Conglomerate Mass (Progressive Massive Fibrosis)
Jeffrey P. Kanne, MD
DIFFERENTIAL DIAGNOSIS
Common
Sarcoidosis
Radiation-Induced Lung Disease
Less Common
Silicosis/Coal Worker’s Pneumoconiosis
Diffuse Alveolar Hemorrhage
Rare but Important
Lipoid Pneumonia
Pulmonary Talcosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Significant overlap of findings between sarcoidosis and silicosis and coal worker’s pneumoconiosis
Occupational and exposure history important
Knowledge of treatment plan useful for recognizing radiation-induced lung fibrosis
Important for distinguishing radiation-induced lung disease from recurrent neoplasm
Helpful Clues for Common Diagnoses
Sarcoidosis
Develops with progressive sarcoid-induced fibrosis
Conglomerate fibrosis difficult to distinguish from silicosis or coal worker’s pneumoconiosis
Upper and mid lung zone predominant
Air bronchograms usually present
Associated traction bronchiectasis, architectural distortion, and volume loss
Punctate or coarse calcification frequently present
Perilymphatic nodules typically present bilaterally
Paracicatricial emphysema common peripheral to conglomerate mass
Increases with progressive fibrosis
Cavitation may occur from necrosis or infection
Mycobacterium species
Mediastinal and bilateral hilar lymphadenopathy often present
May be calcified (solid or “egg shell”)
Honeycombing less common than with other end-stage lung diseases
Cysts usually larger
Basal sparing typical
Radiation-Induced Lung Disease
Most commonly result of radiation for lung carcinoma
Less commonly for mediastinal lymphoma, esophageal carcinoma, or breast carcinoma
Radiation fibrosis
Typically occurs 6-12 months after completion of radiation therapy
Occurs within radiation field and can cross anatomic boundaries, such as pulmonary fissures
Straight lateral and medial margins with conventional therapy
May begin as small consolidative or ground-glass attenuation lung nodules
Nodules coalesce over time to form larger areas of fibrosis
Newer 3D radiation therapy techniques can result in lung abnormalities away from primary disease
Should stabilize within 2 years following therapy
Helpful Clues for Less Common Diagnoses
Silicosis/Coal Worker’s Pneumoconiosis
Exposure to coal dust or free silica
Coal miners
Quarry workers
Sand blasters
Foundry workers
Ceramics workers
Concrete cutters
Typically develops after 20 years of exposure
Can develop < 10 years with exposure to very high concentrations of dust
Progresses despite cessation of exposure
Silicosis and coal worker’s pneumoconiosis indistinguishable radiographically
Large opacities > 1-2 cm
Begins in periphery of lung
Round or oval nodule or mass
Well-defined lateral margin paralleling chest wall
Posterior location on lateral radiograph or CT
Unilateral or asymmetric in early stages
Becomes symmetric with progressive disease
Difficult to distinguish from sarcoidosis
Develops in upper lobes
Air bronchograms less common than with sarcoidosis
Associated with bronchial distortion and upper lobe volume loss
Small perilymphatic nodules usually present
Cavitation may occur from necrosis or infection, especially when > 5 cm
Predisposed to Mycobacterium tuberculosis infection
Punctate calcifications common in conglomerate masses
Mediastinal and hilar lymphadenopathy in up to 40%
Calcification in ˜ 50% (diffuse, central, eccentric, and peripheral “egg shell”)
Paracicatricial emphysema common peripheral to conglomerate mass
Increased risk of lung carcinoma independent of cigarette smoking
Increased risk of developing connective tissue disease, especially systemic sclerosis
Diffuse Alveolar Hemorrhage
Very rare cause of conglomerate mass
Occurs with recurrent alveolar hemorrhage
Subsequent hemosiderosis and fibrosis
Conglomerate mass with high attenuation
Helpful Clues for Rare Diagnoses
Lipoid Pneumonia
Typically result of recurrent lipid aspiration
Most patients asymptomatic
Mineral oil ingestion most common
Occupational exposure to oil mist less frequent
Conglomerate mass with diffuse low attenuation
Usually gravitationally dependent (posterior lower lobes)
Cavitation uncommon
Usually from superinfection with nontuberculous mycobacteria
Pulmonary Talcosis
Frequently results from chronic intravenous drug abuse
Granulomatous vasculitis from foreign body giant cell reaction to contaminants (talc) in drugs
Patients often initially asymptomatic
May progress to respiratory insufficiency and pulmonary hypertension
Early disease
Small nodules
Hyperinflation and emphysema (panlobular or panacinar)
Conglomerate masses develop with progressive disease
Similar to those of silicosis and coal worker’s pneumoconiosis
May have diffuse or punctate calcification
Image Gallery
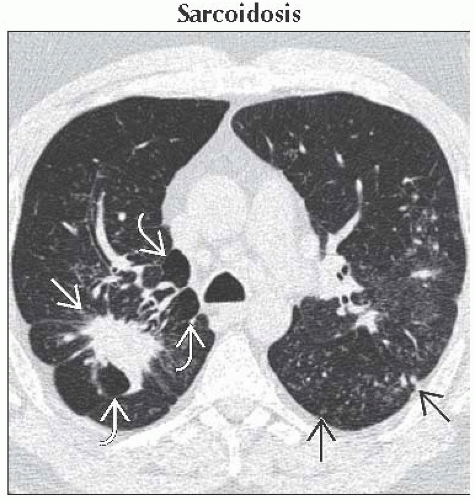 Axial HRCT shows a spiculated mass in the right lower lobe
 . Note the nearby paracicatricial emphysema . Note the nearby paracicatricial emphysema  . Scattered perilymphatic nodules typical of sarcoidosis are seen in the left lung . Scattered perilymphatic nodules typical of sarcoidosis are seen in the left lung  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|