Previous studies have demonstrated ethnic/racial differences in cardiorespiratory fitness (CRF). However, the relative contributions of body mass index (BMI), lifestyle behaviors, socioeconomic status (SES), cardiovascular (CV) risk factors, and cardiac function to these differences in CRF are unclear. In this study, we included 2,617 Dallas Heart Study participants (58.6% women, 48.6% black; 15.7% Hispanic) without CV disease who underwent estimation of CRF using a submaximal exercise test. We constructed multivariable-adjusted linear regression models to determine the association between race/ethnicity and CRF, which was defined as peak oxygen uptake (ml/kg/min). Black participants had the lowest CRF (blacks: 26.3 ± 10.2; whites: 29.0 ± 9.8; Hispanics: 29.1 ± 10.0 ml/kg/min). In multivariate analysis, both black and Hispanic participants had lower CRF after adjustment for age and gender (blacks: Std β = −0.15; p value ≤0.0001, Hispanics: Std β = −0.05, p value = 0.01; ref group: whites). However, this association was considerably attenuated for black (Std β = −0.04, p value = 0.03) and no longer significant for Hispanic ethnicity (p value = 0.56) after additional adjustment for BMI, lifestyle factors, SES, and CV risk factors. Additional adjustment for stroke volume did not substantially change the association between black race/ethnicity and CRF (Std β = −0.06, p value = 0.01). In conclusion, BMI, lifestyle, SES, and traditional risk factor burden are important determinants of ethnicity-based differences in CRF.
Physical activity and high levels of cardiorespiratory fitness (CRF) are strongly associated with lower risk of cardiovascular (CV) disease. Previous studies have identified significant race/ethnic differences in CRF, with lower CRF in blacks than whites. This difference in CRF may contribute to the higher risk of CV disease (CVD) and associated mortality in blacks as compared with whites. Variation in CRF is associated with differences in age, gender, obesity, left ventricular volume, and physical activity. However, the explanation for the variation in CRF across race/ethnicities remains poorly understood. Although previous studies have attributed racial/ethnic differences in CRF levels to genetic factors, the contribution of body mass index (BMI), lifestyle behaviors, socioeconomic status (SES), CV risk factors and measures of cardiac function to these race/ethnic differences are not well understood. Therefore, we sought to characterize the contribution of these factors to the racial/ethnic differences in CRF among participants in the Dallas Heart Study (DHS).
Methods
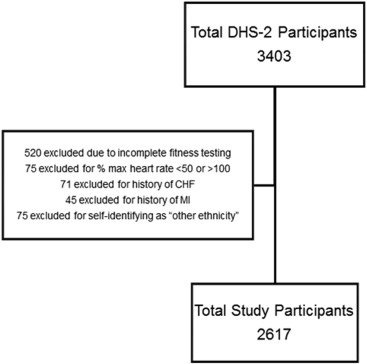
The DHS is a longitudinal, multiethnic population-based probability sample of Dallas County residents, with oversampling of self-reported black participants to ensure approximately 50% of black and non-black participants. Details of the study design and recruitment procedures have been previously described. The original cohort was enrolled from 2000 to 2002, and original participants and their spouses or significant others were invited to participate in phase 2 of the DHS in 2007 to 2009. At the DHS phase 2 examination, each participant completed a detailed staff-administered survey and underwent a health examination that involved measurement of blood pressure, anthropometry, blood and urine sample collection, and CRF testing as detailed in the Supplementary Material . The Institutional Review Board of the University of Texas Southwestern Medical Center approved the study. All participants provided written informed consent. For the present study, we included all DHS phase 2 participants without CVD who had available data on self-reported ethnicity/race and baseline CRF levels ( Figure 1 ).
Race/ethnicity was self-reported as non-Hispanic black, non-Hispanic white, Hispanic, or other according to US census categories. CRF was determined from estimated peak oxygen uptake (VO 2max ) using a submaximal exercise treadmill test using a protocol as described in the Supplementary Material . All DHS phase 2 participants also underwent physical activity level assessment using an accelerometer (Actical; Phyilips Respironics, Bend, Oregon) as previously reported. Moderate (3 to 6 metabolic equivalents) and vigorous (>6 metabolic equivalents) physical activity was quantified according to previously defined activity count thresholds that correspond to differences in exercise intensity. A subgroup of our study participants also underwent cardiac magnetic resonance imaging examination (N = 1,716) with short-axis, breath-hold, electrocardiographic-gated cine cardiac magnetic resonance imaging images using a 3-T system (Phillips Medical Systems, Best, the Netherlands). End-diastolic and end-systolic left ventricular volumes were calculated using the MASS software (Medis Medical Imaging Systems, Leiden, the Netherlands).
Baseline clinical and demographic characteristics were summarized across the 3 race/ethnicity categories (non-Hispanic blacks, non-Hispanic whites, and Hispanics) using percentage for categorical variable and mean ± SD for continuous variables. Participant characteristics were compared across the 3 race/ethnic groups using the chi-square test for categorical variables and Wilcoxon rank-sum test for continuous variables. Multivariable-adjusted linear regression analysis models were constructed to identify the significant clinical and demographic determinants of CRF. Model 1 was adjusted for age, gender, and race/ethnicity; model 2 was adjusted for all the variables in model 1 plus BMI; model 3 was adjusted for all the variables in model 2 plus physical activity, smoking, education, and annual income; model 4 was adjusted for all the variables in model 3 plus other CV risk factors including hypertension and diabetes status, systolic blood pressure, and blood glucose levels; model 5 was adjusted for all the variables in model 4 plus stroke volume at rest. Sensitivity analysis was also performed to evaluate the association between percentage African ancestry, as estimated from previously reported ancestry informative genetic markers and CRF using the most adjusted model 5.
For categorical analysis of the CRF data, all study participants were classified into data-derived age- and gender-specific quintiles of estimated VO 2max . These quintiles of CRF measures were then combined into 3 mutually exclusive CRF groupings: low fit (quintile 1), moderate fit (quintiles 2 to 4), and high fit (quintile 5). This was done to facilitate the comparisons of low fitness status across different racial/ethnic groups. Association of race/ethnicity with likelihood of low baseline CRF was assessed using multivariable-adjusted logistic regression analysis with adjustment for all covariates included in model 5 (age, gender, race/ethnicity, BMI, physical activity, education, annual income, hx. of hypertension, diabetes status, systolic blood pressure, blood glucose levels, and stroke volume). All statistical analysis was performed using SAS, version 9.2 (SAS Institute Inc., Cary, North Carolina).
Results
We included 2,617 participants (58.6% women, 48.6% black, 35.7% white, 15.7% Hispanic). Baseline clinical and demographic characteristics of the study participants across racial/ethnic groups are listed in Table 1 . Blacks had higher BMI, systolic blood pressure, and smoking prevalence, and lower annual income compared with whites and Hispanics. Mean CRF and the proportion of participants meeting guideline recommended minimum physical activity levels were also lower among blacks. In unadjusted analyses, the prevalence of low CRF, defined as estimated VO 2max in the lowest age- and gender-adjusted quintile for the study population, was significantly higher in blacks (25%) as compared with whites (12%) and Hispanics (17%; Figure 2 ).
| Variable | Blacks (N = 1,274) | Whites (N = 933) | Hispanics (N = 410) |
|---|---|---|---|
| Age (years) | 48.0 ± 10.8 | 51.4 ± 10.4 | 45.5 ± 10.2 |
| Women | 62.6% | 53.7% | 57.6% |
| Body Mass Index (kg/m 2 ) | 32.0 ± 7.6 | 29.2 ± 6.1 | 30.6 ± 6.0 |
| Total Percent Body Fat | 37.4 ± 9.6 | 37.0 ± 8.4 | 38.3 ± 8.1 |
| Systolic blood pressure (mm Hg) | 135.5 ± 19.9 | 127.1 ± 16.4 | 126.1 ± 16.5 |
| Glucose (mg/dl) | 99.5 ± 35.7 | 97.8 ± 22.9 | 105.6 ± 39.9 |
| High-density lipoprotein- Cholesterol, (mg/dl) | 54.1 ± 14.9 | 52.9 ± 15.9 | 48.4 ± 12.4 |
| Education (years) | 12.7 ± 1.4 | 13.5 ± 1.7 | 10.9 ± 3.4 |
| Moderate to vigorous Physical activity (min/day) | 39.2 ± 35.7 | 38.4 ± 33.4 | 57.1 ± 43.2 |
| Sedentary time (min/day) | 304.3 ± 96.5 | 311.7 ± 96.3 | 258.1 ± 94.9 |
| Fitness (ml/kg/min) | 26.3 ± 10.2 | 29.0 ± 9.8 | 29.1 ± 10.0 |
| Smoker | 26.3% | 18.3% | 17.3% |
| Annual Income ∗ | |||
| <$20K | 26.6% | 7.6% | 21.5% |
| $20K to <$40K | 28.2% | 17.5% | 35.2% |
| $40K to <$75K | 22.3% | 31.8% | 19.3% |
| >=$75K – <$100K | 7.2% | 21.6% | 6.1% |
| >=$100K | 5.8% | 14.1% | 12.2% |
∗ The percent proportions for annual income categories doesn’t add up to 100% due to missing data in a small proportion of the study participants.
After adjustment for demographic characteristics, blacks and Hispanics had significantly lower CRF than whites ( Table 2 , model 1). After further adjustment for BMI, the association between race/ethnicity and CRF attenuated among blacks and was no longer significant for Hispanics ( Table 2 , model 2). Further attenuation in the association between race/ethnicity and CRF was observed among blacks with additional adjustment for lifestyle factors, SES ( Table 2 , model 3), and other established CV risk factors including hypertension and diabetes status, systolic blood pressure level, and blood glucose levels ( Table 2 , model 4). These associations were not significantly different after additional adjustment for baseline measures of stroke volume ( Table 2 , model 5). Among other characteristics, older age, higher BMI, smoking, lower levels of physical activity, and smaller stroke volume were independently associated with lower levels of CRF ( Supplementary Table 1 ). Similar associations were also observed race/ethnicity and CRF in multivariable-adjusted logistic regression analysis in with low CRF as a categorical outcome variable ( Figure 3 ). No significant interaction was observed between race/ethnicity and BMI (p-interaction for black race × BMI = 0.66) or age (p-interaction for black race × age = 0.20) for CRF. To confirm the robustness of our observed associations between self-reported black race/ethnicity and CRF, we performed additional analysis evaluating the association between percentage African ancestry and CRF after adjustment for potential cofounders. We observed a significant inverse association between percent African ancestry and CRF (Std β = −0.08, p value = 0.02) in the most adjusted model, similar to that observed between self-reported black race/ethnicity and CRF.
| Model R 2 | Blacks (vs. Whites) | Hispanics (vs. Whites) | |||
|---|---|---|---|---|---|
| Std β | P -value | Std β | P -value | ||
| Model 1 | 0.22 | -0.15 | < .0001 | -0.05 | 0.01 |
| Model 2 | 0.28 | -0.09 | < .0001 | -0.03 | 0.08 |
| Model 3 | 0.29 | -0.06 | 0.001 | 0.003 | 0.88 |
| Model 4 | 0.32 | -0.04 | 0.03 | 0.01 | 0.56 |
| Model 5 | 0.35 | -0.06 | 0.01 | 0.02 | 0.27 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


