Vigilance against respiratory virus infections
Respiratory virus
Etiology and Physiopathology
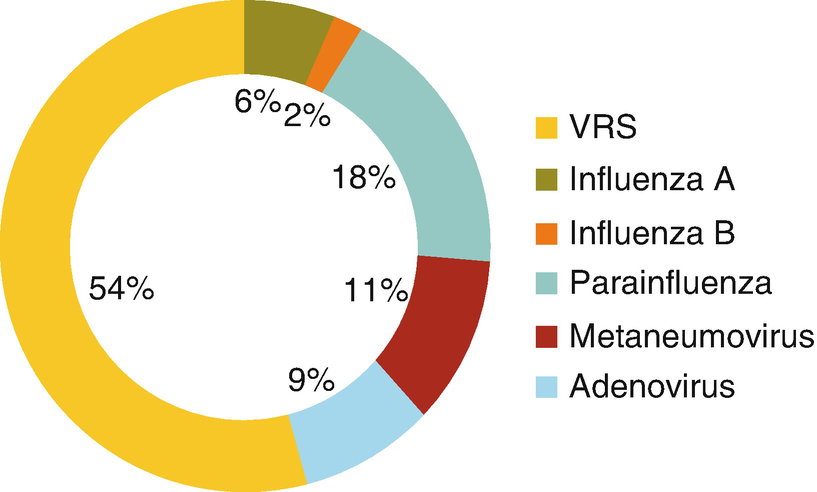
The most common etiological agents are parainfluenza viruses 1 and 3. Less common agents are parainfluenza 2, influenza viruses A and B, RSV, adenovirus, measles, and Mycoplasma pneumoniae.
Parainfluenza is a single-strand, enveloped RNA virus that belongs to the Paramyxoviridae family. It is pleomorphic, measures between 100 and 200 nm, and has six proteins. There are four types of parainfluenza virus, the most common of which are types 1–3. Types 1 and 2 generally produce acute or obstructive laryngitis, while type 3 produces infections of the lower respiratory tract, such as bronchitis and pneumonia. Type 4 is less often detected and can cause upper and lower respiratory infections.
The HN glycoprotein adheres to the host cell and facilitates F protein initiation of virus–cell membrane fusion. It also facilitates the binding of the nucleocapsid (formed by NP, P, and L proteins linked to the viral genome) to the genome of the host cell, thus initiating viral replication. In addition to its basic proteins, the parainfluenza virus expresses other proteins such as C, V and D. V and C neutralize innate immunity through suppression of activity by interferon 1.
Initially, the virus infects epithelial cells of the nose and oropharynx, and then it extends to the cell cilia and bronchial epithelial alveoli, as well as to the large and small airways. Viral replication peaks at 2–5 days and begins to decline by the seventh day.
Cellular or tissue damage is fundamentally caused by the host response, with minimal direct cytopathic effects of the virus itself. It induces an innate immune response with production of CD4 and CD8, interferon, and local and systemic immunoglobulin A and immunoglobulin G, all of which contribute to elimination of the virus. The hyperresponsiveness that is often seen in patients may be due to immunoglobulin E production and histamine release.
The result of this process is diffuse inflammation of the airway, with a greater intensity at the levels of the larynx and trachea, particularly in the subglottic space. This causes a reduction of the lumen and increased resistance to the entry of air in the lungs, resulting in greater work of breathing and appearance of the cardinal sign, a stridor.
Clinical Manifestations
After an incubation period of 2–7 days in the case of parainfluenza virus, the patient presents coryza and a fever, which can be high or low, and in 24–48 hours the characteristic signs appear: a barking cough and a stridor. If the edema and narrowing of the airway increase, the breathing rate rises, the patient becomes increasingly more agitated (to the extent that respiration is more difficult), and the use of accessory musculature appears, with suprasternal drainage, intercostal and subcostal retraction, and even cyanosis. Changes in the mental state occur in this phase, with agitation or lethargy. The patient is unable to cry or speak, and there is no stridor and no air entering the lungs, but there is a paradoxical movement of the chest, with signs of hypoxemia and respiratory failure.
Fortunately, the majority of cases of acute obstructive laryngitis are mild and resolve within 7 days, although coughing can continue for weeks.
Severity Scores
There are different severity scores to assess the seriousness of the clinical picture, such as the Downes score and the Wesley score, the latter being the most often used for studies.
Downes Score
Grade I—mild: stridor during crying or activity, absence of retraction
Grade II—moderate: inspiratory stridor at rest, suprasternal and intercostal retraction at rest, but without agitation
Grade III—severe: major inspiratory or biphasic stridor, with marked suprasternal and intercostal retraction, and with agitation; signs of respiratory difficulty
Grade IV—imminent respiratory failure: weak cough , altered level of consciousness, signs of hypoxemia
Westley Score
Stridor :
0: absent
1: during crying
2: at rest
Retraction:
0: absent
1: slight
2: moderate
3: severe
Entry of air:
0: normal
1: reduced but audible
2: very reduced, hardly audible
Cyanosis (O2 saturation <92%; fraction of inspired oxygen (FiO2) 0.21):
0: absent
4: with agitation
5: at rest
Level of awareness:
0: normal
5: diminished
Total score: 0–1 = mild; 2–7 = moderate; ≥8 = severe
Diagnostic Focus
The diagnosis is clinical. A virus identification study is sometimes requested in severe cases, which can include a viral etiological study of a respiratory sample (either a nasopharyngeal swab, nasopharyngeal aspirate, bronchoalveolar lavage fluid, or tracheal aspirate). The parainfluenza virus can be identified by direct immunofluorescence or polymerase chain reaction (PCR). There are rapid immunochromatographic tests for RSV, influenza, and adenoviruses.
X-ray examinations are done only when there is suspicion of a differential diagnosis.
The airway is assessed endoscopically only in severe cases in which an adequate response to the established therapy is not observed and significant obstructive symptoms persist after 48 hours of treatment.
Differential diagnosis: In general, the other diagnostic alternatives are much less common but, because they require other assessments and/or treatments, the clinician should always keep them in mind, especially if the patient does not evolve as expected.
Bacterial tracheitis
Epiglottis
Retro- or parapharyngeal abscess
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


