Coronary Artery Disease
Baris Gencer • Debabrata Mukherjee • Marco Roffi
QUESTIONS
1.A 67-year-old man presents to the emergency room with increasing frequency of chest pain on exertion and one episode of rest pain lasting 15 minutes the day of admission. Other than for hypertension and hyperlipidemia his medical history is unremarkable. He quit smoking (1 pack a year for 20 years) 11 years ago. On physical examination he is afebrile, his pulse is 78 bpm, and his blood pressure is 138/76 mmHg. Cardiac and pulmonary auscultations are unremarkable. His current medications include aspirin, metoprolol, ramipril, and atorvastatin. The electrocardiogram (ECG) at admission reveals deep T-wave inversion in the precordial leads and no pathologic Q waves. You admit the patient to the hospital and start intravenous (IV) unfractionated heparin (UFH) and nitroglycerine. The first available serum troponin I level is 1.4 μg/L (upper limit of normal, 0.09 μg/L). Cardiac echocardiography shows an anterior and apical hypokinesia with mildly depressed left ventricular function. The next step in his management would be
a.low-level exercise stress ECG next morning.
b.to continue IV heparin and nitroglycerin, increase β-blocker, and add a calcium antagonist until completely free of chest pain for 24 hours, then discharge home.
c.coronary angiography within 48 hours followed by percutaneous intervention/surgical revascularization if indicated.
d.dobutamine echocardiogram or myocardial perfusion scan within 48 hours.
e.continue IV heparin and nitroglycerin, increase β-blocker, and add a calcium antagonist until completely free of chest pain for 24 hours, then transfer to a cardiac rehabilitation program.
2.A 57-year-old man presenting with unstable angina (UA) was successfully treated with percutaneous coronary intervention (PCI) of a significant lesion of the right coronary artery (RCA) in the presence of a normal left ventricular ejection fraction (LVEF). He is referred for cardiac rehabilitation program. What is the expected benefit?
a.Reduced risk of stent restenosis
b.Lower rate of hospital readmission
c.Reduction in maximal V˙O2
d.Higher event rate related to exercise
e.Reduced risk of stent thrombosis
3.A 66-year-old man with stable angina at low exertion level was investigated with coronary angiography that showed an isolated significant lesion (70%) of the ostium and mid-portion of the left main coronary artery in the presence of a normal left ventricular function. What is the correct statement regarding the recommended approach?
a.Heart team discussion between the interventional cardiologist and the cardiac surgeon to select the best treatment option is the recommended approach.
b.Coronary artery bypass grafting (CABG) is the recommended approach for all patients with left main disease.
c.PCI is the recommended approach for all patients with left main disease.
d.A calculation of the Society of Thoracic Surgeons (STS) and SYNTAX (Synergy between PCI with TAXUS and Cardiac Surgery) scores is not recommended at this stage.
e.The choice of treatment is independent of the clinical presentations (stable angina or acute coronary syndromes [ACSs]).
4.A 58-year-old man with coronary artery disease (CAD) and severe chronic obstructive pulmonary disease (COPD) with forced expiratory volume in the first second of expiration (FEV1)/forced vital capacity <0.74 with FEV1 <40% predicted had stenting of the mid-left anterior descending artery (LAD) 10 months prior to admission with a 3.0 mm × 24 mm bare metal stent (BMS). He presents now with recurrent angina despite intensified medical treatment, and coronary angiography reveals a severe and diffuse in-stent restenosis (ISR). A reasonable next therapeutic option would be
a.plain balloon angioplasty.
b.coronary artery bypass surgery.
c.drug-eluting stent (DES) implantation (stent-in-stent).
d.medical therapy.
e.brachytherapy.
5.A 66-year-old man had in the last few months sporadic episodes of chest pain on exertion. His cardiovascular (CV) risk factors included diabetes, hypertension, and hypercholesterolemia. He had no other comorbidity. Coronary angiography revealed a lesion of 60% of the RCA in addition to multiple nonsignificant plaques affecting the three coronary arteries. The fractional flow reserve (FFR) of the RCA (0.0.85) and LVEF were normal. What is the recommended treatment for this patient?
a.CABG is the first recommended approach as the risk of surgical procedure is low.
b.PCI is the first recommended approach as the SYNTAX score is low.
c.Perform an additional imaging (myocardial perfusion scan or magnetic resonance [MR] perfusion scan) in addition to optimal medical management.
d.Guideline-directed medical therapy is the first recommended approach.
e.Repeat coronary angiography after 6 months to exclude disease progression in addition to optimal medical management.
6.A 58-year-old male smoker treated for hypertension complained about chest pain on exertion in the preceding 4 weeks. To investigate the clinical symptoms, you performed a stress perfusion cardiac magnetic resonance showing hypoperfusion during IV administration of adenosine. Which area of the myocardium is more vulnerable to hypoperfusion?
a.Subepicardium
b.Mid-myocardium
c.Subendocardium
d.Pericardium
e.All of the above
7.A 73-year-old man presents to the emergency room with severe mid-sternal chest discomfort. He appears anxious and in distress. His heart rate is 66 bpm, blood pressure is 92/68 mmHg, and respiratory rate is 14. There is marked jugular venous distention. Cardiac auscultation is unremarkable and the lungs are clear. ECG reveals 2-mm ST-segment elevation in leads II, III, and aVF. The most likely diagnosis is
a.acute pericarditis.
b.acute aortic dissection.
c.pneumothorax.
d.inferior wall myocardial infarction (MI) with right ventricular infarction.
e.pneumonia.
8.A 65-year-old hypertensive man was hospitalized for non-ST-segment-elevation myocardial infarction (NSTEMI). The clinical examination shows a fourth heart sound (S4). What is expected to be found at the echocardiography?
a.Reduction in left ventricular compliance
b.Rapid deceleration of transmitral flow during protodiastolic filling of the left ventricle
c.Increased inflow into the left ventricle
d.Reduced left ventricular systolic function
e.Aortic sclerosis
9.A 66-year-old man known for diabetes mellitus treated with oral glucose lowering medications presents with UA. Coronary angiography reveals a three-vessel disease: 70% mid-LAD lesion, complex, long, and calcified; 70% focal proximal left circumflex artery (LCX) stenosis; and 70% focal mid-RCA lesion. A hybrid coronary revascularization was proposed. All the following statements are correct regarding hybrid coronary revascularization, with the exception of one.
a.Hybrid revascularization is defined as the planned combination of surgical and percutaneous revascularization (typically left internal mammary artery [LIMA]-to-LAD and PCI of ≥1 additional vessel).
b.Hybrid revascularization is reasonable in patients with limitations to traditional CABG, such as heavily calcified proximal aorta.
c.Hybrid revascularization is reasonable in patients with lack of suitable graft conduit.
d.Hybrid revascularization is reasonable in patients with unfavorable LAD artery for PCI.
e.Hybrid revascularization mandates surgical and percutaneous revascularization during the same procedure.
10.A 57-year-old female smoker presents to the emergency department for an ongoing new typical chest pain lasting 30 minutes. The physical examination is unremarkable and she is hemodynamically stable. The ECG reveals T inversion in II, III, and aVF leads. Which of the following biomarker elevation has been associated with an improved benefit of ticagrelor therapy over clopidogrel in patients hospitalized with ACS?
a.Ultrasensible C-reactive protein
b.Interleukin-6
c.High-sensitive troponin T (Hs-TnT)
d.D-dimers
e.Lactate dehydrogenase
11.A 58-year-old man known for a metabolic syndrome shows increasing frequency of chest pain on exertion in the preceding 2 weeks. Resting ECG did not show significant abnormalities. Which of the exercise parameters are associated with adverse prognosis?
a.Duration of symptom-limiting exercise <5 METs (metabolic equivalents)
b.Failure to increase systolic blood pressure ≥120 mmHg, or a sustained decrease ≥10 mmHg, or below rest levels, during progressive exercise
c.ST-segment depressions ≥2 mm
d.Angina pectoris at low exercise workloads
e.All of the above
12.A 58-year-old man presented stable chest pain on moderate effort exertion in the preceding 12 months. The medical history is relevant for hypertension and hyperlipidemia. His current treatment includes lisinopril, atorvastatin, metoprolol, and aspirin. He is addressed for coronary angiography that showed a 70% to 90% lesion of the LCX successfully treated with PCI with a placement of a DES. The LVEF was normal. What was the expected benefit of a PCI over a medical therapy?
a.Decrease of total mortality
b.Decrease of CV mortality
c.Decrease of MI
d.Decrease of heart failure events
e.No improvement of any of the mentioned endpoints
13.The same patient was investigated with stress imaging before and after PCI to assess the extension of myocardial ischemia. Which of the following statements is correct regarding the benefit of PCI over medical therapy in this setting?
a.A greater reduction in the extension of residual myocardial ischemia
b.A greater resolution of angina episodes
c.An increased benefit of ischemia reduction in patients with extensive ischemic areas at baseline
d.A greater improvement in symptoms
e.All of the above
14.A 63-year-old man has been successfully treated with percutaneous coronary revascularization for a stable angina pectoris. His low-density lipoprotein cholesterol (LDL-C) value was 143 mg/dL. Which of the following statement is incorrect regarding the impact of prescribing intensive lipid-lowering therapy (e.g., 80 mg atorvastatin daily) compared with less intensive therapy (e.g., 10 mg atorvastatin daily)?
a.Higher LDL-C level reduction
b.Significant absolute risk reduction of major adverse cardiovascular events (MACE) of ~2% over 5 years
c.Significant relative risk reduction of MACE of ~20% over 5 years
d.Increased incidence of persistent liver aminotransferase levels of 1%
e.Significant reduction of overall mortality
15.A 67-year-old man is treated with PCI. Which of the following statement is not correct regarding periprocedural anticoagulation?
a.An anticoagulant should be administered to all patients undergoing PCI.
b.Administration of IV UFH is useful in patients undergoing PCI.
c.An additional dosage of IV enoxaparin should be administered at the time of PCI to patients who received the last subcutaneous dose of enoxaparin 12 hours or more prior to PCI.
d.The appropriate diagnostic test to check for the level of anticoagulation with UFH during PCI is the activated clotting time.
e.Fondaparinux might be used as the sole anticoagulant to support PCI.
16.A 65-year-old male hypertensive smoker benefited from primary PCI of the RCA for inferior STEMI. Which of the following statements is not correct regarding secondary prevention in this patient?
a.Medically supervised cardiac rehabilitation programs are recommended.
b.Blood pressure should be controlled with a goal of <140/90 mmHg.
c.Statin therapy should be uptitrated to achieve an LDL-C <70 mg/dL
d.Smoking cessation program should be proposed.
e.Even in the absence of symptoms, routine periodic stress testing is indicated.
17.A 60-year-old male patient was treated 2 years earlier with PCI and the implantation of BMS in the LAD for NSTEMI. He complains about recurrent worsening exertional chest pain in the last week. Coronary angiography reveals ISR. What are the predisposing factors for BMS restenosis?
a.Diabetes
b.Increasing stent length
c.Increasing stent number
d.Decreasing stent diameter
e.All of the above
18.A 60-year-old healthy colleague on no medication with an LDL-C level of 123 mg/dL and High-sensitivity C-reactive protein (hs-CRP) level >2.0 mg/L asked to you whether he should take rosuvastatin 20 mg a day. Which of the following statements is incorrect regarding JUPITER trial?
a.Rosuvastatin 20 mg/day reduced LDL-C levels by 50%.
b.Rosuvastatin 20 mg/day significantly decreased the incidence of MI.
c.Rosuvastatin 20 mg/day reduced hs-CRP by 37%.
d.Rosuvastatin 20 mg/day did not significantly decrease the incidence of stroke.
e.Rosuvastatin 20 mg/day significantly increased the incidence of physician-reported diabetes.
19.A 65-year-old man with diabetes presented typical chest pain on exertion in the previous 2 months. Coronary angiography revealed significant complex multivessel coronary disease (SYNTAX score, 34). What is the expected benefit of a revascularization with CABG versus PCI?
a.CABG is associated with a reduction of death only.
b.CABG is associated with a reduction of stroke only.
c.CABG is associated with a reduction of death and of MI, but not of stroke.
d.CABG is associated with a reduction of all following individual endpoints: stroke, myocardial infraction, and death.
e.CABG is associated with a reduction of MI only.
20.A 41-year-old male smoker was admitted for STEMI and quitted smoking after hospitalization. Which of the following statements is incorrect regarding smoking cessation?
a.Smoking cessation reduces the relative risk of total mortality by >30% over a mean follow-up of 5 years.
b.Smoking cessation reduces the relative risk of nonfatal MI by >30% over a mean follow-up of 5 years.
c.More than 70% of patients quit smoking after ACS.
d.Smoking cessation counseling program is effective to help smokers to quit smoking.
e.Smoking cessation counseling program should be proposed during hospital stay and continued after discharge.
21.Six hours after the start of chest pain, a 55-year-old diabetic man was admitted to the emergency department for anterior STEMI with hemodynamic instability (cold extremities, heart rate of 110 bpm and blood pressure of 85/50 mmHg) and severe reduced LVEF (25% to 30%) estimated by echocardiography. What is the correct statement regarding the decision to perform an emergent revascularization versus an initial medical stabilization according to the SHOCK trial?
a.Significant reduction of mortality with early revascularization compared with intensive medical therapy at 30 days
b.No significant difference of mortality with early revascularization compared with intensive medical therapy at 30 days
c.Significant reduction with intensive medical therapy compared with early revascularization at 30 days
d.Significant reduction of mortality with early revascularization compared with intensive medical therapy at 6 months
e.Answers b and d are correct
22.A 63-year-old man known for chronic kidney disease (CKD) due to long-term uncontrolled hypertension is hospitalized for elective coronary angiography. Which of the following statements is not correct?
a.Patients with CKD undergoing cardiac catheterization should receive adequate preparatory hydration.
b.In patients with CKD, the volume of contrast should be minimized.
c.Administration of N-acetyl-cysteine is useful for the prevention of contrast-induced acute kidney injury (AKI).
d.Contrast-induced AKI is one of the leading causes of hospital-acquired AKI.
e.In elective cases, patients should be assessed for risk of contrast-induced AKI before coronary angiography.
23.A 45-year-old man benefited from primary PCI for STEMI. The adjunctive antithrombotic therapy consisted of aspirin, heparin, and abciximab. The addition of abciximab is associated with
a.no significant difference in the risk of stroke.
b.a significant increase in the risk of stroke.
c.a significant decrease in the risk of stroke.
d.a significant decrease of nonhemorrhagic stroke only.
e.a significant increase of hemorrhagic stroke only.
24.A 65-year-old diabetic man known for a multivessel coronary disease underwent revascularization with CABG. What is the target LDL-C that should be aimed?
a.160 mg/dL
b.130 mg/dL
c.100 mg/dL
d.70 mg/dL
e.50 mg/dL
25.A 62-year-old man was hospitalized for an NSTEMI and underwent invasive strategy with DES-based PCI. Which of the following statements about antiplatelet therapy is wrong?
a.Patients not on aspirin should be given nonenteric aspirin 325 mg before PCI.
b.After PCI, use of aspirin should be continued indefinitely.
c.Additional aspirin (81 to 325 mg) is recommended in all patients on chronic aspirin therapy before PCI.
d.A loading dose of a P2Y12 receptor inhibitor should be given to patients undergoing PCI with stenting at the latest after completion of PCI (e.g., clopidogrel 600 mg, prasugrel 60 mg, and ticagrelor 180 mg).
e.In patients receiving a stent (BMS or DES) during PCI for ACS, P2Y12 receptor inhibitor should be given for 12 months.
26.A 50-year-old white female nonsmoker without history of cardiovascular disease (CVD) and treated only with ramipril for hypertension was hospitalized for UA. The ECG revealed T inversion in the lateral leads. The medical student who admitted the patient asks you what is the proportion of patients that undergo coronary angiography for ACS who have nonsignificant CAD.
a.<5%
b.10% to 15%
c.20% to 30%
d.25% to 35%
e.30% to 40%
27.A 59-year-old man was successfully treated with PCI for NSTEMI. During the procedure, the patient received bivalirudin. Due to closure device failure, the patient suffered a major bleeding at the access site difficult to control with manual compression and you are in need of reversing the anticoagulation. Your treatment of choice is
a.fresh frozen plasma.
b.prothrombin complex.
c.epsilon aminocaproic acid.
d.protamine.
e.vitamin K.
28.A 63-year-old man presents typical chest pain at moderate exertion in the preceding month and he is admitted to the hospital for coronary angiography. While considering the best access for the procedure, which of the following statements is not correct regarding a radial vascular access?
a.The radial vascular access may be useful to decrease access site complications.
b.The radial vascular access is preferred in patients with coagulopathy.
c.The radial vascular access is preferred in patients with morbid obesity.
d.The radial vascular access is preferred in patients with an elevated INR.
e.The radial vascular access is more frequently performed in the United States than in Europe.
29.Which of the following conditions does not justify immediate coronary angiography and, if needed, revascularization?
a.A 57-year-old man presenting with typical chest pain lasting 60 minutes up to emergency department arrival. As cardiologist on call you are called in immediately and when you see the patient, his pain has virtually disappeared while ECG shows 2-mm ST-segment elevation in the inferior leads.
b.A 60-year-old diabetic man known for previous coronary disease presenting with not better defined chest discomfort lasting for 10 hours and currently decreasing in intensity, pulmonary edema, and 3-mm ST-segment elevation in the anterior leads on ECG in the absence of Q waves.
c.A 65-year-old man known for CAD complaining of progressive shortness of breath since 1 week. At admission, no ongoing chest pain with stable hemodynamic status but bibasilar rales at lung auscultation. The ECG revealed ST-segment elevation as well as Q waves in the anterior leads.
d.A 70-year-old man presenting to the emerging department with on–off chest pain in the preceding 20 hours. Upon your arrival he has mild chest pain and on ECG 2-mm ST elevation in the lateral leads in the absence of Q waves.
e.A 68-year-old diabetic man presenting to the emerging department with chest pain lasting 4 hours, hypotension, and tachycardia and on ECG 3-mm ST-segment elevation in the anterior and lateral leads.
30.A 76-year-old man with no prior cardiac history presents to the emergency department with acute retrosternal chest pain. He had a single episode of chest pain lasting 4 hours 5 days ago. At that time he did not seek medical attention. Physical examination reveals a slightly confused diaphoretic patient, with heart rate of 95 bpm, blood pressure of 76/42 mmHg, and cold extremities. He is able to lie flat, the lungs are clear, and the jugular veins are distended even if the upper part of the body is raised at 45°. On cardiac auscultation a loud systolic murmur is audible, while on ECG Q waves associated with ST-segment elevation are detected in the inferior leads. The most likely diagnosis is
a.severe left ventricular failure.
b.ventricular septal defect.
c.acute mitral regurgitation.
d.right ventricular infarction.
e.cardiac rupture.
31.Considering the suspected diagnosis for the patient described in the previous question, what is the next diagnostic step?
a.Cardiac enzymes
b.Chest X-ray
c.Transesophageal echocardiography
d.Immediate coronary angiography
e.Transthoracic echocardiography
32.While considering surgery for the patient described in the previous two questions, the most effective cardiac unloading treatment for him is
a.fluid resuscitation.
b.β-blockers.
c.mechanical ventilation with positive end-expiratory pressure.
d.vasopressors.
e.intra-aortic balloon pump.
33.A 66-year-old man with a history of diabetes was referred for coronary angiography. The procedure showed complex multivessel disease. Which of the following statements justify the use of DES over BMS?
a.Patient with diabetes mellitus
b.Long coronary lesions
c.Multifocal coronary lesions
d.Small vessel disease
e.All of the above
34.A 63-year-old male smoker with no history of CVD and a treatment for hypertension complains of typical chest pain on exertion the preceding 2 months without any aggravation. He is scheduled for coronary angiography in 7 days. In the meantime, you should start the following antiplatelet treatment(s):
a.Low-dose aspirin daily
b.Clopidogrel 75 mg daily without loading dose
c.A loading dose of clopidogrel 300 mg followed by 75 mg daily should be given
d.A loading dose of ticagrelor 180 mg followed by 2 × 90 mg/day should be given
e.No antiplatelet therapy needed prior to coronary angiography
35.A 66-year-old man with intermediate probability of ischemic heart disease is scheduled for stress testing. Which of the following strategies is not recommended?
a.Exercise ECG if able to exercise and ECG interpretable
b.Exercise echocardiography if able to exercise but uninterpretable ECG
c.Pharmacologic stress with nuclear myocardial perfusion imaging if able to exercise and ECG interpretable
d.Exercise stress with nuclear myocardial perfusion imaging if able to exercise but uninterpretable ECG
e.Pharmacologic stress with cardiac MR imaging if unable to exercise and interpretable ECG
36.A 65-year-old man with hypercholesterolemia, diabetes, and hypertension presents new, worsening, typical angina symptoms. The angiogram (Fig. 4.1) shows
a.occluded LAD.
b.occluded left circumflex coronary artery.
c.severe ostial and moderate distal left main trunk stenosis.
d.normal coronary arteries.
e.normal RCA.
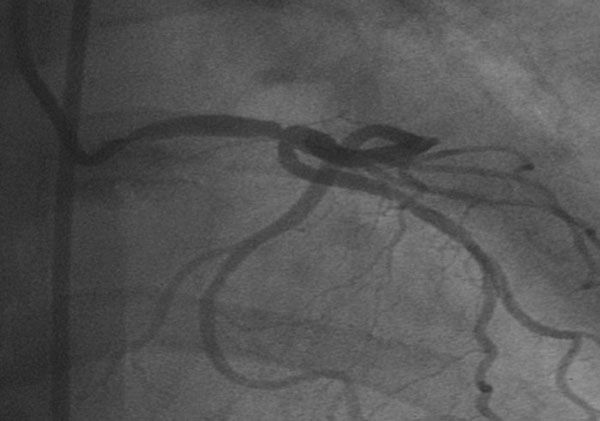
Figure 4.1
37.A 64-year-old man with stable ischemic heart disease (SIHD) wants to know whether he is at high risk for mortality. Which of the following clinical and exercise testing data are useful to predict the risk?
a.Typical angina symptoms
b.Diabetes
c.ST-segment depression during exercise
d.Proportion of predicted METs achieved
e.All of the above
38.A 48-year-old woman presents with congestive heart failure. The etiology of her heart failure based on the coronary angiogram (Fig. 4.2) is
a.severe CAD.
b.arteriovenous fistula.
c.aortic regurgitation.
d.absent RCA.
e.coronary perforation.
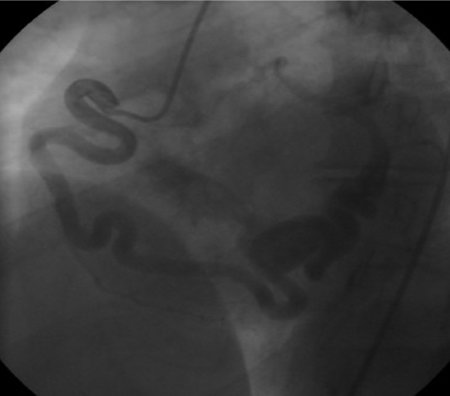
Figure 4.2
39.A 72-year-old man known with a history of coronary heart disease presents typical chest pain. During the transport to the PCI center, the patient had two episodes of ventricular fibrillation requiring electrical reanimation. ECG shows inferolateral ST depression. What does the angiography show (Fig. 4.3)?
a.Lesions at bifurcation
b.Stenosis of the ostium of the LCX
c.Stenosis of the ostium of the LAD
d.Stenosis of the distal left main trunk
e.All of the above

Figure 4.3
40.During coronary angioplasty of the RCA, this 72-year-old patient developed sharp chest pain with rapid development of hypotension and tachycardia. The etiology based on Figure 4.4 is
a.abrupt closure of the RCA.
b.dissection of the RCA.
c.perforation of the RCA.
d.allergic reaction.
e.distal embolization of an atherosclerotic plaque.

Figure 4.4
41.For which clinical situation is coronary angiography not recommended in patients with SIHD?
a.Risk assessment in patients with SIHD not candidates for revascularization because of comorbidities
b.Risk assessment in patients with SIHD who have preserved LV function and low-risk criteria on noninvasive testing
c.Risk assessment in patients who are at low risk according to clinical criteria and have not undergone noninvasive risk testing
d.Risk assessment in asymptomatic patients with no evidence of ischemia on noninvasive testing
e.All the mentioned clinical situations do not justify coronary angiography in the initial phase of patient management
42.A 66-year-old man with diabetes with no hypertension but end-stage renal failure treated with hemodialysis in the last 15 years presents with worsening dyspnea and suspicion of ischemia at the stress imaging. What are the most characteristic findings relating to the coronary arteries to be found at angiography?
a.Tortuous coronary vessels
b.Calcified coronary arteries
d.Coronary arteries with anomalous origins
e.Normal coronary arteries (symptoms caused by small vessel disease)
43.A 65-year-old man with SIHD wants to optimize secondary prevention. Which of the following statements does not apply?
a.Smoking cessation and avoidance of exposure to environmental tobacco smoke at work and home should be encouraged.
b.Patients should be screened for depression and treated when indicated.
c.Treatment with clopidogrel is reasonable when aspirin is contraindicated.
d.Dipyridamole is not recommended as antiplatelet therapy for patients with SIHD.
e.Acupuncture might be used for the purpose of improving symptoms of patients with SIHD.
44.A 74-year-old man was hospitalized for a subacute MI. He presented 1 week prior to admission one episode of chest pain lasting 3 hours but he did not seek medical attention. The ECG at admission revealed deep Q waves and persisting ST-segment elevation in the anterior leads. The angiography showed a total occlusion of the proximal left anterior ascending coronary artery. Which statement about the benefit of revascularization in this particular patient does apply?
a.PCI reduces the occurrence of death.
b.PCI reduces the occurrence of reinfarction.
c.PCI reduces the occurrence of heart failure.
d.CABG should be preferred to PCI.
e.PCI does not reduce the occurrence of death, reinfarction, or heart failure.
45.A 60-year-old man with a history of PCI 3 years previously asks for your advice with respect to his pharmacologic treatment. He is asymptomatic and his CV risk factors include smoking, hypertension, hypercholesterolemia, and impaired glucose tolerance. His medications include aspirin, atorvastatin, metoprolol, metformin, and lisinopril. His friend told him that clopidogrel should be added to his regimen. What is the correct statement about that suggestion in this particular patient?
a.There is no significant benefit associated with clopidogrel plus aspirin as compared with placebo plus aspirin in reducing the incidence of the primary endpoint of MI, stroke, or death from CV causes.
b.There is a significant benefit associated with clopidogrel plus aspirin as compared with placebo plus aspirin in reducing the incidence of the primary endpoint of MI, stroke, or death from CV causes.
c.The rate of severe or moderate bleeding is not significantly greater with clopidogrel and aspirin compared with aspirin alone.
d.The rate of severe or moderate bleeding is significantly greater with clopidogrel and aspirin compared with aspirin alone.
e.Answers a and d are correct.
46.A 60-year-old woman was discharged after an MI. Pharmacologic secondary prevention with antiplatelet agents, statins, β-blockers, and angiotensin-converting enzyme inhibitors is associated with
a.significant reduction in recurrent angina but no mortality benefit.
b.significant survival advantage.
c.no significant clinical benefit.
d.significant reduction in recurrent hospitalization but no mortality benefit.
e.significant survival advantage only in patients treated with PCI.
47.A 55-year-old man presents since 3 months typical chest pain at moderate exertion. The angiography revealed single-vessel disease. An optimal therapy has been started; what is the benefit of a treatment with PCI of the culprit lesion?
a.PCI would reduce the risk of death, MI, or other major CV events when added to optimal medical therapy (OMT).
b.PCI may reduce the episodes of angina in the presence of moderate-to-severe ischemia at stress single-photon emission computed tomography (SPECT) but not the risk of death, MI, or other major CV events when added to OMT.
c.PCI would not reduce the risk of death, MI, angina episodes, or other CV events when added to OMT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


