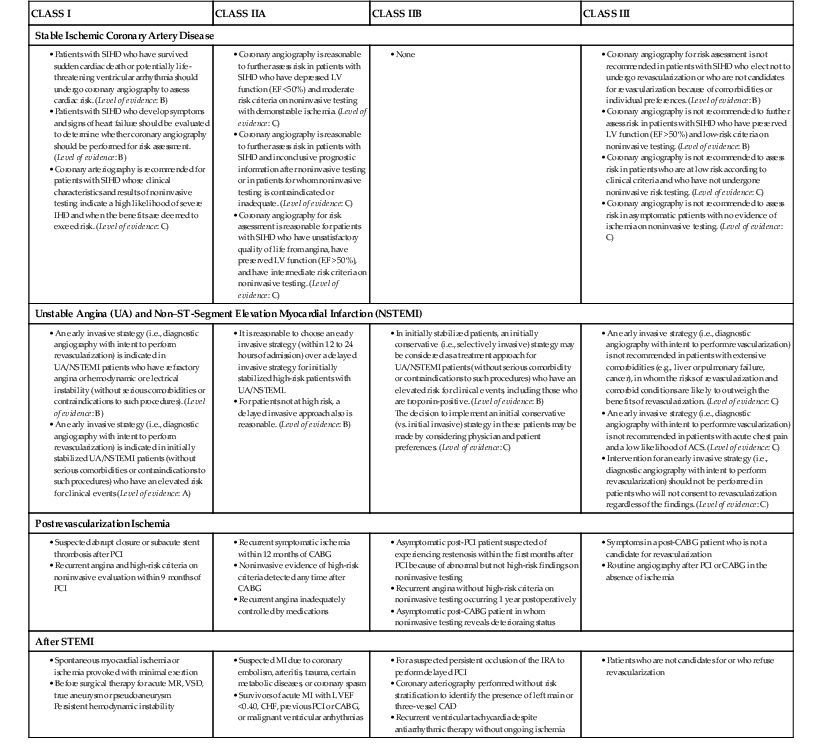
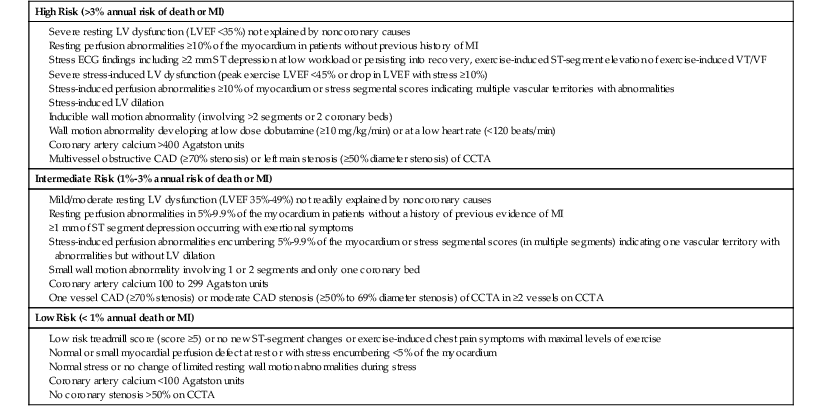
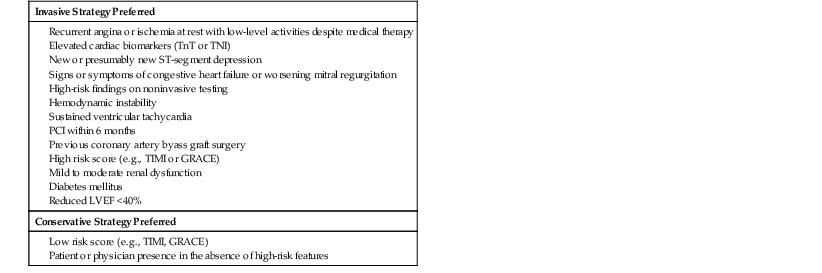
Jeffrey J. Popma, Scott Kinlay, Deepak L. Bhatt Coronary arteriography remains the standard for identifying the presence or absence of arterial narrowings related to atherosclerotic coronary artery disease (CAD) and provides the most reliable anatomic information for determining the appropriateness of medical therapy, percutaneous coronary intervention (PCI), or coronary artery bypass grafting (CABG) in patients with ischemic CAD. First performed by Mason Sones in 1959, coronary arteriography has subsequently become one of the most widely used invasive procedures in cardiovascular medicine.1 It is performed by direct injection of radiopaque contrast material into the coronary arteries and recording high-resolution digital angiograms on exportable radiographic medium. The methods used to perform coronary arteriography have improved substantially since 1959. Smaller (sizes 4F and 5F), high-flow injection catheters have replaced larger (8F) thick-walled ones, and the reduced sheath size has allowed same-day coronary arteriography, ambulation, and discharge. Complication rates have fallen as a result of a better understanding of the periprocedural management of patients undergoing cardiac catheterization. Transradial access has further reduced vascular complication rates and allows early ambulation after the procedure. Digital angiographic laboratories now permit high-quality image acquisition, electronic storage, and rapid image transfer and dissemination. Almost 2 million patients will undergo coronary arteriography in the United States this year. Cardiac catheterization is available in more than 80% of U.S. hospitals, and approximately 20% of these centers also provide cardiac surgery services.2 Although the number of patients undergoing coronary arteriography has plateaued in the United States, more routine cardiac catheterizations are being performed in the community setting, often without cardiac surgical services on site.2 This chapter reviews the indications, risks, techniques, and program oversight for coronary arteriography; the normal coronary anatomy and pathologic coronary variants; the qualitative and quantitative angiographic methods to assess severity of stenoses; and the potential technical pitfalls of coronary angiography for assessing the extent of CAD. This chapter also provides an overview of the current and evolving methods for intracoronary imaging. Coronary arteriography establishes the presence or absence of coronary stenoses and aids in the determination of therapeutic options for revascularization. Its role as the initial diagnostic tool for determining prognosis in patients with suspected CAD has been challenged as a result of the relatively low rates of disease in patients without symptoms or suggestive findings on noninvasive studies.3 The 2012 Multi-Society Guidelines for the Diagnosis and Management of Patients with Stable Ischemic Heart Disease has provided recommendations for the use of coronary arteriography as a supplement to symptom status and noninvasive studies4 (Table 20-1). Furthermore, the Appropriate Use Criteria (AUC) Task Force has evaluated a number of clinically relevant scenarios for coronary angiography and revascularization.5,6 Based on the predominance of the evidence that includes (1) the clinical presentation (e.g., stable angina or an acute coronary syndrome), (2) the severity of angina, (3) the response to medical therapy, (4) magnitude of ischemia as determined by noninvasive testing, and (5) the extent of anatomic disease and its complexity, coronary revascularization is deemed “appropriate,” “may be appropriate,” or “rarely appropriate.”5,6 The AUC are used commonly in the cardiac catheterization laboratory to document indications for coronary arteriography and revascularization. The frequency of normal or insignificant CAD with diagnostic coronary arteriography ranges from 20% to 39%, depending on the types of patients studied (e.g., stable angina versus acute coronary syndrome).2 TABLE 20-1 Indications for Coronary Arteriography* • None • In initially stabilized patients, an initially conservative (i.e., selectively invasive) strategy may be considered as a treatment approach for UA/NSTEMI patients (without serious comorbidity or contraindications to such procedures) who have an elevated risk for clinical events, including those who are troponin-positive. (Level of evidence: B) * Class definitions: Class I: conditions for which there is agreement that the procedure is useful and effective. Class IIa: weight of the evidence is in favor of usefulness and efficacy. Class IIb: weight of the evidence is less well established by evidence and opinion. Class III: conditions for which there is general agreement that the procedure is not useful and effective and in some cases may be harmful. CCS = Canadian Cardiovascular Society; CHF = congestive heart failure; EBCT = electron beam computed tomography; IRA = infarct-related artery; LV = left ventricular; LVEF = left ventricular ejection fraction; MR = mitral regurgitation; NQWMI = non–Q wave MI; QOL = quality of life; VSD = ventricular septal defect; VT = ventricular tachycardia. From Fihn SD, Gardin JM, Abrams J, et al: 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 60:e44, 2012; Anderson JL, Adams CD, Antman EM, et al: 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61:e179, 2013; and Scanlon P, Faxon D, Audet A, et al: ACC/AHA Guidelines for coronary angiography. J Am Coll Cardiol 33:1756, 1999. Coronary arteriography is increasingly performed in community-based cardiac catheterization laboratories without on-site cardiac surgery. Although the risk of adverse events associated with coronary arteriography is low at such centers, patients with pulmonary edema resulting from ischemia, patients with complex congenital disease, and pediatric patients should still be referred to centers with on-site surgery in the event that complications occur.2 Minimal-volume criteria for cardiac catheterization are lacking; nevertheless, operators should be proficient in the performance of coronary arteriography and perform their procedures at hospitals that have established policies to ensure patient safety.7 A dedicated quality assurance program is mandatory for all facilities that offer coronary arteriography, to ensure that the complication rates are not excessive.2 Coronary arteriography is recommended as an initial diagnostic test for the evaluation of CAD in two settings: patients with stable ischemic heart disease who have survived sudden cardiac death or have potentially lethal ventricular arrhythmias and patients who develop worsening symptoms of congestive heart failure when exercise testing is not feasible.4 In other patients with stable ischemic heart disease, noninvasive stress testing is recommended as the initial assessment tool for the detection of CAD (see Chapters 14 and 16).4 Coronary arteriography is recommended to assess risk when noninvasive testing indicates a high likelihood of ischemic heart disease and when the benefits are deemed to exceed the risks4 (Table 20-2). Coronary arteriography is a reasonable investigational strategy to further assess risk in patients with left ventricular (LV) dysfunction (i.e., LV ejection fraction <50%) in whom noninvasive testing yields evidence of ischemia, in those patients in whom such testing provides inconclusive evidence, or in patients for whom noninvasive testing is contraindicated or inadequate.4 Coronary arteriography also constitutes a reasonable assessment option in patients with stable ischemic heart disease who report an unsatisfactory quality of life because of angina, on a background of preservation of ventricular function, and in whom noninvasive testing reveals intermediate risk criteria.4 TABLE 20-2 Risk Stratification in Patients with Stable Ischemic Coronary Artery Disease Severe resting LV dysfunction (LVEF <35%) not explained by noncoronary causes Resting perfusion abnormalities ≥10% of the myocardium in patients without previous history of MI Severe stress-induced LV dysfunction (peak exercise LVEF <45% or drop in LVEF with stress ≥10%) Inducible wall motion abnormality (involving >2 segments or 2 coronary beds) Coronary artery calcium >400 Agatston units Multivessel obstructive CAD (≥70% stenosis) or left main stenosis (≥50% diameter stenosis) of CCTA CCTA = coronary CT angiography; ECG = electrocardiogram; LV = left ventricle; LVEF = left ventricular ejection fraction; MI = myocardial infarction; VT/VF = ventricular tachycardia/ventricular fibrillation. Modified from Fihn SD, Gardin JM, Abrams J, et al: 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 60:e44, 2012. On the basis of studies that failed to show a reduction in death and myocardial infarction (MI) with PCI compared with maximal medical therapy,8 coronary arteriography is not recommended in patients with stable ischemic heart disease who are not candidates for revascularization because of comorbid conditions or personal preference. Coronary arteriography also is not recommended in patients with normal ventricular function and low-risk criteria on noninvasive testing, or those with low-risk criteria in the absence of noninvasive testing.4 Coronary arteriography is not recommended in asymptomatic patients with no evidence of ischemia on noninvasive testing.4 In the absence of symptoms and signs of ischemia, the presence of coronary calcification on fluoroscopy and a high calcium score obtained using cardiac computed tomography (see Chapter 18) are not indications for coronary arteriography. Discussions with patients relating to the risks and benefits of coronary arteriography should be coupled with an outline of the revascularization method in the event that obstructive CAD is identified. Although the performance of CABG generally can be deferred until after a discussion with the cardiac surgeon, the vast majority of PCIs are performed on “ad hoc” basis or at the same time as coronary arteriography.2 An early invasive strategy is defined as diagnostic angiography with an intent to perform revascularization in patients who present with unstable angina or non–ST-segment elevation MI (NSTEMI) (see Table 20-1).9 An early invasive strategy is indicated in those patients who have refractory angina or hemodynamic instabilities and in those who initially are stabilized but are at elevated risk for recurrent clinical events9 (Table 20-3). An early invasive strategy is reasonable within the first 12 to 24 hours in both patients at high risk and those not at high risk for clinical events.9 An early invasive strategy is not recommended in patients with extensive comorbid disease, in whom the risks are likely to outweigh the benefits of revascularization, and in patients with acute chest pain but a low likelihood of an acute coronary syndrome (see Chapters 52 and 53).9 TABLE 20-3 Risk Stratification in Patients with Unstable Angina and Non–ST-Segment Elevation Myocardial Infarction GRACE = Global Registry of Acute Coronary Events; PCI = percutaneous coronary intervention; TIMI = Thrombolysis in Myocardial Infarction; TnI = troponin I; TnT = troponin T. Modified from Anderson JL, Adams CD, Antman EM, et al: 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61:e179, 2013. Patients who should undergo coronary arteriography are patients with ST-segment elevation MI (STEMI), NSTEMI, or unstable angina who experience spontaneous ischemia; patients who experience ischemia at a minimal workload; and patients in whom MI is complicated by heart failure, hemodynamic instability, cardiac arrest, mitral regurgitation, or ventricular septal rupture.10 Patients with angina or provocable ischemia after MI also should undergo coronary arteriography, because revascularization may reduce the high risk of reinfarction in such cases.10 Coronary arteriography should be performed in patients scheduled to undergo noncardiac surgery who demonstrate high-risk criteria on noninvasive testing, those with angina unresponsive to medical therapy or unstable angina, and those with equivocal results on noninvasive testing combined with high-risk surgical factors (see Table 20-1).11 Coronary arteriography also is recommended for patients scheduled to undergo surgery for valvular heart disease or congenital heart disease, particularly those with multiple cardiac risk factors and those with infective endocarditis and evidence of coronary embolization (see Chapters 62 to 64).11 Coronary arteriography should be performed annually in patients after cardiac transplantation (see Chapter 28), even in the absence of clinical symptoms, because of the characteristically diffuse and asymptomatic nature of graft atherosclerosis. Coronary arteriography is useful in potential donors for cardiac transplantation whose age or cardiac risk profile increases the likelihood of CAD.11
Coronary Arteriography and Intracoronary Imaging
Overview and Background
Indications and Contraindications for Coronary Arteriography
CLASS I
CLASS IIA
CLASS IIB
CLASS III
Stable Ischemic Coronary Artery Disease
Unstable Angina (UA) and Non–ST-Segment Elevation Myocardial Infarction (NSTEMI)
The decision to implement an initial conservative (vs. initial invasive) strategy in these patients may be made by considering physician and patient preferences. (Level of evidence: C)
Postrevascularization Ischemia
After STEMI
Chronic Stable Angina
High Risk (>3% annual risk of death or MI)
Intermediate Risk (1%-3% annual risk of death or MI)
Low Risk (< 1% annual death or MI)
Acute Coronary Syndromes
Other Conditions Warranting Coronary Arteriography
Coronary Arteriography and Intracoronary Imaging
20



