (QCA) assessment of ICA as the reference standard.
Methods
The present retrospective, observational, single-center study was approved by the institutional review board with waiver of informed consent. The cohort included consecutive symptomatic patients without previously diagnosed CAD who underwent 256-row CCTA in our institution within a 2-year period followed by ICA within <2 months after CCTA. Patients presented either as elective outpatients or as emergency department patients with atypical chest pain and without high-risk features (i.e., without ongoing/recurrent angina, typical ST-segment deviation suggestive of ischemia, or an elevated troponin level), and were referred for CCTA to “rule out” acute coronary syndrome.
Patients were eligible for inclusion in the study if they were >18 years old and were in sinus rhythm. In the present retrospective study, the exclusion criteria were known CAD and/or previous revascularization. No patient was excluded because of poor-quality CCTA. Patients with iodine allergy, renal function impairment (creatinine clearance <60 ml/min), or pregnancy were not included. A routine structured interview on the day of CCTA provided information regarding the baseline data and risk factors.
CCTA was performed using a 256-row scanner (Brilliance iCT, Philips Healthcare, Cleveland Ohio), which has a longitudinal coverage of 8 cm, offers options for different rotation times. which can be as fast as 0.27 second, and has a 120-kW generator. CCTA was performed either as prospectively triggered “step-and-shoot” mode or with helical retrospective electrocardiographic (ECG) gating. ECG-based tube current modulation was used when possible with retrospective gating.
Oral and/or intravenous β blockers were used to lower the heart rate when it was >70 beats/min. Sublingual nitroglycerine (0.4 mg) was given before CCTA for all patients with systolic blood pressure of ≥110 mm Hg and no clinical contraindications (e.g., aortic stenosis or suspected pulmonary embolism). The coronary artery calcium score (Agatston units [AU]) was measured on a nonenhanced scan (using prospective ECG triggering), and a contrast-enhanced scan was then performed using a bolus of 69 ± 11 ml (range 50-100) Iohexol (Omnipaque 350 mg Iodine/ml, GE Healthcare, Princeton, New Jersey) injected into an antecubital vein at a flow rate of 5 to 6 ml/s, followed by a mixed 50% contrast/saline injection and then a 20- to 30-ml saline chaser bolus. The iohexol dose was calculated according to the following formula: (predicted scan time in seconds + 5) × intravenous contrast flow rate. The scans were performed at 120 kV (or 100 kV in 14 patients with a body mass index <24 kg/m 2 and a heart rate at rest of <60 beats/min in last 6 months of the study) with a slice collimation of 128 × 0.625 mm, with dual z-focal spot positions (which leads to a double number of simultaneous imaged slices per gantry rotation; therefore 256-row acquisition), and a rotation time of 0.27 or 0.33 second. The helical scans (retrospective ECG gating) were performed with an effective tube current (rotation time product normalized by the pitch) in the range of 900 to 1,500 mA (effective), depending on the body mass index and body habitus, and a pitch of 0.14 to 0.18. The “step-and-shoot” mode scans were performed in patients with a stable heart rhythm and a heart rate <65 beats/min with a tube current–x-ray “ON” time product of 160 to 300 mAs. The scanner provided several predefined protocols that determined the pitch and rotation time for each protocol according to the scanning mode, heart rate, and whether a “bariatric mode” (high mA) was used (to allow optimal temporal resolution at all settings). Radiation exposure was assessed as dose-length-product (product of scan length and CT dose index). Reconstruction was performed using a window centered at 75% of the R-R interval as the default. For heart rates >70 beats/min, an earlier reconstruction phase (usually ≤45%) was frequently used with retrospective gating.
The interpretation and diagnosis of CAD on CCTA scans was performed separately by 2 experienced readers (R.R., T.G.), who were unaware of the invasive angiographic results. The 2 reports included the clinical reading (before ICA) and post hoc reading by the alternate reader. The post hoc readers were also unaware of the clinical presentation. If disagreement occurred between the 2 readers, the results were adjudicated by a third reader (N.P.). Interpretation of the results was performed on the scanner workstation (Extended Brilliance Workstation, Philips Healthcare) with all available techniques, including curved multiplanar reformations. Obstructive CAD was defined as >50% diameter stenosis.
Recording and analysis were performed using the 18-segment Society of Cardiovascular Computed Tomography model. Four coronary segments were defined as “proximal”: the left main stem, proximal left anterior descending artery, proximal left circumflex artery, and proximal right coronary artery.
All ICA procedures were performed using the standard technique with the Judkins femoral or radial artery approach. QCA was performed off-line using the Coronary Artery Analysis System, version 3.2 (Pie Medical Imaging, Maastricht, The Netherlands) by a different observer (O.P. or D.A.H.) who had no knowledge of the CCTA results. The proximal and distal reference vessel diameters and minimal lumen diameter of the suspected lesion were recorded using the catheter shaft diameter for calibration, and the percentage of diameter stenosis was calculated using the same 18-segment Society of Cardiovascular Computed Tomography model as for CCTA analysis.
Nonassessable segments on CCTA were considered obstructive for the purposes of the primary analysis. The performance characteristics (patient-based, vessel-based, and segment-based) of CCTA to detect obstructive CAD were calculated using QCA as the reference standard. Differences between the false-positive rates in patients with and without an elevated calcium score were calculated using the chi-square test. p Values <0.05 were considered significant. Statistical analysis was performed using the Statistix, version 8, software package (Analytical Software, Tallahassee, Florida).
Results
Among 1,477 patients undergoing CCTA during the study period, 931 had no previously known CAD (63%). Of these 931 patients, 121 (37% women, age range 30 to 86 years) met the study inclusion criteria. The patients’ baseline characteristics are presented in Table 1 .
| Variable | Value |
|---|---|
| Age (yrs) | |
| Mean ± SD | 59 ± 12 |
| Range | 30–86 |
| Women | 45 (37%) |
| Hypertension ∗ | 85 (70%) |
| Diabetes mellitus | 32 (26%) |
| Hyperlipidemia † | 82 (68%) |
| Smoking history | 53 (44%) |
| Family history of CAD ‡ | 32 (26%) |
| Peripheral vascular disease | 6 (5%) |
| Body mass index (kg/m 2 ) | |
| Median | 27 |
| Interquartile range | 24–30 |
| Agatston calcium score | |
| Median | 12 |
| Interquartile range | 6–517 |
| Acute presentation (emergency department) | 79 (65%) |
∗ Blood pressure >140/90 mm Hg or treatment with antihypertensive medication.
† Total serum cholesterol level ≥5 mmol/L or treatment with lipid-lowering drugs.
‡ CAD in first-degree relatives <55 (men) or <65 (women) years old.
No scan was excluded because of poor diagnostic quality. The mean heart rate during the scans was 61 ± 8 beats/min (range 42–82). With the advances in scanner software during the study period, the scanning modes changed. In general, most scans during the first study year were performed with retrospective gating, and most scans performed during the second study year were performed using prospective ECG triggering (“step-and-shoot” mode). Overall, 67 patients (55%) were scanned using the “step-and-shoot” mode and 54 (45%) using retrospective ECG gating. In 14 patients (12%), a tube voltage of 100 kV was used. The median dose-length-product was 438 mGy × cm (range 160 to 1,392), resulting in a median effective radiation dose estimate of 6.1 mSv (range 2.2 to 19.5) using a conversion coefficient k of 0.014 for the chest.
QCA demonstrated obstructive CAD (>50% diameter stenosis) in 145 segments among the 82 of 121 patients (68%). The detailed anatomic distributions of the obstructive segments and extent of CAD are presented in Tables 2 and 3 .
| Coronary Artery Segment | n | Detailed Distribution |
|---|---|---|
| Left main | 3 | |
| Left anterior descending (and branches) | 56 | Proximal, 18; mid, 27; distal or branches, 11 |
| Left circumflex (and branches) | 31 | Proximal, 12; distal or branches, 19 |
| Right (and branches) | 53 | Proximal, 12; mid, 22; distal or branches, 19 |
| Intermediate branch | 2 |
| Variable | n (%) |
|---|---|
| Coronary arteries involved (n) | |
| 0 | 39 (32) |
| 1 | 53 (44) |
| 2 | 22 (18) |
| 3 | 4 (3) |
| Left main | 3 (2) |
| Left main or 3 vessels | 7 (6) |
The results of the pre-CCTA, nonenhanced CT scans for calcium scoring showed a wide range of AU values, as expected ( Table 1 ). A total of 56 patients had a low calcium score (<100 AU), of whom 26 patients had a 0 calcium score. A total of 35 patients had a high calcium score (>400 AU). After CCTA, 1,677 coronary segments were available for comparative analysis (between CCTA and QCA of ICA), of which 39 (2.3%) in 16 patients were nonassessable by CCTA. The most frequent cause of an inability to assess a segment was heavy calcification in 26 of 39 segments. Other reasons included low intravascular contrast or excessive image noise in 7 and significant motion artifacts in 6 segments. Nonassessable segments were considered obstructive for the purpose of the present analysis.
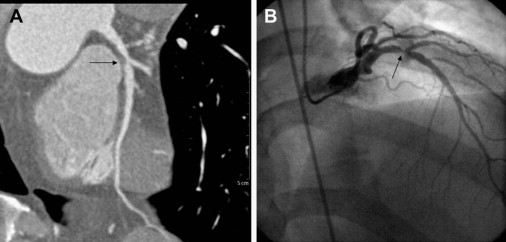
Overall, of the 145 segments with obstructive CAD on QCA, CCTA correctly identified 141 (sensitivity 97%, Table 4 ). An example is shown in Figure 1 . Four segments with obstructive CAD in 4 different patients were not detected by CCTA. All 4 patients had additional coronary obstructions identified by CCTA (and QCA). Hence, the patient-based sensitivity was 100%. All 4 false-negative segments were mildly calcified. Two were in the proximal left anterior descending artery, one in the proximal left circumflex artery, and one at the mid-right coronary artery. There were 46 false-positive segments (2.7%) on CCTA that were mostly due to calcification obscuring the arterial lumen. Patient-based analysis showed that 12 patients had false-positive CCTA findings. leading to a positive predictive value of 87% and a suboptimal specificity of 69%. Nonetheless, the predictive accuracy (97% per segment and 90% per patient) was high ( Table 4 ).
| Parameter | Segment-based Analysis | Patient-based Analysis |
|---|---|---|
| Sensitivity | 141/145 (97%, 95–100%) | 82/82 (100%) |
| Specificity | 1,486/1,532 (97%, 96–98%) | 27/39 (69%, 55–84%) |
| Negative predictive value | 1,486/1,490 (99.7%, 99.5–100%) | 27/27 (100%) |
| Positive predictive value | 141/187 (75%, 69–82%) | 82/94 (87%, 81–94%) |
| Predictive accuracy | 1,627/1,677 (97%, 96–98%) | 109/121 (90%, 85–95%) |

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


