There are three causes of decreased automaticity:
1. Physiologic slowing of the sinus rate.
2. Physiologic or pathologic enhancement of parasympathetic nervous activity.
3. Pathologic pacemaker failure
MECHANISMS OF BRADYARRHYTHMIAS OF DECREASED AUTOMATICITY
Physiologic Slowing of the Sinus Rate
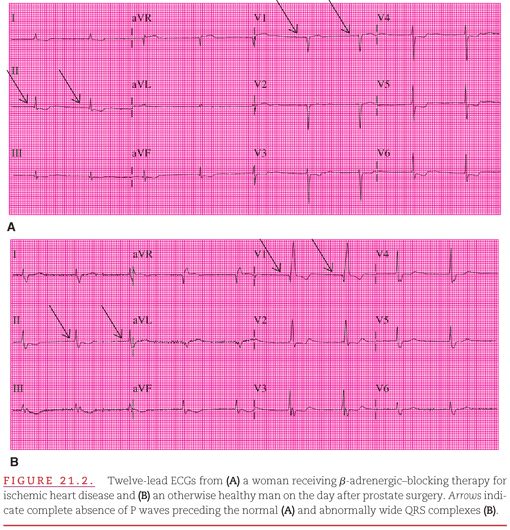
Although a rate of <60 beats per minute is technically termed a “bradyarrhythmia,” it is often a normal variation of cardiac rhythm (especially in trained athletes, whose heart rates may be as low as in the 30s of beats per minute at rest). The rhythm may be either sinus bradycardia or, as shown in Figure 21.2, a junctional (see Fig. 21.2A) or ventricular (see Fig. 21.2B) escape rhythm. Bradycardia is a physiologic reaction to relaxation or sleep, when the parasympathetic effect on cardiac automaticity dominates over the sympathetic effect. Even during the expiratory phase of the respiratory cycle, there is slowing of the sinus rate, often into the bradycardic range (see Fig. 3.15). The lead V1–positive QRS complexes in Figure 21.2B indicate that the escape site is in the left bundle.
Physiologic or Pathologic Enhancement of Parasympathetic Activity
All cells with pacemaking capability are under some influence of the sympathetic and parasympathetic divisions of the autonomic nervous system. This influence is greatest in the sinus node and diminishes in the lower sites with pacemaking capacity. Usually, the changing autonomic balance causes a gradual increase or decrease in the pacing rate. However, many factors can induce a sudden increase in parasympathetic activity and decrease in sympathetic activity. These factors include:
1. Carotid sinus massage.
2. Hypersensitivity of the carotid sinus.
3. Straining (i.e., a Valsalva maneuver).
4. Ocular pressure.
5. Increased intracranial pressure.
6. Sudden movement from a recumbent to an upright position.
7. Drugs that cause pooling of blood by dilating the veins.
This increase in parasympathetic activity is termed a vasovagal reaction (vasovagal reflex) because it has a prominent component of vascular relaxation in addition to cardiac slowing and because it is mediated by the vagus nerve. Typical bradyarrhythmias that occur suddenly during a vasovagal reaction are presented in Figure 21.3. A sudden increase in parasympathetic activity is manifested by both slowing of the sinus rate and failure of atrioventricular (AV) conduction (note the nonconducted P wave in the electrocardiogram [ECG] shown in Fig. 21.3). The increase in parasympathetic activity also suppresses escape pacemakers, and the resulting pause is interrupted only by the return of sinus rhythm. The combination of vascular relaxation and cardiac slowing results in a reduction in cardiac output so severe that it may cause dizziness or even loss of consciousness. This is termed vasovagal syncope or fainting. It is typically reversed when the individual falls into a recumbent position, thereby increasing venous return to the heart. When a person who has fainted is encountered, consciousness can usually be restored by lowering the head and chest and elevating the legs.
A single physiologic vasovagal reaction can have severe pathologic consequences if the individual is injured during a consequent fall or if the change in body position required to restore venous return to the heart is not possible. Indeed, the autonomic reflex itself may become pathologic, resulting in neurocardiogenic syncope.1–3 Repeated, severe, and sudden episodes of bradyarrhythmia with vasodilation require medical intervention to prevent serious injury or death.
Pathologic Pacemaker Failure
When a sudden period of complete absence of P waves appears in the ECG, the term asystole is used. The term sick sinus syndrome is often applied to this situation; it is tempting to attribute the problem solely to the sinus node and pathologic pacemaker failure. However, if the problem was indeed limited to the sinus node, it would not produce any serious bradyarrhythmia because a 1- to 2-second pause in sinus rhythm would be interrupted by escape from a lower site with the capacity for impulse formation (Fig. 21.4). After three sinus beats (see Fig. 21.4A), there is no further evidence of atrial activity, but then two junctional escape beats result. The pause following a ventricular premature beat (see Fig. 21.4B) ends with a junctional escape beat. After three sinus beats (see Fig. 21.4C), a nonconducted atrial premature beat (APB) provides a cycle long enough for the ventricular Purkinje system to provide an escape beat. Therefore, a prolonged atrial pause is caused by either:
1. Enhanced parasympathetic activity or
2. Impairment of all cells with impulse formation capability.
Although “sick pacemaker syndrome” would be a more accurate term, “sick sinus syndrome” is used here because of its general acceptance. Its characteristics are:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


