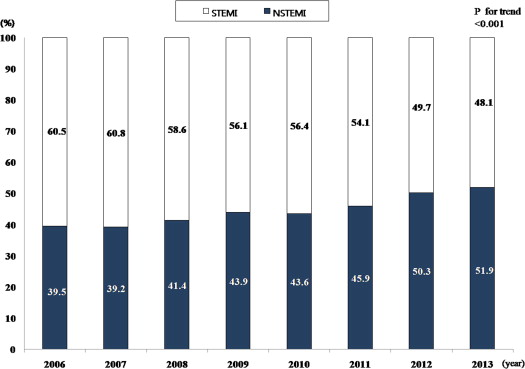
Although the incidence of acute myocardial infarction (AMI) in Korea has been rapidly changed because of westernization of diet, lifestyle, and aging of the population, the recent trend of the myocardial infarction have not been reported by classification. We investigated recent trends in the incidence and mortality associated with the 2 major types of AMI. We reviewed 39,978 patients registered in the Korea Acute Myocardial Infarction Registry for either ST-segment elevation acute myocardial infarction (STEMI) or non–ST-segment elevation acute myocardial infarction (NSTEMI) from 2006 to 2013. When the rate for AMI were investigated according to each year, the incidence rates of STEMI decreased markedly from 60.5% in 2006 to 48.1% in 2013 (p <0.001). In contrast, a gradual increase in the incidence rates of NSTEMI was observed from 39.5% in 2006 to 51.9% in 2013 (p <0.001). As risk factors, hypertension, diabetes mellitus, and dyslipidemia were much more common in patients with NSTEMI than STEMI. Among medical treatments, the use of β blockers, angiotensin receptor blocker, and statin were increased from 2006 to 2013 in patients with STEMI and NSTEMI. Patients with STEMI and NSTEMI were more inclined to be increasingly treated by invasive treatments with percutaneous coronary intervention. In conclusion, this study demonstrated that the trend of myocardial infarction has been changed rapidly in the aspect of risk factors, ratio of STEMI versus NSTEMI, and therapeutic strategies during the recent 8 years in Korea.
Previous studies have not investigated ST-elevation myocardial infarction (STEMI) and non–ST-elevation myocardial infarction (NSTEMI) separately in the past years, although the management and outcomes of these entities differ markedly. Therefore, this study attempted to overview the general aspect of alteration in Koreans with 2 major types of acute myocardial infarction (AMI) by annual analysis using the database of the Korea Acute Myocardial Infarction Registry (KAMIR).
Methods
KAMIR is the first nationwide, registry-observed, prospective, multicenter, online data collection study designed to reflect the “real world” clinical field in Korean patients presenting with AMI and also to investigate the risk factors, incidence, and mortality of patients with AMI with the support of the Korean Circulation Society from November 2005. We enrolled patients who were diagnosed with AMI, including both patients with STEMI and NSTEMI. The diagnosis of AMI was based on a typical increase and decrease of biochemical markers of myocardial necrosis (including creatine kinase-MB and troponin I and T) with at least 1 of the following: ischemic symptoms, electrocardiographic changes indicative of ischemia (ST-segment elevation or depression), and development of pathologic Q waves on the electrocardiogram.
The study population was derived from patients in the KAMIR enrolled from January 2006 to December 2013. We identified 39,978 patients with STEMI and NSTEMI, and eligible patients (24,949 men and 10,039 women, age = 65.2 ± 12.9 years) were classified based on hospital arrival time on a yearly basis. Demographics (age, gender, and body mass index), conventional risk factors of AMI (hypertension, diabetes mellitus, dyslipidemia, smoker, and previous angina pectoris), baseline clinical characteristics (chest pain, dyspnea, Killip class, and the presence of percutaneous coronary intervention), and in-hospital mortality were investigated. Hypertension was defined as a previous diagnosis or antihypertensive medication use, and diabetes was defined as a previous diagnosis of diabetes and use of insulin or oral hypoglycemic agents on initiation into the study. Dyslipidemia was defined as a diagnosis previously confirmed by physician or by treatment with lipid-lowering medications. The detailed definition of other variables has been previously described in published article using the KAMIR study.
The present study was run according to the Declaration of Helsinki. The institutional review board of all participating centers approved the study protocol. The approval number was 05-49 of Chonnam National University Hospital. Written informed consent was obtained from all participating patients.
For the comparison of demographics, risk factors, clinical characteristics, and in-hospital mortality between the patients with STEMI and NSTEMI, the chi-square test and independent t test were used, as appropriate. Also for the trend analysis of demographics, risk factors, medical treatment, and mortality, according to type of AMI from 2006 to 2013, linear-by-linear association test was conducted. All statistical analyses were performed using SPSS for Windows version 21.0 (IBM SPSS Statistics for Windows, Armonk, New York; IBM Corporation). Two-tailed p <0.05 was considered to indicate a significant difference.
Results
A total of 39,978 patients were hospitalized with confirmed AMI during the 8 years. The subjects with STEMI accounted for 56.3% (22,514), and those with NSTEMI accounted for 43.7% (17,464) of all patients. However, when the trend for AMI was investigated according to the year, the proportion of 2 types of AMI was significantly reversed. Interestingly, the incidence rates of STEMI decreased markedly from 60.5% in 2006 to 48.1% in 2013 ( Figure 1 ). On the contrary, the incidence of NSTEMI was gradually increased from 39.5% in 2006 to 51.9% in 2013 ( Figure 1 ). Finally, the incidence rates for NSTEMI overtook STEMI at 2012 and steadily increased in the following year ( Figure 1 ).
Among risk factors, male gender, overweight, and smoking were greater in patients with STEMI than in those with NSTEMI, whereas age, hypertension, diabetes mellitus, dyslipidemia, and previous angina pectoris history were lesser ( Table 1 ). In the trend analysis since the year 2006, the number of patients of male gender with hypertension, diabetes mellitus, and dyslipidemia were gradually and significantly increased, and the patients with overweight, smoking history, and previous angina pectoris history were significantly decreased in both STEMI and NSTEMI groups ( Table 2 ).
| Variables | STEMI (n=22,514) | NSTEMI (n=17,464) | p value |
|---|---|---|---|
| Age (mean yrs, SD) | 64.1±13.2 | 66.5±12.5 | <0.001 |
| Men | 16,823 (74.8%) | 11,715 (67.2%) | <0.001 |
| Body mass index (mean ± SD; kg/m 2 ) | 24.0±3.4 | 23.9±3.4 | 0.831 |
| Body mass index ≥ 23 | 7,541 (37.5%) | 5,773 (36.4%) | 0.029 |
| Hypertension | 10,390 (48.9%) | 9,596 (58.4%) | <0.001 |
| Diabetes mellitus | 5,548 (26.2%) | 5,546 (33.8%) | <0.001 |
| Dyslipidemia | 2,221 (10.5%) | 2,227 (13.6%) | <0.001 |
| Smoker | 11,324 (51.2%) | 6,828 (39.8%) | <0.001 |
| Previous angina pectoris | 7,278 (32.9%) | 7,512 (43.8%) | <0.001 |
| Chest pain | 19,287 (86.9%) | 13,041 (75.9%) | <0.001 |
| Dyspnea | 5,021 (22.9%) | 4,649 (27.2%) | <0.001 |
| Percutaneous coronary intervention | 20,882 (93.1%) | 13,670 (78.5%) | <0.001 |
| Killip class (≥III) | 3,188 (15.0%) | 2,178 (13.3%) | <0.001 |
| In-hospital mortality | 1,310 (5.9%) | 637 (3.7%) | <0.001 |
| Variables | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | p for trend | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | STEMI (n=22,477) | 62.3±12.8 | 62.8±12.9 | 66.7±13.2 | 65.8±12.9 | 64.9±13.1 | 63.6±13.1 | 63.0±14.4 | 62.1±12.4 | <0.001 |
| NSTEMI (n=17,444) | 64.7±12.3 | 65.2±12.3 | 69.0±12.3 | 68.3±12.4 | 67.4±12.2 | 66.6±12.3 | 64.8±12.2 | 64.9±12.6 | <0.001 | |
| STEMI | 2,884 (74.2%) | 2,363 (73.5%) | 2,623 (73.7%) | 2.377 (74.6%) | 1,903 (73.9%) | 1,888 (76.7%) | 1,523 (77.6%) | 1,262 (77.3%) | <0.001 | |
| Men | ||||||||||
| NSTEMI | 1,657 (65.3%) | 1,369 (66.2%) | 1,632 (64.9%) | 1,680 (67.3%) | 1,360 (68.3%) | 1,406 (67.5%) | 1,382 (69.6%) | 1,229 (69.8%) | <0.001 | |
| Body mass index ≥ 23 | STEMI | 1,483 (41.2%) | 1,205 (41.4%) | 1,156 (36.8%) | 915 (35.1%) | 790 (35.5%) | 890 (36.4%) | 643(34.6%) | 540 (35.0%) | <0.001 |
| NSTEMI | 975 (41.1%) | 755 (39.9%) | 777 (34.5%) | 755 (35.8%) | 609 (34.9%) | 661 (34.7%) | 648 (34.2%) | 593 (35.1%) | <0.001 | |
| Chest pain | STEMI | 3,392 (89.2%) | 2,810 (89.1%) | 3,050 (86.5%) | 2,687 (85.5%) | 2,159 (84.7%) | 1,986 (81.4%) | 1,713 (87.7%) | 1,490 (91.3%) | <0.001 |
| NSTEMI | 975 (41.1%) | 755 (39.9%) | 777 (34.5%) | 755 (35.8%) | 609 (34.9%) | 661(34.7%) | 648 (34.2%) | 593 (35.1%) | 0.023 | |
| Dyspnea | STEMI | 957 (26.0%) | 770 (24.8%) | 837 (23.8%) | 633 (20.3%) | 603 (23.9%) | 446 (18.4%) | 420 (21.5%) | 355 (21.8%) | <0.001 |
| NSTEMI | 801(33.3%) | 546 (26.9%) | 675 (27.3%) | 636 (26.1%) | 510 (26.1%) | 461 (22.5%) | 558 (28.1%) | 462 (26.2%) | <0.001 | |
| Hypertension | STEMI | 1,753 (45.3%) | 1,453 (45.4%) | 1,670 (47.6%) | 1,456 (46.5%) | 1,206 (47.5%) | 1,172 (49.1%) | 920 (62.8%) | 760 (66.7%) | <0.001 |
| NSTEMI | 1,365 (53.9%) | 1,118 (54.3%) | 1,392 (56.3%) | 1,382 (56.0%) | 1,094 (56.1%) | 1,169 (57.6%) | 1,097 (69.4%) | 979 (73.4%) | <0.001 | |
| Diabetes mellitus | STEMI | 951 (24.6%) | 794 (24.8%) | 878 (25.0%) | 771 (24.6%) | 616 (24.3%) | 622 (26.1%) | 505 (34.5%) | 411 (36.1%) | <0.001 |
| NSTEMI | 821 (32.5%) | 664 (32.2%) | 788 (31.8%) | 772 (31.3%) | 644 (33.0%) | 637 (31.4%) | 667 (42.2%) | 553 (41.5%) | <0.001 | |
| Dyslipidemia | STEMI | 238 (6.2%) | 310 (9.7%) | 370 (10.6%) | 298 (9.5%) | 338 (13.4%) | 288 (12.1%) | 200 (13.7%) | 179 (15.7%) | <0.001 |
| NSTEMI | 265 (10.5%) | 281 (13.7%) | 366 (14.8%) | 298 (12.1%) | 287 (14.8%) | 279 (13.8%) | 227 (14.4%) | 224 (16.8%) | <0.001 | |
| Smoker | STEMI | 2,380 (62.0%) | 1,922 (60.4%) | 1,653 (47.5%) | 1,475 (47.4%) | 1,166 (46.6%) | 1,129 (46.9%) | 871 (44.6%) | 728 (44.6%) | <0.001 |
| NSTEMI | 1,285 (51.1%) | 1,048 (51.3%) | 963 (39.4%) | 889 (36.7%) | 674 (34.8%) | 671 (32.9%) | 690 (34.9%) | 608 (34.5%) | <0.001 | |
| Previous angina pectoris | STEMI | 1,467(38.3%) | 1,170 (37.0%) | 1,233 (35.2%) | 953 (30.8%) | 826 (32.6%) | 804 (33.3%) | 461 (23.7%) | 364 (22.3%) | <0.001 |
| NSTEMI | 1,199 (47.7%) | 1081 (52.9%) | 1,134 (46.0%) | 1,015 (42.1%) | 888 (45.7%) | 964 (47.2%) | 671 (33.9%) | 560 (31.8%) | <0.001 | |
| Aspirin | STEMI | 3,508 (90.2%) | 2,838 (88.2%) | 3,047 (97.7%) | 2,792 (98.6%) | 2,211 (99.2%) | 2,084 (99.1%) | 1,837 (97.2%) | 1,570 (96.2%) | <0.001 |
| NSTEMI | 2,314 (91.0%) | 1,822 (87.9%) | 2,199 (96.5%) | 2,181 (97.4%) | 1,724 (97.8%) | 1,831 (97.1%) | 1,856 (96.6%) | 1,684 (95.6%) | <0.001 | |
| Clopidogrel | STEMI | 3,398 (87.4%) | 2,745 (85.3%) | 2,997 (84.1%) | 2,751 (86.0%) | 2,174 (84.0%) | 2070 (84.0%) | 1723(87.8%) | 1067 (65.4%) | <0.001 |
| NSTEMI | 2,108 (82.9%) | 1,655 (79.9%) | 2,064 (82.1%) | 2,072 (82.8%) | 1,610 (80.7%) | 1,718 (82.3%) | 1,720 (86.5%) | 1,283 (72.8%) | <0.001 | |
| Cilostazol | STEMI | 1,374 (35.3%) | 865(26.9%) | 803(27.4%) | 874 (32.9%) | 525 (24.4%) | 454 (22.2%) | 365 (19.4%) | 122 (7.5%) | <0.001 |
| NSTEMI | 771 (30.3%) | 469 (22.6%) | 556 (26.2%) | 561 (26.6%) | 365 (21.4%) | 414 (22.4%) | 374 (19.5%) | 168 (9.5%) | <0.001 | |
| Beta blocker | STEMI | 2,500 (64.3%) | 2,120 (65.9%) | 2,386 (67.0%) | 2,375 (74.3%) | 1,938 (74.9%) | 1,797 (72.9%) | 1,614 (82.2%) | 1,352 (82.8%) | <0.001 |
| NSTEMI | 1,684 (66.2%) | 1,329 (64.1%) | 1,703 (67.8%) | 1,803 (72.1%) | 1,448 (72.5%) | 1,511 (72.4%) | 1,559 (78.4%) | 1,440 (81.7%) | <0.001 | |
| Angiotensin converting enzyme inhibitor | STEMI | 2,411 (62.0%) | 1,938 (60.2%) | 2,066 (58.0%) | 1,721 (53.8%) | 1,364 (52.7%) | 1,053 (42.7%) | 941 (47.9%) | 961 (58.9%) | <0.001 |
| NSTEMI | 1,505 (59.2%) | 1,205 (58.2%) | 1,337 (53.2%) | 1,247 (49.8%) | 963 (48.2%) | 874 (41.9%) | 757 (38.1%) | 834 (47.3%) | <0.001 | |
| Angiotensin receptor blocker | STEMI | 607 (15.6%) | 376 (11.7%) | 523 (14.7%) | 685 (21.4%) | 502 (19.4%) | 631 (25.6%) | 596 (30.4%) | 345 (21.1%) | <0.001 |
| NSTEMI | 1,060 (16.5%) | 662 (12.5%) | 998 (16.4%) | 1,306 (22.9%) | 962 (21.0%) | 1,257 (27.6%) | 1,336 (33.8%) | 903 (26.6%) | <0.001 | |
| Statin | STEMI | 2,718 (69.9%) | 2,128 (66.1%) | 2,380 (66.8%) | 2,188 (68.4%) | 1,731 (66.9%) | 1,799 (73.0%) | 1,635 (83.3%) | 1,460 (89.5%) | <0.001 |
| NSTEMI | 1,693 (66.6%) | 1,362 (65.7%) | 1,609 (64.0%) | 1,622 (64.8%) | 1,315 (65.9%) | 1,601 (76.7%) | 1,634 (82.2%) | 1,558 (88.4%) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


