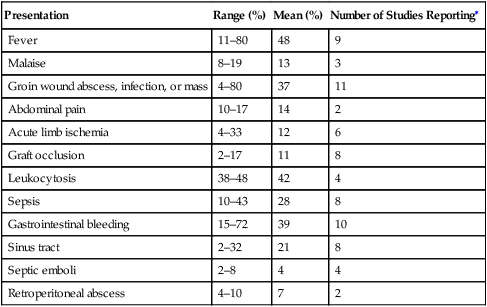
In general, aortic graft infections tend to manifest late and have a much broader potential spectrum of symptoms (Table 1). Infections caused by low-virulence organisms most commonly become manifest by a focal wound infection, a fluid collection, or a draining sinus tract. Systemic symptoms are very uncommon. Infections caused by high-virulence organisms manifest with systemic symptoms, and these can vary from being quite subtle with malaise, discomfort in the region of the prosthesis, or weight loss to the very obvious with fever, leukocytosis, bacteremia, and sepsis. False aneurysms can occur if infection has disrupted an anastomosis. TABLE 1 Spectrum of the Clinical Presentation of Aortic Graft Infection ∗Maximum is 13. The number of patients in these studies ranged from 18 to 68, with a mean of 38.
Diagnosis of Aortic Graft Infection
Presentation
Presentation
Range (%)
Mean (%)
Number of Studies Reporting∗
Fever
11–80
48
9
Malaise
8–19
13
3
Groin wound abscess, infection, or mass
4–80
37
11
Abdominal pain
10–17
14
2
Acute limb ischemia
4–33
12
6
Graft occlusion
2–17
11
8
Leukocytosis
38–48
42
4
Sepsis
10–43
28
8
Gastrointestinal bleeding
15–72
39
10
Sinus tract
2–32
21
8
Septic emboli
2–8
4
4
Retroperitoneal abscess
4–10
7
2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


