Cough
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Pneumonia
Chronic Bronchitis
Asthma
Congestive Heart Failure
Malignancy
Less Common
Pulmonary Embolism
Pneumothorax
Mycobacterium Infection
Cystic Fibrosis
Sarcoidosis
Bronchiectasis
Smoking-Related Interstitial Lung Disease
Rare but Important
Usual Interstitial Pneumonia
Hypersensitivity Pneumonitis
Pneumoconioses
Langerhans Cell Histiocytosis
Goodpasture Syndrome
Bronchioloalveolar Cell Carcinoma
Constrictive Bronchiolitis
Pulmonary Alveolar Proteinosis
Foreign Body
Lipoid Pneumonia
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Over 1,000 conditions associated with cough
Review focuses on selected causes of cough identified on thoracic imaging
Chronic cough defined by duration ≥ 3 weeks
Commonly secondary to post-nasal drip, asthma, GERD, chronic bronchitis, bronchiectasis, ACE inhibitor medications, and extrinsic tracheal compression
Most are radiographically occult
Helpful Clues for Common Diagnoses
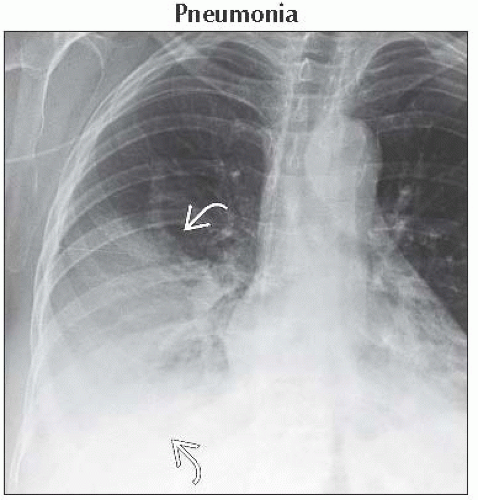
Pneumonia
Lobar or segmental lung consolidation
± pleural effusion
Chronic Bronchitis
± bronchial wall thickening &/or mucus plugging
Asthma
± hyperinflation
± bronchial wall thickening
Complications include pneumonia, pneumothorax, pneumomediastinum, or atelectasis
Congestive Heart Failure
Cardiomegaly and pleural effusions
Kerley B lines
Malignancy
Bronchogenic carcinoma
Spiculated lung nodule or mass
± lymphadenopathy
Lymphangitic carcinomatosis
Smooth or nodular thickening of interlobular septa
± pleural effusions and lymphadenopathy
Helpful Clues for Less Common Diagnoses
Pulmonary Embolism
CTA: Filling defect diagnostic
“Railroad track” or “doughnut” signs
Document signs of right heart strain
RV/LV chamber size >1, leftward bowing of interventricular septum, or reflux of contrast into IVC
Pneumothorax
Spontaneous
Young, tall, and thin male smokers
Also seen in emphysema, asthma, infection, lung fibrosis, or cystic lung disease
Traumatic or iatrogenic
Mycobacterium Infection
M. tuberculosis
Upper lobe cavitary nodule
Tree in bud opacities indicates endobronchial spread of disease
M. avium complex
Older women
Middle lobe or lingular bronchiectasis
Tree in bud opacities
Cystic Fibrosis
Hyperinflation with bronchiectasis
Early upper lobe involvement
Sarcoidosis
Paratracheal and symmetric hilar lymphadenopathy
± perilymphatic lung nodules (nodules along fissures, subpleural lung, and bronchovascular bundles)
Bronchiectasis
Smoking-Related Interstitial Lung Disease
Respiratory bronchiolitis associated interstitial lung disease
Symptomatic smoker
Upper lung predominant centrilobular nodules of ground-glass opacity
Desquamative interstitial pneumonia
Diffuse/patchy, lower lung predominant ground-glass opacity
± cystic spaces and centrilobular emphysema
Helpful Clues for Rare Diagnoses
Usual Interstitial Pneumonia
Basal and subpleural fibrosis with honeycombing
± mediastinal lymphadenopathy
Hypersensitivity Pneumonitis
Centrilobular nodules of ground-glass opacity
“Head-cheese” sign
Ground-glass opacity, air-trapping, and normal lung
Pneumoconioses
Asbestosis
Posterobasal and subpleural lung
Bilateral pleural plaques
Reticular and dot-like opacities early
Fibrosis and distortion late
Silicosis/Coal worker’s pneumoconiosis
Posterior and superior lung
Centrilobular and subpleural nodules
± calcified lymphadenopathy
Langerhans Cell Histiocytosis
Smokers, 20-40 years old
Centrilobular nodules and cavitary nodules
Spares costophrenic sulci
Round or bizarrely shaped cysts
± pneumothorax
Goodpasture Syndrome
Hemoptysis
Ground-glass opacity or consolidation
Bronchioloalveolar Cell Carcinoma
Chronic ground-glass opacity with “pseudocavitation”
Constrictive Bronchiolitis
Bronchiectasis, mosaic perfusion, and expiratory air-trapping
Causes include
Infection, toxic fume inhalation, collagen vascular diseases, and chronic lung transplant rejection
Pulmonary Alveolar Proteinosis
Chronic crazy-paving
Geographic ground-glass opacity with superimposed interlobular septal thickening
Foreign Body
History key to diagnosis
Lipoid Pneumonia
Aspiration of oils used for laxatives
Lower lobe consolidation or mass
Central low attenuation areas (-80 to -30 HU)
Image Gallery
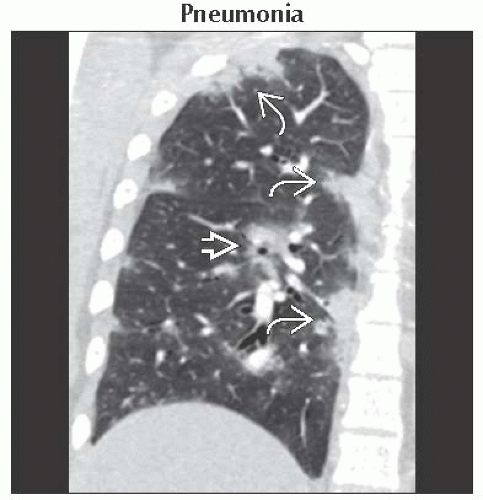 Coronal NECT shows peribronchial consolidation
 and peripheral subpleural consolidation and peripheral subpleural consolidation  reminiscent of organizing or eosinophilic pneumonia. This pattern is also described in H1N1 infection. reminiscent of organizing or eosinophilic pneumonia. This pattern is also described in H1N1 infection.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|