Traditional imaging for ablation of supraventricular tachycardia has been fluoroscopy, although 3-dimensional electroanatomic mapping (3D) has been demonstrated to reduce radiation exposure. This study compares a technique for the reduction of radiation, low-dose fluoroscopy (LD), with standard-dose fluoroscopy (SD) and 3D with SD (3D-SD). This was a single institutional retrospective cohort study. All patients undergoing initial ablation for atrioventricular reentrant tachycardia (AVRT) or atrioventricular nodal reentrant tachycardia (AVNRT) from 2009 to 2012 were reviewed and divided into 3 groups: (1) SD, (2) 3D (CARTO or NavX) with SD, or (3) LD. LD uses the same equipment as SD but includes customized changes to the manufacturer’s lowest settings by decreasing the requested dose to the detector. Primary outcomes were fluoroscopy time and dose area product exposure. One hundred eighty-one patients were included. The median age was 15.0 years (3.3–20.8); 59% had AVRT, 35% had AVNRT, and 6% had both AVRT and AVNRT. LD decreased the dose area product (DAP) compared with SD (637.0 vs 960.1 cGy*cm 2 , p = 0.01) with no difference in fluoroscopy time. 3D-SD decreased fluoroscopy time compared with SD (9.9 vs 18.3 minutes, p <0.001) with DAP of 570.1.0 versus 960.1 cGy*cm 2 (p = 0.16). LD and 3D-SD had comparable DAP (637.0 vs 570.1 cGy*cm 2 , p = 0.67), even though LD had significantly longer fluoroscopy time (19.9 vs 9.9 minutes, p <0.001). In conclusion, LD during catheter ablation of AVRT and AVNRT significantly reduced the DAP compared with SD and had similar radiation exposure compared with 3D with SD.
Radiation effects of fluoroscopy are known to have both deterministic and stochastic effects on patients. Deterministic effects such as skin injury are dose dependent, and typically such doses are not reached during electrophysiology studies with ablation. In contrast, stochastic effects such as the development of cancer occur by chance without a threshold level for which no effect is seen. Ionizing radiation has long been known to increase the risk for development of cancer, and the World Health Organization has officially classified x-rays as a carcinogen. This concern has led to the attempt to limit radiation exposure to children, including patients undergoing catheter ablation, with the goal of ALARA (as low as is reasonably achievable). In pediatric catheter ablations over the past 20 years, fluoroscopy times have decreased, whereas success rates have increased. In an attempt to limit or eliminate the need for fluoroscopy, nonfluoroscopic magnetic and impedance electroanatomic mapping systems have been advocated and have been shown to decrease fluoroscopy times and radiation doses in the treatment of supraventricular tachycardia in children. We made novel modifications to the fluoroscopic imaging system in our electrophysiology laboratory to reduce the fluoroscopy dose, which we describe as low-dose (LD) fluoroscopy. The primary aim of this study was to determine the dose area product (DAP) and fluoroscopy times for patients who had procedures using LD fluoroscopy and compare this technique to procedures using standard low-dose (SD) fluoroscopy settings and procedures with 3-dimensional electroanatomic mapping (3D-SD) with standard-dose fluoroscopy.
Methods
We performed a retrospective cohort study of patients at a single pediatric institution with Cincinnati Children’s Hospital Medical Center Institutional Review Board approval (ID#: 2011-2846). The patients underwent an electrophysiology study with catheter ablation between January 2009 and February 2012. Patients who underwent initial ablation for atrioventricular reentrant tachycardia (AVRT) or atrioventricular nodal reentrant tachycardia (AVNRT) were included. Three experienced pediatric electrophysiologists performed the procedures. Patients <3 years of age and >21 years of age were excluded from the study. Patients with repeat catheter ablation procedures or procedures for other forms of supraventricular tachycardia (atrial tachycardia, intraatrial reentrant tachycardia, atrial fibrillation) and ventricular tachycardia were excluded from the study.
Patients were divided into 3 groups based on fluoroscopy type and whether 3-dimensional electroanatomic mapping was used during the procedure. The 3 groups included patients undergoing (1) SD fluoroscopy, (2) 3D-SD, or (3) LD. All 3 fluoroscopy groups used the Phillips Allura RD 10/10 biplane (Philips Healthcare, Andover, Massachusetts) cardiovascular x-ray system using a 0.9-mm copper filter in the collimator. The SD group used the fluoroscopy system alone for imaging with no modifications (requested dose to the detector of 310 nGy per second). The 3D-SD fluoroscopy group used 3D electroanatomic mapping systems with adjunct fluoroscopy imaging, which was the same as the SD group fluoroscopy settings. The electroanatomic systems used were CARTO (Biosense Webster, Diamond Bar, California) or EnSite NavX (St Jude Medical, St. Paul, Minnesota). The electroanatomic mapping was used with an intent to decrease fluoroscopy time but not to eliminate fluoroscopy completely. Our electrophysiologists were experienced with the use of electroanatomic mapping before the initiation of this study. Three-dimensional electroanatomic mapping was used for imaging during catheter manipulation, mapping of arrhythmia substrate, and catheter placement.
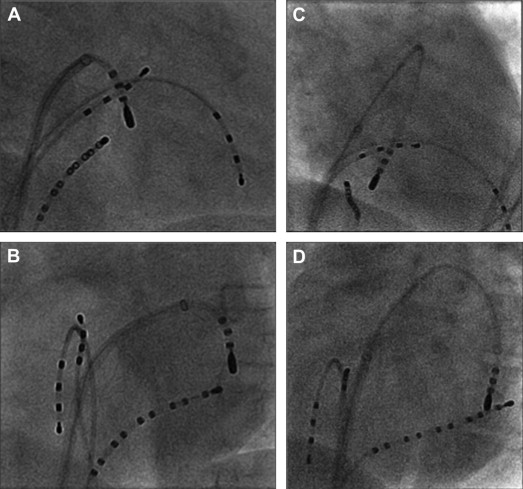
The LD fluoroscopy group used customized changes to the Phillips Allura RD 10/10 biplane system’s lowest fluoroscopy settings by decreasing the requested dose to the detector from 310 to 155 nGy per second ( Table 1 ). The difference in visual appearance between the 2 methods is demonstrated in Figure 1 . The pulse rate for all 3 groups was the same at 15 frames per second. Fluoroscopy was used for wire placement during central venous access, imaging during catheter manipulation, and for catheter placement during ablation. The standard protocol was to save a biplane image with each ablation lesion as a fluoroscopy saved image that used the same dose of fluoroscopy as a standard biplane image. Our standard of care is to reduce radiation exposure to each patient by coning down the images eliminating radiation to regions not of interest and placing the flat plate as close to the patient as possible.
| Fluoroscopy Group | Requested Dose | 3D Mapping |
|---|---|---|
| SD | 310 nGy/s | No |
| 3D-SD | 310 nGy/s | Yes |
| LD | 155 nGy/s | No |
Before the customized changes to LD fluoroscopy, electroanatomic mapping was used as a trial to explore the use of this technique for the purpose of assessing efficacy of the different systems and reducing fluoroscopy time. The customized changes to LD were initiated in April 2011; therefore, all patients after that date received LD fluoroscopy. Patients in which 3D was used with adjunctive LD were excluded from this study.
General anesthesia or sedation was used for all electrophysiology studies. Patients had catheters positioned in the high right atrium, right ventricular apex, and the His bundle recording area. Catheter placement in the coronary sinus was placed based on electrophysiologist preference. Baseline intracardiac intervals, incremental atrial pacing, atrial extra-stimulus testing, incremental ventricular pacing, and ventricular extra-stimulus testing were performed in baseline conditions and with isoproterenol if needed to induce tachycardia.
Standard baseline electrophysiologic assessment and documentation of AVRT or AVNRT were performed. If the patient had a left-sided accessory pathway, an atrial septal puncture was performed with or without a SafeSept wire (Pressure Products, San Pedro, California) based on electrophysiologist preference. During the atrial transseptal procedure the fluoroscopy setting was typically changed from LD to SD to improve image quality until the placement of the transseptal sheath, at which point the fluoroscopy was returned to LD settings. Radiofrequency ablation was performed with a #7 French radiofrequency catheter and/or cryoablation was performed with a #7 French cryoablation catheter. Following completion of the successful lesion or lesion line, incremental, and extra-stimulus atrial and ventricular testing were repeated both on and off isoproterenol for 60 minutes.
Demographic data was obtained on all patients. Procedural data were obtained from our electrophysiology and general cardiology databases. The primary outcome variables were fluoroscopy time and DAP (cGy*cm 2 ). Secondary outcome variables included procedure length and procedural success. Independent variables included mechanism of tachycardia (AVNRT or AVRT), accessory pathway location, and type of ablation: radiofrequency and/or cryoablation, procedural complications, and number of lesions. Procedural length was measured from the placement of venous sheaths to removal of venous sheaths after 1-hour of postablation testing. Procedural acute success was defined as (1) AVRT: no evidence of accessory pathway conduction and no inducible AVRT, and (2) AVNRT: no inducible AVNRT with no more than a single AV nodal echo beat. These criteria were fulfilled after 60 minutes of postablation testing. Complications were defined as permanent second- or third-degree AV block, vascular or cardiac injury, and pericardial effusion.
Statistical analysis was performed using Stata 10.0 analysis software (Stata Corporation, College Station, Texas). All continuous variables were described and tested for central tendency to determine the normality of the data distribution. Normally distributed continuous variables are expressed as means ± SD. Non–normally distributed data are expressed using the median value and range. Univariate analyses was performed using the Wilcoxon rank-sum test for continuous variables and the Fischer exact test for dichotomous variables. Multivariate analysis was performed using analysis of variance. Because multiple group comparisons were performed, a Bonferroni correction was used, and a p value of <0.0167 was considered significant.
Results
From January 2009 to February 2012, 181 patients met inclusion criteria and all were included in analysis. Baseline demographic data on these patients are listed in Table 2 . There were no demographic or procedural differences between the fluoroscopy groups ( Table 2 ). There were no differences in body surface area, mechanism of tachycardia, accessory pathway location, procedure length, success rates, complication rates, and number of lesions between the 3 groups ( Table 2 ).
| Demographic data | Total (n = 181) | SD (n = 117) | 3D-SD (n = 26) | LD (n = 38) |
|---|---|---|---|---|
| Age (yrs) | 15.0 (3.3–20.8) | 14.7 (3.3–20.8) | 15.7 (10.3–18.9) | 14.4 (5.3–19.2) |
| Weight (kg) | 55.7 (14.8–128.4) | 53.8 (14.8–128.4) | 59.1 (25.8–127.3) | 53.5 (19.7–103.6) |
| Height (cm) | 163 (78–192) | 164 (78–192) | 164 (133–186) | 161 (111–192) |
| Body surface area (m 2 ) | 1.6 (0.6–2.6) | 1.6 (0.6–2.6) | 1.7 (1–2.5) | 1.6 (0.8–2.4) |
| Male | 97 (54%) | 63 (54%) | 12 (46%) | 22 (58%) |
| Mechanism of tachycardia | ||||
| AVRT | 107 (59%) | 64 (55%) | 19 (73%) | 24 (63%) |
| AVNRT | 64 (35%) | 45 (38%) | 7 (27%) | 12 (32%) |
| Both | 10 (6%) | 8 (7%) | 0 | 2 (5%) |
| Accessory pathway location, n | 124 | 75 | 21 | 28 |
| Left | 86 (69%) | 57 (76%) | 9 (43%) | 20 (71%) |
| Right | 16 (13%) | 5 (7%) | 8 (38%) | 3 (11%) |
| Septal | 22 (18%) | 13 (17%) | 4 (19%) | 5 (18%) |
| Multiple | 8 | 3 | 2 | 3 |
| Procedure length (h) | 3.6 (1.9–11.7) | 3.5 (2.2–8.4) | 3.6 (2.6–11.7) | 4.0 (1.9–7.4) |
| Acute success | 177/181 (98%) | 114/117 (97%) | 26/26 (100%) | 37/38 (97%) |
| Complications | 2 (1%) | 2 (1.7%) | 0 | 0 |
| Type of ablation | ||||
| Radiofrequency | 85 (47%) | 53 (45%) | 15 (58%) | 17 (45%) |
| Cryoablation | 75 (41%) | 49 (42%) | 10 (38%) | 16 (42%) |
| Both | 21 (12%) | 15 (13%) | 1 (4%) | 5 (13%) |
| Number of lesions | 7 (1–38) | 7 (1–33) | 7 (1–38) | 6 (1–20) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


