Coronary Artery Bypass Surgery
Joseph F. Sabik III
Overview
The discovery of coronary cineangiography by Mason Sones at the Cleveland Clinic in Cleveland, Ohio, in the 1960s laid the foundation for the development of coronary artery bypass surgery (1). Now in its fourth decade, coronary artery bypass surgery is one of the great success stories of medicine. It has been shown to prolong survival, relieve angina, and improve exercise tolerance in patients with coronary artery disease. Excellent early and late outcomes are the result of advances in surgical technique, myocardial protection, conduit selection, anesthesia, and postoperative care.
History
In 1951, Vineberg and Miller reported on direct implantation of an internal thoracic artery into the myocardium to improve blood flow (2). Although this operation was shown to improve myocardial blood flow, the blood flow of the implant was too limited in quantity and distribution to be effective (3). Other early approaches to improving myocardial blood flow included coronary endarterectomy by Longmire and patch grafting by Senning (4,5).
Kolessov in Leningrad, Effler and Favaloro in Cleveland, and Garrett and DeBakey in Houston, Texas, were some of the first surgeons in the 1960s to treat coronary artery disease directly with bypass grafts (6,7,8,9). With the development of selective coronary cineangiography by Mason Sones, Rene Favaloro at the Cleveland Clinic demonstrated the safety and efficacy of using saphenous vein as conduits in the treatment of left main, single-vessel, and multivessel coronary artery disease. By 1971, this group had performed more than 700 surgical myocardial revascularizations with saphenous veins (10).
The first direct left internal thoracic artery to left anterior coronary artery bypass revascularization was performed by Demikov in 1953; and in 1967, Kolessov reported performing the same procedure (11,12). Green and colleagues were early proponents of using internal thoracic arteries as bypass grafts and in the 1970s popularized its use (13). Growth of surgical myocardial revascularization exploded, and within a decade it became the most common surgical procedure performed in the United States (14).
Indications
Chronic Stable Angina
The goals of surgical myocardial revascularization are to prolong life, relieve angina, preserve myocardial function, and improve exercise capacity. Much of what is known about the indications for coronary surgery was obtained from the randomized trials of the 1970s, which compared initial surgical therapy with medical therapy for patients with mild to moderate angina and coronary artery disease. These studies were the Veterans Administration Study, the European Cooperative Surgical Study, and the Coronary Artery Surgery Study (15,16,17,18,19,20,21,22). Although patient inclusion criteria for the these trials were different, all three studies had the same objective: to determine whether initial coronary artery bypass surgery or medical therapy improved the survival of patients with surgically approachable coronary artery disease and mild to moderate angina. In applying the findings of these trials to identify patients who benefit from surgical revascularization, it is important to appreciate that only low-risk, stable, male patients were included in these trials. In addition, since the randomized studies were conducted, substantial improvements in both the surgical and medical therapy of coronary artery disease have occurred. These include lipid-lowering drugs, antiplatelet agents, β-blockers, angiotensin-converting enzyme inhibitors, internal thoracic artery grafting, better myocardial protection, and
percutaneous coronary intervention. The randomized trials found both clinical and angiographic factors, such as location and extent of coronary disease, left ventricular dysfunction, severity of angina, and stress testing, useful in identifying patients in whom surgical revascularization is indicated.
percutaneous coronary intervention. The randomized trials found both clinical and angiographic factors, such as location and extent of coronary disease, left ventricular dysfunction, severity of angina, and stress testing, useful in identifying patients in whom surgical revascularization is indicated.
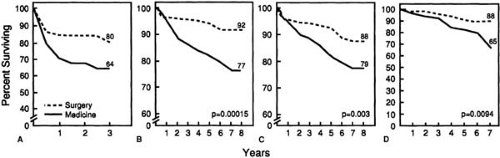
Survival
Improved survival was found in patients treated with surgical revascularization who had left main disease (stenosis ≥50%), left main equivalent disease (stenosis ≥70% of the proximal left anterior descending and circumflex), three-vessel coronary artery disease (stenosis ≥50% in three epicardial coronary arteries), or one- or two-vessel disease that included the proximal left anterior descending coronary artery (stenosis ≥50% in one or two coronary arteries including the left anterior descending artery) (Fig. 80.1) (16,17,22). Patients with worse left ventricular dysfunction derived more survival benefit from surgical revascularization than patients with normal ventricular function, and similarly patients with greater clinical risk factors (severity of angina, positive stress tests, ST-segment depression at rest, history of myocardial infarction, and hypertension) derived more survival benefit from surgical revascularization than patients with few or no risk factors (16,18,22). The more severe the coronary disease, symptoms, and left ventricular dysfunction, the greater was the benefit of surgical revascularization over medical therapy on survival (15,17).
As stated earlier, these trials demonstrated the importance of left ventricular dysfunction in determining which patients obtain a survival benefit from coronary artery bypass surgery (22). However, no patients included in the randomized trials had an ejection fraction less than 35%. Observational studies have demonstrated a survival benefit of surgical revascularization in patients with coronary artery disease and ejection fractions less than 35%, particularly when the patients’ primary symptom was angina (suggesting myocardial viability), and not dyspnea (suggesting myocardial scarring) (23,24,25). In the Coronary Artery Surgery Study Registry, patients whose primary symptom was angina derived a survival advantage with coronary surgery, whereas those whose primary symptom was dyspnea did not (23). This was an early demonstration of the importance of myocardial viability in determining which patients with ventricular dysfunction benefit from surgical revascularization. Noninvasive tests, such as positron emission tomographic scanning, radioisotope imaging, and dobutamine echocardiography, can be used to identify hibernating (viable but nonfunctioning) myocardium to help determine which patients with left ventricular dysfunction may benefit from revascularization (26,27,28,29,30,31,32). Observational studies have shown both a functional and a survival advantage of surgical revascularization in patients with left ventricular dysfunction and substantial myocardial viability on preoperative testing (33).
Quality of Life
In addition to prolonging life, coronary artery bypass surgery was found in the randomized trials to be more effective than medical therapy in decreasing the symptoms of ischemia and in improving quality of life. These studies demonstrated a decrease in angina, an increase in exercise capacity, and a decrease in antianginal medical therapy in patients treated surgically independent of the severity of coronary artery disease (18,21). However, the risk of subsequent myocardial infarction was not lowered in the surgically treated patients in the randomized trials, although registry studies have suggested a lower risk of subsequent myocardial infarctions in patients treated with surgical revascularization.
Unstable Angina
Early studies reported that coronary artery bypass surgery was effective in relieving ischemia in patients with unstable angina (34). However, no survival benefit with surgery was found in these early studies because of the increased hospital mortality of surgical patients with unstable angina. Not until the randomized Veterans Administration Cooperative Study was surgical revascularization found to improve survival in some subsets of patients with unstable angina (35,36,37). This study compared the outcomes of patients with unstable angina who were treated either medically or surgically. Patients were classified by extent of coronary artery disease, ventricular dysfunction, and severity of unstable angina. Patients with left main stenosis were excluded. Coronary revascularization was found to improve survival in patients with (a) triple-vessel coronary artery disease; (b) left ventricular dysfunction, and (c) both left ventricular dysfunction and severe angina at rest (ST-segment and T-wave changes) (36). In addition, the Veterans Administration Cooperative Study also found that quality of life was better in surgically treated patients. Patients treated with coronary revascularization were found to have less angina, to require less antianginal medication, to have increased exercise tolerance, and to have fewer hospital admissions for cardiovascular reasons than patients treated medically (36,37).
Acute Myocardial Infarction
Technique of Operation
The goal of coronary artery surgery is to obtain complete revascularization by bypassing all coronary arteries of sufficient size that have proximal stenosis ≥ 50%. The two most commonly used bypass graft conduits are saphenous veins and internal thoracic arteries. Less commonly used arterial grafts include radial, gastroepiploic, and inferior epigastric arteries. Most coronary artery bypass operations are performed through a median sternotomy. This approach has multiple advantages: (a) access to the ascending aorta and right atrium for central cannulation during on-pump procedures, (b) access to all coronary arteries, (c) ability to harvest both internal thoracic arteries and the right gastroepiploic artery, and (d) ability to perform concomitant cardiac procedures such as valve or aortic replacement. Other approaches that are useful in specific situations of limited coronary revascularization include anterior and lateral thoracotomies, partial sternotomies, parasternotomies, and epigastric incisions (40). Conduit harvesting and preparation occur during and after completion of the median sternotomy. Today, coronary artery bypass surgery is usually performed with the assistance of cardiopulmonary bypass and cardioplegic myocardial arrest (on-pump) or without the assistance of cardiopulmonary bypass on a beating heart (off-pump).
On-Pump Procedure
After the median sternotomy has been completed and all bypass conduits have been harvested, cannulation for cardiopulmonary bypass is performed. Heparin is administered, and cannulation is attained by placing cannulas in the ascending aorta for arterial return and in the right atrium for venous drainage. Before cannulation, the aorta should be evaluated for atherosclerosis, and if atherosclerosis makes ascending aortic cannulation unsafe, the ascending aorta should not be cannulated, and the axillary artery should be used for arterial return (41,42). Cardioplegia cannulas are placed in the ascending aorta and coronary sinus for both antegrade and retrograde delivery of cardioplegia during the period of myocardial ischemia.
Cardiopulmonary bypass is begun with flows of 2.0 to 2.2 L/m2 per minute. Systemic arterial blood pressure should be maintained between 50 and 70 mm Hg. In patients with cerebrovascular occlusive arterial disease, it may be beneficial to keep systemic arterial blood pressure higher to maintain adequate cerebral perfusion and prevent neurologic injury. The aorta is clamped proximal to the arterial cannula, thus keeping blood from perfusing the myocardium. The heart is arrested and protected with first antegrade and then retrograde cardioplegia. Cardioplegia should be administered every 15 to 30 minutes during myocardial ischemia. Construction of the coronary artery bypass grafts is then performed. The distal bypass graft to coronary artery anastomoses are constructed first, and then the proximal bypass graft to aortic anastomoses are performed. To reduce the risk of arterial embolization, it is best to perform the proximal anastomoses during the cross-clamp period, thus eliminating the need for tangential and multiple clampings of the aorta. After all bypass graft anastomoses are completed, the aorta is unclamped, allowing blood to perfuse the myocardium once again. When the heart has recovered, weaning from cardiopulmonary bypass is performed, and the cannulas are removed.
Off-Pump Procedure
During off-pump surgery, a major challenge is to be able to position the heart to permit access to all coronary arteries while maintaining adequate hemodynamics and cardiac output. After completion of the median sternotomy and harvesting of bypass conduits, the patient is placed in the Trendelenburg position. This increases preload and helps to maintain cardiac output while the heart is positioned. Next, the operating table is rotated to the right. Because of gravity, the heart rotates to the right, bringing the apex out of the chest and exposing the lateral, inferior, and posterior surfaces of the heart. As the heart is retracted to the right, the right ventricle becomes compressed against the pericardium. To avoid right ventricular compression and hemodynamic collapse, the right pleura is incised along the sternum, and the pericardium is incised posteriorly along the right diaphragm down toward the inferior vena cava. This allows the heart to move into the right side of the chest, thus assisting with exposure of the coronary arteries and preventing right ventricular compression.
To improve exposure of the coronary arteries, traction can be placed on pericardial sutures or on an apical suction device. Coronary artery stabilization is obtained with either compression or suction stabilizers. These stabilizers allow for performance of the coronary to bypass graft anastomosis in a motionless field.
To obtain a bloodless operating field and to prevent ischemia during the construction of the distal anastomosis, intravascular coronary shunts or proximal and distal silastic loops can be used. Heparin is administered before grafting.
The sequence of grafting is important when performing off-pump revascularization. The grafting sequence should be individualized for each patient, depending on anatomic patterns of coronary occlusion and collateralization. The goal is to avoid making large areas of the myocardium ischemic simultaneously. In general, perform bypass grafts to completely occluded, collateralized coronary arteries before grafting
collateralizing arteries. The left internal thoracic artery graft to the left anterior descending bypass graft should be performed early, especially if the left anterior descending is occluded or there is left main stenosis. Proximal anastomosis may be constructed to in situ arterial grafts or to the aorta.
collateralizing arteries. The left internal thoracic artery graft to the left anterior descending bypass graft should be performed early, especially if the left anterior descending is occluded or there is left main stenosis. Proximal anastomosis may be constructed to in situ arterial grafts or to the aorta.
After the patient is decannulated in on-pump procedures and after all bypass grafts are completed in off-pump procedures, heparin is reversed with protamine, and the incisions are closed. Aspirin should be administered 6 to 8 hours postoperatively and continued for at least 1 year.
Conduits
Saphenous Vein
The first conduit used in coronary surgery was saphenous vein, and today, except for revascularization of the left anterior descending coronary artery, the most commonly used conduit in coronary surgery remains saphenous vein. Use of this vein has many benefits. Because of its relatively large diameter and wall characteristics, it is technically easy to use. In addition, patients have plenty of saphenous vein, so there is enough to perform multiple grafts, and it is also long enough to reach any coronary artery.
Early in the experience of coronary artery bypass surgery, the durability and longevity of saphenous vein grafts came into question. One year after surgery, only 80% to 90% of saphenous vein grafts are patent (43,44




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree