The association between coronary revascularization strategy (percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG]) and compliance with coronary artery disease (CAD) performance measures is not well studied. Our analysis studied patients enrolled in the Practice Innovation and Clinical Excellence registry, who underwent coronary revascularization using PCI or CABG in the 12 months before their most recent outpatient visit in 2011. We compared the attainment of CAD performance measures and statin use in eligible patients with PCI and CABG using hierarchical logistic regression models. Our study cohort consisted of 112,969 patients (80,753 with PCI and 32,216 with CABG). After adjustment for site and patient characteristics, performance measure compliance for tobacco use query (odds ratio [OR] 0.80; 95% confidence interval [CI] 0.76 to 0.86), antiplatelet therapy (OR 0.9; 95% CI 0.86 to 0.94) and angiotensin-converting enzyme inhibitor/angiotensin receptor blocker therapy (OR 0.89; 95% CI 0.84 to 0.94) was lower in CABG compared with patients with PCI. Patients who underwent recent CABG had higher rates of β-blocker (OR 1.25; 95% CI 1.16 to 1.33) and statin treatment (OR 1.37; 95% CI 1.31 to 1.43) compared with patients with PCI. Of the 79 practice sites, 15 (19%) had ≥75% of their patients with CAD (CABG or PCI) meeting 75% to 100% of all eligible CAD performance measures. In conclusion, gaps persist in compliance with specific CAD performance measures in patients with recent PCI or CABG, and 1 in 5 practices had ≥75% compliance of eligible CAD performance measures in the most of their patients.
Revascularization either using percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) represents an important event in patients with coronary artery disease (CAD). Both PCI and CABG and the subsequent outpatient care that ensues provide opportunity to improve control of cardiovascular risk factors in this secondary prevention known to have a high risk of recurrent cardiovascular events. The exact impact of mode of revascularization (percutaneous coronary revascularization [PCI] or CABG) on attainment of the American Heart Association/American College of Cardiology Foundation (AHA/ACCF) CAD performance measures is not well known. There are no studies directly comparing compliance with AHA/ACCF CAD performance measures in a national cohort of patients who have undergone recent PCI or CABG. A greater number of patients who underwent PCI compared with those who underwent CABG present with acute coronary syndrome. Additionally, the differences in practice patterns and the frequency of outpatient follow-up visits in the 2 groups could also lead to differences in compliance rates with specific CAD performance measures. We aimed to compare compliance with CAD performance measures in patients enrolled in the Practice Innovation and Clinical Excellence (PINNACLE) registry who underwent recent revascularization with either PCI or CABG. Statin use is currently not considered a performance measure for CAD; however, given the recent emphasis on the use of statin therapy as first-line treatment in patients with CAD, we also assessed whether the use of evidence-based statin therapy varies between these 2 groups.
Methods
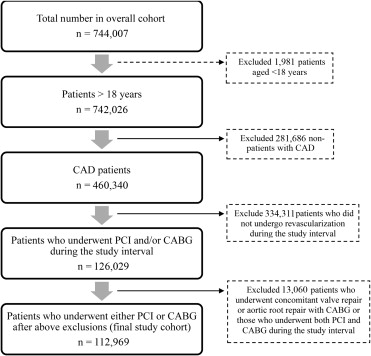
Among the National Cardiovascular Data Registry (NCDR), the PINNACLE program is the largest outpatient registry of cardiovascular disease patients. The PINNACLE registry represents the US first national prospective, outpatient registry for quality improvement in care and outcomes of cardiac patients. For the current analyses, we identified patients with CAD enrolled in the PINNACLE registry with clinic visits from January 1, 2011, to December 31, 2011. If a patient had multiple clinic visits during the study interval, the most recent clinic visit was used as the index visit. After identification of the index visit, we identified patients who had revascularization performed within the last 12 months from the index visit. Modes of revascularization included CABG or PCI (bare metal stent use, drug-eluting stent use, or nonstent PCI). Patients aged ≤18 years (n = 1,981) and patients who had both PCI and CABG performed during the study period (n = 13,060) were excluded from the analyses. The resulting cohort (n = 112,969) was then divided into those who underwent recent CABG (n = 32,216) or recent PCI (n = 80,753) ( Figure 1 ).
The outcome of interest for our study was the proportion of patients in the CABG or the PCI group meeting each of the CAD performance measures. We compared the following performance measures between the 2 groups in accordance with the 2005 AHA/ACCF performance measures in patients with CAD : (1) blood pressure control (percentage of patients with CAD who had a blood pressure of <140/90 mm Hg or who had a blood pressure of ≥140/90 mm Hg and were prescribed ≥2 antihypertensive medications during the most recent office visit), (2) lipid control (percentage of patients with CAD with low-density lipoprotein cholesterol [LDL-C] levels <100 mg/dl or who had an LDL-C result ≥100 mg/dl with a documented plan of care to achieve LDL-C <100 mg/dl, including, at a minimum, the prescription of a statin), (3) symptom and activity assessment (percentage of patients with CAD for whom there were documented results of an evaluation of the level of activity and an evaluation of presence or absence of angina symptoms/angina equivalents in the medical record), (4) tobacco use: screening and intervention (percentage of patients with CAD who were screened for tobacco use and received tobacco cessation counseling if identified as tobacco users), (5) antiplatelet therapy (percentage of patients with CAD who were prescribed aspirin or clopidogrel), (6) β-blocker therapy use (percentage of patients with CAD with previous myocardial infarction or a current or previous left ventricular ejection fraction (LVEF) ≤40%, who were prescribed β-blocker therapy), and (7) angiotensin-converting enzyme inhibitor (ACE-I)/angiotensin receptor blocker (ARB) use (percentage of patients with CAD with diabetes or a current or previous LVEF ≤40% who were prescribed ACE-I or ARB therapy). In addition, we also compared the proportion of PCI or CABG patients receiving statin therapy at the index visit.
Baseline demographic variables and co-morbidities were compared between the 2 groups (CABG vs PCI) using chi-square statistic for categorical variables and t test for continuous variables. These included gender, health insurance status (private [fee for service or health maintenance organization], public [Medicare, Medicaid, Veterans Affairs Administration], none), history of diabetes mellitus, hypertension, dyslipidemia, previous stroke or transient ischemic attack, peripheral artery disease (PAD), unstable angina, heart failure, body mass index, LVEF, history of myocardial infarction, history of tobacco use (never, current, quit in past 12 months, quit >12 months ago), total cholesterol levels, high-density lipoprotein cholesterol levels, LDL-C levels, and triglycerides.
We subsequently examined whether there were differences in compliance with eligible performance measures by mode of revascularization strategy (PCI or CABG) using hierarchical logistic regression models. These models included a random intercept for the office practice and a within-practice estimate of treatment effect to account for differences in volumes and enrollment duration among participating practices. To accomplish this, we first evaluated the proportion of eligible patients in the PCI or CABG groups meeting CAD performance measures. Subsequently, we adjusted for patient and clinical characteristics (in addition to practice effects) to examine the influence of patient factors on observed differences in performance. The following patient-level covariates were used in the adjusted analyses: age, gender, diabetes, dyslipidemia, hypertension, PAD, previous stroke, unstable angina, heart failure, history of myocardial infarction, tobacco use, LVEF, body mass index, atrial fibrillation, systolic blood pressure, diastolic blood pressure, heart rate, weight, cigarette use, and insurance status. Missing covariates were imputed using sequential regression imputation. Odds ratios and 95% confidence intervals are reported, and statistical significance was denoted by 2-sided p values <0.05.
Additionally, we evaluated the proportion of patients who underwent recent revascularization (either recent CABG or PCI) at each practice site meeting most (75% to 100%) of all eligible CAD performance measures in sites with >20 patients with recent PCI or CABG. Analyses were performed using SAS, version 9.3 for Windows x64 (SAS Institute, Inc., Cary, North Carolina) and R version 2.11.1.
Results
Our study population included 112,969 patients with CAD from the PINNACLE registry, of which 32,216 had undergone recent CABG and 80,573 had recent PCI. The 2 patient populations were significantly different from each other in terms of baseline characteristics ( Table 1 ). CABG patients were older, had a higher proportion of Caucasians and men, and had higher prevalence of diabetes, dyslipidemia, hypertension, current smoking, and LV systolic dysfunction (LVEF <40%) compared with patients with PCI. Patients in the PCI group had a higher prevalence of PAD and previous stroke or transient ischemic attack. Patients with recent CABG had lower levels of total cholesterol, LDL-C, and high-density lipoprotein cholesterol compared with the patients in the recent PCI group.
| Variable | Group | p-Value | |
|---|---|---|---|
| CABG [n = 32216] | PCI [n = 80753] | ||
| Age (years) mean ± standard deviation | 70.7 ± 11.4 | 64.4 ± 14.4 | < 0.001 |
| Men | 23441 (72.9%) | 44841 (55.6%) | < 0.001 |
| Caucasian ethnicity | 16887 (94.5%) | 31138 (86.9%) | < 0.001 |
| Insurance | < 0.001 | ||
| None | 1291 (4.4%) | 11591 (15.0%) | |
| Private | 15914 (54.8%) | 43854 (56.8%) | |
| Public | 11838 (40.8%) | 21758 (28.2%) | |
| Diabetes mellitus | 11764 (36.5%) | 22025 (27.3%) | < 0.001 |
| ∗ Dyslipidemia | 26919 (83.6%) | 56893 (70.5%) | < 0.001 |
| † Hypertension | 27798 (86.3%) | 65825 (81.5%) | < 0.001 |
| Peripheral artery disease | 20387 (63.3%) | 56627 (70.1%) | < 0.001 |
| Prior stroke/CVA | 11410 (35.4%) | 41666 (51.6%) | < 0.001 |
| Unstable angina pectoris | 988 (3.1%) | 2477 (3.1%) | 0.996 |
| Heart failure | 16919 (52.5%) | 52203 (64.6%) | < 0.001 |
| Prior myocardial infarction | 11260 (35.0%) | 28869 (35.7%) | 0.011 |
| Tobacco Use | < 0.001 | ||
| Never | 7341 (31.3%) | 18507 (25.7%) | |
| Current | 4400 (18.8%) | 10272 (14.3%) | |
| Quit within past 11 months | 1204 (5.1%) | 1725 (2.4%) | |
| Quit more than 11 months ago | 10494 (44.8%) | 41415 (57.6%) | |
| LVEF, mean ± standard deviation | 53.4 ± 13.7 | 55.9 ± 12.7 | < 0.001 |
| LVEF | < 0.001 | ||
| ≥50% | 2444 (57.9%) | 6457 (60.0%) | |
| 40-49% | 998 (23.7%) | 2962 (27.5%) | |
| 26-39% | 442 (10.5%) | 855 (7.9%) | |
| ≤25% | 335 (7.9%) | 493 (4.6%) | |
| Total cholesterol, mean ± standard deviation (mg/dL) | 154.7 ± 40.5 | 165.4 ± 42.5 | < 0.001 |
| High density lipoprotein, mean ± standard deviation (mg/dL) | 45.2 ± 14.5 | 49.0 ± 16.0 | < 0.001 |
| Low density lipoprotein cholesterol, mean ± standard deviation(mg/dL) | 84.6 ± 36.9 | 91.2 ± 38.6 | < 0.001 |
| Triglycerides, mean ± standard deviation (mg/dl) | 137.5 ± 105.2 | 137.7 ± 110.7 | 0.859 |
∗ Dyslipidemia defined as by the National Cholesterol Education Program criteria and includes documentation of the following: 1. Total cholesterol greater than 200 mg/dL (5.18 mmol/l); or 2. Low-density lipoprotein cholesterol (LDL-C) greater than or equal to 130 mg/dL (3.37 mmol/l); or 3. High-density lipoprotein (HDL-C) less than 40 mg/dL (1.04 mmol/l). For patients with known coronary artery disease, treatment is initiated if LDL-C is greater than 100 mg/dL (2.59 mmol/l), and this would qualify as hypercholesterolemia.
† Hypertension defined by any of the following: History of hypertension diagnosed and treated with medication, diet and/or exercise. 2. Prior documentation of blood pressure greater than 140 mm Hg systolic and/or 90 mm Hg diastolic for patients without diabetes or chronic kidney disease, or prior documentation of blood pressure greater than 130 mm Hg systolic and/or 80 mm Hg diastolic on at least two occasions for patients with diabetes or chronic kidney disease. 3. Currently on pharmacologic therapy for treatment of hypertension.
Table 2 describes the proportion of patients in each group meeting individual CAD performance measures and comparison between the 2 groups after adjusting for patient and site characteristics. Overall, compliance was highest for performance measure of blood pressure control in both groups (97.3% for CABG and 98.3% for patients with PCI), whereas it was lowest for lipid control (23.8% each for the CABG and the PCI groups) and symptoms/activity assessment (28.7% and 19.9% for the CABG and the PCI groups, respectively). After adjusting for site and patient characteristics ( Table 2 ), patients with recent CABG were less likely to meet the performance measures for tobacco use query (odds ratio [OR] 0.80, 95% confidence interval [CI] 0.76 to 0.86), antiplatelet therapy (OR 0.90, 95% CI 0.86 to 0.94), and ACE-I/ARB therapy (OR 0.89, 95% CI 0.84 to 0.94) compared with patients with PCI. CABG patients were more likely to meet the performance measure for β-blocker therapy (OR 1.25, 95% CI 1.16 to 1.33) and to be on statin therapy (OR 1.37, 95% CI 1.31 to 1.43) compared with patients with PCI. Compliance with CAD performance measures of blood pressure control, lipid control, symptom and activity assessment, and smoking cessation intervention were not significantly different between the 2 groups after adjustment. We also performed exploratory analyses comparing compliance with CAD performance measures among patients who had both PCI and CABG during the study interval with patients who underwent either CABG or PCI. Compliance with CAD performance measures was either greater (for some measures) or similar in patients who underwent both PCI and CABG compared with those who had revascularization either through PCI or CABG ( Supplementary Figure 1 ).



