Receptor
Ligands
TLR1
Bacterial lipoproteins
TLR2
Lipopeptides, lipoteichoic acid
TLR3
Double-stranded RNA
TLR4
Lipopolysaccharides
TLR5
Flagellin
TLR6
Lipopeptides
TLR7/TLR8
Imidazoquinolines, single-stranded RNA
TLR9
Unmethylated CpG DNA
TLR10
Unknown
NOD-like receptor
Ligands
NOD1, NOD2
Peptidoglycan derivatives
Twenty types of these receptors have been identified. They are involved in detection of bacterial pathogens. Two NLR types—NOD1 and NOD2—recognize bacterial peptidoglycan from Gram-positive bacteria and activate nuclear factor (NF)-κΒ, which generates an increase in interleukin (IL)-1. This is an important way of controlling intracellular bacteria such as L. pneumophila.
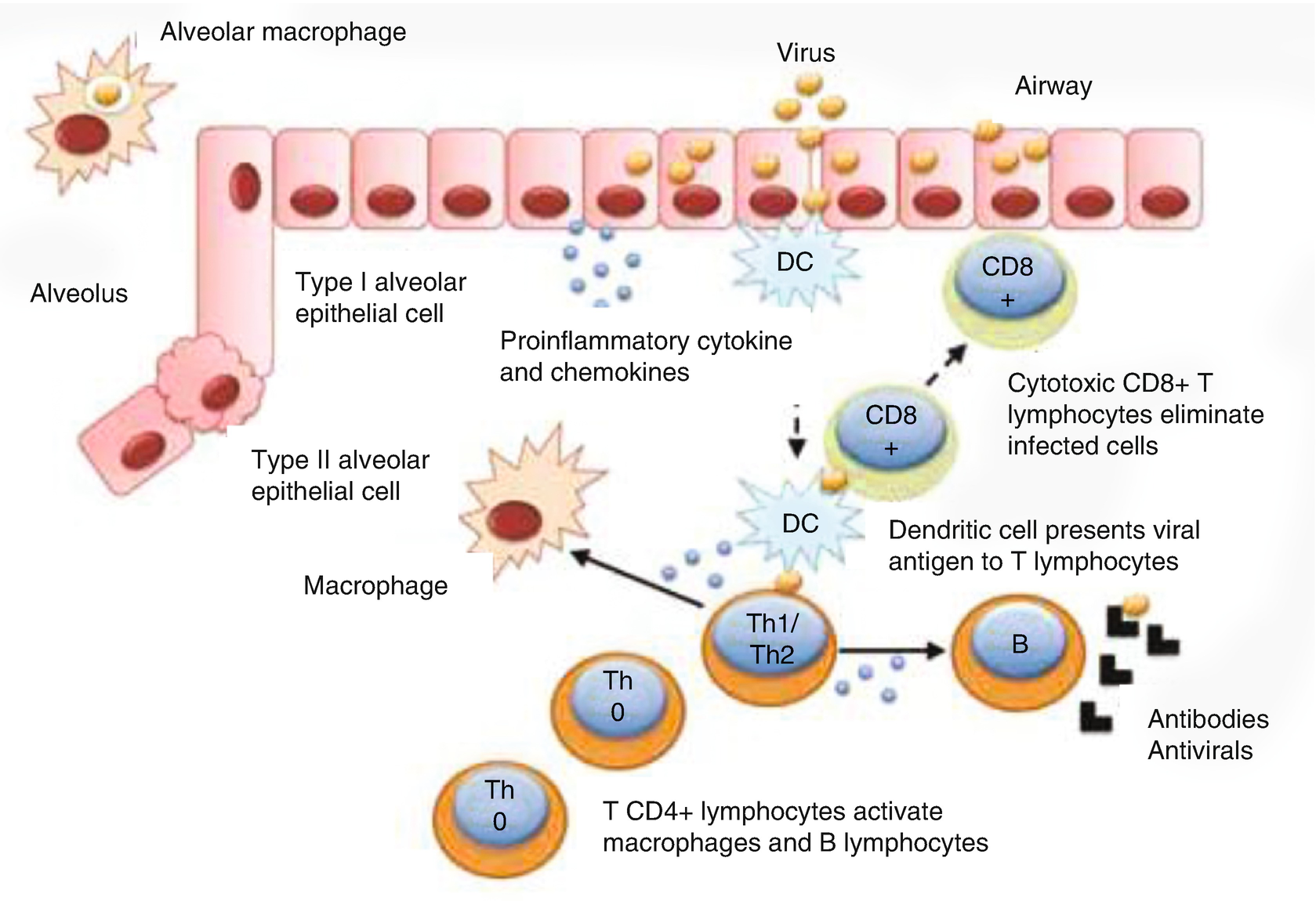
Many types of cell participate in the innate immune response of the respiratory system.
Type 2 alveolar cells express TL2 and TL4, contributing to the response to lipopolysaccharides and bacterial peptidoglycans.
The epithelial cells of the airway express TLR1–TLR10, and their stimulation increases the production of various proinflammatory cytokines.
Neutrophils are recruited rapidly by the production of proinflammatory mediators such as B4 leukotriene, C5a, and IL-8. Pathogens are then phagocytized. Neutrophils have a short half-life; after their apoptosis, they trigger an anti-inflammatory response and restore the normal architecture of the epithelium.
There are macrophages in the interstice and the alveolus. Alveolar macrophages are located in the surfactant in the air–lung tissue interface, and this location allows them to be the first barrier of defense against inhaled pathogens and environmental toxins. They are involved in phagocytic activity, starting an inflammatory cascade and participating as antigen-presenting cells before being replaced by monocytes.
Dendritic cells play a fundamental role in the interface between the innate immune response and the adaptive immune response. They have the ability to capture antigens and, through damage-associated molecular pattern (DAMP) stimulation, they migrate toward the lymph node and present the antigens to activate T cells.
Adaptive Immunity
For many years, our understanding of cellular immunity in the lungs has been simplified, divided only into Th1 and Th2 responses; however, it is now understood that there are other kinds of cellular response, forming a system that is more diverse and complex. Th1 immunity (mediated by T CD4+ lymphocytes, which secrete cytokines such as interferon (IFN)-γ, IL-6, and IL-12) is fundamental in defense against environmental pathogens, both bacterial and viral. In particular, it plays a fundamental role in defense against intracellular bacteria such as Mycobacterium tuberculosis. The Th2 response is mediated by T CD4 lymphocytes, which secrete mainly IL-4, IL-5, and IL-13. Its main function is defense against helminths, but it also takes part in defense against viral pathogens and in immune system regulation. Th2 immunity is possibly better known for its pathogenic role; it is central to generation of allergic responses mediated by IgE, which can trigger asthma and allergic rhinitis, as in excessive immune responses to some respiratory viruses such as RSV.
Our understanding of the Th1–Th2 balance has been modified since the discovery of the Th17 immune response, which is essential for defense against extracellular bacteria and plays an important role in diverse inflammatory illnesses. Differentiation of T lymphocytes into Th17 lymphocytes is provoked by the combination of IL-6, IL-1β, and IL-23. Once the response has been activated, large amounts of IL-17 are produced. This cytokine participates in the mobilization of neutrophils and plays an essential role in the elimination of pathogens in the airway. It has been observed that there is an inhibitory interaction between the different responses: Th1 cytokines inhibit Th2 and Th17 responses, and Th2 cytokines inhibit Th1 and Th17 responses. The inflammatory response provoked by Th17 can participate in the pathogenesis of bronchial asthma. There is a relationship between the production of Th17 cells and regulator T cells; when T cell production is inhibited by IL-6, the differentiation into Th17 increases. Once the levels of proinflammatory cytokines increase, the regulator T cell population starts to grow to re-establish the basal state.
Regulatory T lymphocytes (Tregs) play a fundamental role in the regulation of the peripheral immune response of T lymphocytes; other mediators also participate: IL-10, transforming growth factor (TGF)-β, and nitrous oxide. Tregs have a fundamental function in the regular postviral inflammatory response (helping to avoid sequelae of postviral infections) and in modulation of tolerance of aeroallergens to avoid allergic illnesses.
Immune Responses to Respiratory Infections

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


