11 Coronary Artery Disease
Ischemia, Infarction, and Complications
Wall Motion Abnormalities and Their Relation to Blood Flow
Although echocardiographic estimates using wall motion correlate well with autopsy estimates of infarction,1,2 in general, echocardiography tends to overestimate the amount of ischemic/infarcting muscle.3 Pathologic:echocardiographic correlations
Echocardiography for Wall Assessment in Acute Myocardial Infarction
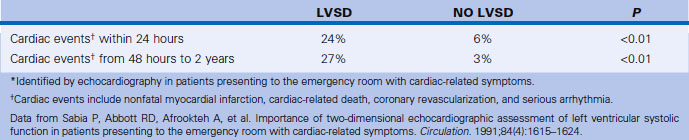
In terms of 1-year mortality, a WMS <2 has high predictive value for a good prognosis and low complication rate. A WMS >7 on admission predicts Killip Class 3 or 4 with a sensitivity of 88%, specificity of 57%, positive predictive value of 35%, and negative predictive value of 95%, and may, therefore, be helpful in identifying early low-risk patients.4 The degree of systolic function of the nonischemic/infarcting myocardial segments is largely a function of the adequacy of perfusion to these other territories. The normal response of noninfarcting myocardium is hyperkinesia. The absence of hyperkinesia correlates with more extensive CAD (e.g., prior infarction, acute ischemia, stunning, or hibernation), and high risk for early mortality.4,5 Echocardiography is superior to electrocardiography in determining infarct extension.6 Echocardiographic assessment of left ventricular systolic function (presence/absence of WMAs) in patients presenting to the emergency department with cardiac-related symptoms is able to stratify patients (Table 11-1).
Echocardiographic Views to Assess Left Ventricular Wall Motion and its Relation to Coronary Arteries
Apical 5-Chamber View
 The A5CV images through the anterior septum; therefore, this is predominantly LAD territory.
The A5CV images through the anterior septum; therefore, this is predominantly LAD territory.
 The apex is usually LAD territory.
The apex is usually LAD territory.
 The lateral wall perfusion may reflect any combination of LAD–diagonal branches, left circumflex–obtuse marginal branches, and right coronary distal posterolateral branches.
The lateral wall perfusion may reflect any combination of LAD–diagonal branches, left circumflex–obtuse marginal branches, and right coronary distal posterolateral branches.
 A5CV sampling, as with all “apical” views, is prone to foreshortening.
A5CV sampling, as with all “apical” views, is prone to foreshortening.
 The A4CV images through the inferior interventricular septum.
The A4CV images through the inferior interventricular septum.
 The basal portion is typically perfused by septal branches of the posterior descending artery.
The basal portion is typically perfused by septal branches of the posterior descending artery.
 The lateral wall perfusion may reflect any combination of LAD–diagonal branches, left circumflex–obtuse marginal branches, and right coronary distal posterolateral branches.
The lateral wall perfusion may reflect any combination of LAD–diagonal branches, left circumflex–obtuse marginal branches, and right coronary distal posterolateral branches.
Coronary Care Unit Echocardiographic Studies
Scanning Issues/Required Parameters to Obtain from Scanning
 LV quantification (Simpson’s for ejection fraction, end-systolic volume)
LV quantification (Simpson’s for ejection fraction, end-systolic volume)
 Stroke volume, cardiac insufficiency, right ventricular systolic pressure
Stroke volume, cardiac insufficiency, right ventricular systolic pressure
 Weight and height for body surface area
Weight and height for body surface area
 Note on the worksheet if the patient was on inotropes (e.g., dobutamine, milrinone) or an intra-aortic balloon pump.
Note on the worksheet if the patient was on inotropes (e.g., dobutamine, milrinone) or an intra-aortic balloon pump.
 If a cardiogenic shock case, have the echocardiography attending review the case before disconnecting.
If a cardiogenic shock case, have the echocardiography attending review the case before disconnecting.
 If on an intra-aortic balloon pump, partial rolling of the patient may be acceptable in some cases, at the discretion of the attending in the cardiac care unit.
If on an intra-aortic balloon pump, partial rolling of the patient may be acceptable in some cases, at the discretion of the attending in the cardiac care unit.
Echocardiography for the Assessment of Complications of Acute Myocardial Infarction
Pump Failure
Left Ventricular Systolic Dysfunction and Failure
LV pump failure is the dominant cause (>65%) of in-hospital mortality from acute MI. It may occur with a first, and massive, infarction, or with a second or third infarction. Severe WMAs in extensive territories are expected in cardiogenic shock due to pump failure. The LV may or may not be dilated. Massive acute first MI is unlikely to have prominent dilation. It is the combination of abrupt fall in ejection fraction and lack of dilation that is responsible for the low stroke volume, and resultant low output, despite tachycardia.
Mechanical Complications of Infarction
Free Wall Rupture
Free wall rupture accounts for approximately 10% of postinfarction sudden deaths. Rupture typically occurs through the lateral (but it may be through any) wall of the left ventricle. The right ventricle is one-seventh as likely to rupture as the LV. Rupture occurs only following a transmural infarction. The time is typically 3 to 5 days following MI, but may be earlier, especially if the patient received fibrinolytics. A subset of patients with free wall rupture will not experience immediate sudden death: this group is said to have “subacute rupture”7 with echocardiographic signs of tamponade, pericardial effusion >5 mm, and echodensities in the pericardial space that represent coagulated blood. Suspected clot in the pericardial space, which appears as an echo-dense mass in the pericardial space, may be a sign of free wall rupture8 and renders the likelihood of evacuation through a pericardiocentesis needle unlikely. Urgent surgical repair will salvage some cases. Bedside echocardiography is the most suitable test to identify free wall rupture. Ultimately, there is no perfect echocardiographic sign to distinguish severe early postinfarction tamponade from rupture. Identification of clot in the pericardial space is useful, however.
Left Ventricular (or Other) False Aneurysm
Ventricular false or “pseudo” aneurysms contain no myocardial layer; a free wall rupture is contained by adherence of overlying pericardium or by a thin layer of epicardium beneath pericardium. A false aneurysm develops because a tear into a portion of recently transmurally infarcted myocardium extended up to the epicardium or even through it, and complete rupture of the LV into the pericardial cavity was avoided because pericardial adhesions (the result of prior pericarditis) contained the rupture. Thus, a false aneurysm is to be considered an intermediate form of rupture, and reparative surgery is urgently indicated. The contained rupture typically extends away from the neck to appear as an echo-free space with the shape of a mushroom cap. The neck usually is less than half the width of the body of the false aneurysm. This is in contradistinction to the wide neck of a (true) aneurysm, which usually is as wide as the body of the aneurysm itself (the dimension of the neck/the dimension of the body is 0.9 to 1.0).9 It is the width of the neck, more than any other detail, that renders the outpouching of the LV a false aneurysm rather than a true aneurysm. In systole, the false aneurysm typically bulges out as it receives part of the LV stroke volume. The flow in and out (or “to-and-fro”) is evident by color and spectral Doppler.10 Two-dimensional echocardiography is the procedure of choice to establish the presence of a pseudoaneurysm. Cineangiography and MRI also are excellent means to image false aneurysms. Confusion occurs about aneurysms of the base of the LV between the body of the posteromedial papillary muscle and the mitral annulus. Often the traction of the papillary muscle keeps the neck narrow, replicating the sign of a false aneurysm. Thus the “neck” sign is best applied away from the trouble spot on the posterolateral wall, where both aneurysms and false aneurysms occur, but where they cannot be easily distinguished by neck morphology alone.