Chapter 7 Congenital Aortic Stenosis
Congenital Aortic Regurgitation
Clinical evaluation of congenital obstruction to left ventricular outflow seeks to establish the presence and degree of obstruction and the level and morphologic type.1–6 Five varieties of congenitally abnormal aortic valves are based on the number and types of cusps and commissures (Box 7-1).6 A unicuspid aortic valve is either acommissural7 or unicommissural.6 A unicuspid acommissural valve is characterized by a single leaflet with a central orifice that is usually stenotic but can be stenotic and regurgitant.7 Traces of three rudimentary commissures do not divide the valve (Figure 7-1A, left upper).6 This type of congenitally stenotic semilunar valve is found in the pulmonary location (see Chapter 11), but rarely in the aortic location.6 A unicommissural unicuspid valve is characterized by a single commissural attachment to the aorta (Figures 7-1A, left middle, and 7-2A).2,6 The single (unicuspid) leaflet originates from a single commissural attachment, proceeds across the aortic orifice without making contact with the aortic wall, bends on itself, and returns to reinsert at the same attachment site from which it originated.2,6 Remnants of rudimentary raphes are occasionally present.6 Viewed from above, the orifice resembles an exclamation point (see Figure 7-1A, left middle).6 The typical unicommissural valve is intrinsically stenotic, but if the free edge is sufficiently redundant and the single commissure is not fused, obstruction is initially absent but subsequently appears when mobility is reduced by fibrosis and calcification.2
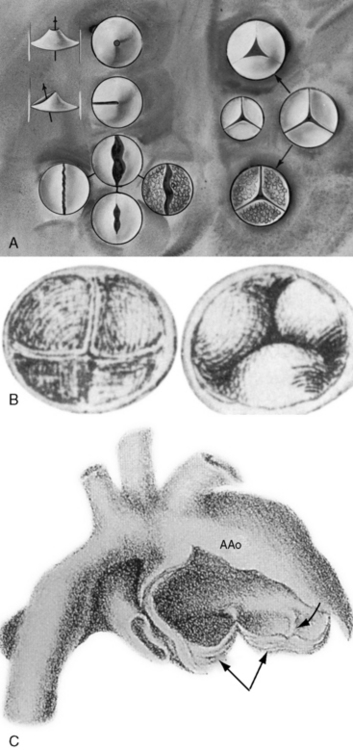
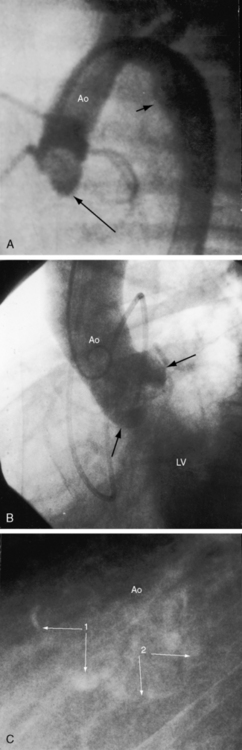
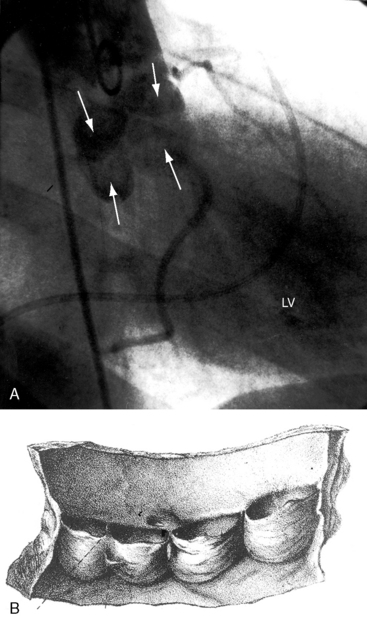
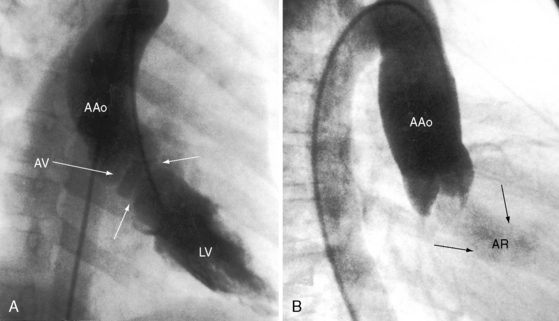
Figure 7-1 A, Illustrations of the various types of aortic valve stenosis. Figure on the left illustrates three types of congenitally abnormal aortic valves. The upper drawing shows a unicuspid acommissural valve. The middle drawing shows a unicuspid unicommissural valve with an eccentric orifice. The lower group of four drawings shows a functionally normal bicuspid aortic valve (upper center), a fibrocalcific stenotic bicuspid aortic valve (center right), a bicuspid aortic that is inherently stenotic because the free edges are not longer than the annular diameter (center left), and a bicuspid aortic valve that is inherently stenotic because of failure of commissural separation (lower center). Illustrations on the right show a normal trileaflet aortic valve with equal cusps and equal commissures (center right). A congenitally hypoplastic trifleaflet aortic valve (center left) is paired beside the normal trileaflet aortic valve (center left). Acquired aortic valve stenosis from fibrosis and calcification without commissural fusion (right lower) or from rheumatic fusion of commissures (upper) is shown. A dysplastic trileaflet valve is not shown. B, Congenital aortic cuspal inequality as represented by Leonardo da Vinci circa 1513.16 His legend read: “Figures of the cusps (aorti) of the gateway which the left ventricle possesses when it closes itself.” On the left is a trileaflet aortic valve as seen from above. On the right is a closed trileaflet aortic valve as seen from below. C, Dilation of the ascending aorta (AAo) above a congenitally bicuspid aortic valve (paired arrows) with a false raphe (curved arrow).
(From Maude Abbott. Atlas of congenital cardiac disease. Montreal: Osler Library, McGill University; 1936. Reproduced with permission.)
A bicuspid aortic valve is the most common congenital anomaly to which that structure is subject (see Figure 7-1A, left lower group)1,2,6 and is the most common gross morphologic congenital abnormality of the heart or great arteries in adults.8 Estimated frequency in the general population has been reported as 0.5% to 0.6%9 and 0.9% to 1.36%,10 with an overall prevalence rate in the United States of approximately four million.4,11 The male:female ratio is 2:1. The bicuspid aortic valve is a genetic disorder, with a transmission pattern that suggests autosomal dominant inheritance.10,12 A low prevalence rate of bicuspid aortic valve is found in African Americans.13 Acquired calcification of a congenitally bicuspid aortic valve accounts for approximately half of surgical cases of isolated aortic stenosis in adults.11,14 Hypercholesterolemia is an atherosclerotic risk factor for the development of calcification.15
The bicuspid aortic valve was first identified in the early 16th century by Leonardo da Vinci in his remarkable Anatomical, Physiological, and Embryological Drawings, released by Dover Publications in a facsimile edition.16 Normal aortic valves are composed of a connective tissue framework of interstitial cells and a matrix covered by endothelial cells. During valvulogenesis, extracellular matrix proteins direct cell differentiation and cusp formation. Differentiation of mesenchymal cells into mature aortic valve cells correlates with the expression of the matrix protein fibrillin-1, which is deficient in bicuspid aortic valve tissue. Three morphologic types of a bicuspid aortic valve based on cusp size are characterized by two cusps of equal size, two cusps of unequal size, and a conjoined cusp twice the size of its nonconjoined mate.11 Three morphologic types based on commissural fusion are characterized by fusion of the right and left coronary cusps (most common), fusion of the right and noncoronary cusps, and fusion of the left and noncoronary cusps (least common).8 A false raphe can be well-formed, fenestrated, calcified, or absent.11,17 If the free edges of the bicuspid leaflets are sufficiently long, if the cusps are thin and mobile, and if the commissures are not fused, the valve is functionally normal—unobstructed—which is the usual condition at birth (see Figure 7-1A, left lower).4–6 Conversely, if the commissures are congenitally fused, or if the free edges of the cusps are not longer than the diameter of the aortic ring, the valve is inherently obstructed (see Figure 7-1A, left lower). Fusion of the right and left coronary cusps is strongly associated with coarctation of the aorta.18 Fusion of the right and noncoronary cusps is associated with valve pathology.18 Sclerosis of a bicuspid aortic valve begins as early as the second decade, and calcification as early as the fourth decade.19 The fibrocalcific process is more rapid in bicuspid aortic valves with cusps of unequal size because of maldistribution of tension during diastolic closure.19 Rarely, a congenital bicuspid aortic valve is stenotic because of myxoid dysplasia.20 Bicuspid aortic and bicuspid pulmonary valves coexist in the Syrian hamster,21 but not in human subjects.
A functionally normal bicuspid aortic valve can continue to function normally throughout a long lifetime,4 but more often than not, fibrocalcific thickening or acquired commissural fusion decreases mobility and renders the valve stenotic (see Figures 7-1A, left lower group, and 7-2C).1,4,11 Thomas Peacock22 recognized this tendency in his On Malformations of the Human Heart (1858). Abnormal mechanical stress is an important factor in promotion of fibrosis and calcification of a bicuspid bicommissural aortic valve (see Figure 7-2C).23 An important consequence of a functionally normal bicuspid aortic valve is progressive regurgitation, which may be accelerated by infective endocarditis to which a bicuspid valve is highly susceptible (see subsequent discussion). Rarely, a severely incompetent bicuspid aortic valve becomes stenotic with virtual loss of regurgitation.24
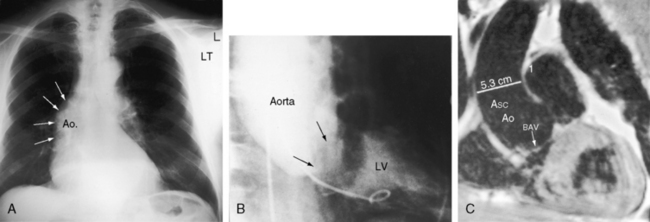
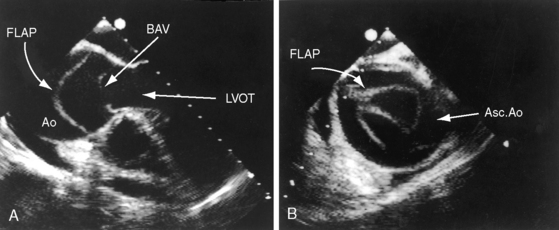
Dilation of the ascending aorta is consistently associated with a congenitally bicuspid aortic valve (Figures 7-1C, 7-3, and 7-4),25–27 but the term poststenotic dilation is a misnomer because the ascending aorta is dilated whether the bicuspid valve is stenotic, incompetent, or functionally normal.28 Dilation is the result of an inherent medial abnormality that expresses itself as an ascending aortic aneurysm with chronic aortic regurgitation (see Figure 7-4) or dramatically as a dissecting aneurysm (Figure 7-5).28–32 A decrease in ascending aortic elasticity is independent of dilation.33,34
Trileaflet aortic valves are congenitally abnormal when three cusps and three commissures are miniaturized within a small aortic ring35 or when an aortic valve is the site of myxoid dysplasia.20 In a hydraulically ideal aortic valve with three equal cusps, diastolic force is equally distributed among the three cusps and their sinus attachments. Cuspal inequality is a common variation of normal in trileaflet aortic valves but results in unequal distribution of diastolic force (see Figure 7-1B).5,36 The fibrocalcific process of aging proceeds more rapidly in the cusp or cusps that bear the greatest hemodynamic stress.11,36 Accordingly, cuspal inequality in a normal trileaflet aortic valve enhances the aging process, converting a functionally normal trileaflet valve into fibrocalcific aortic stenosis.5,36 Similarly, the tendency for a bicuspid aortic valve to become fibrocalcific (see Figure 7-2C) is related in part to the mechanical stress inherent in bicuspid cuspal inequality (see Figure 7-2B).23 The quadricuspid aortic valve, first reported in 1862, can function normally or cause incompetence (Figures 7-35 and 7-42)37 but is rarely stenotic.6 Six-cuspid semilunar valves sporadically occur with truncus arteriosus (see Chapter 28).6
Fixed subaortic stenosis is the second most common variety of congenital obstruction to left ventricular outflow6,38 and accounts for 15% to 20% of all types of congenital aortic stenosis.39 It occurs in isolation (Figure 7-6) or with other congenital cardiac defects.40,41 Nonfixed muscular subaortic stenosis can coexist with severe aortic valve stenosis and can account for as much as half the pressure gradient.40–42
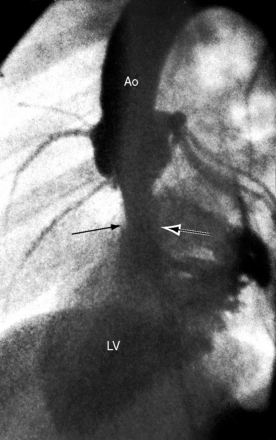
This chapter deals with two principal varieties of fixed subaortic stenosis in hearts that are otherwise devoid of congenital heart disease. The first variety is characterized by a thin fibrous crescent-shaped membrane located immediately beneath the aortic valve (see Figure 7-6A).6,40 The membrane is occasionally relatively thick and forms a fibrous or fibromuscular collar that extends across an otherwise normal left ventricular outflow tract43 and inserts onto the anterior mitral leaflet. This form of fixed subaortic stenosis occurs in human hearts and in dogs, pigs, and cows.44 The aortic root is not dilated.28 Aortic regurgitation is associated with malformed leaflets that are damaged by the proximity of the subvalvular membrane or fibromuscular collar and by the impact of the eccentric systolic jet (see Figure 7-6B).6 Tubular subaortic stenosis is a less common variety of fixed obstruction to left ventricular outflow and is represented by a fibromuscular channel that occupies several centimeters within the outflow tract (Figure 7-7).40,41,45 A layer of fibrous tissue extends onto the ventricular surface of the anterior mitral leaflet. The aortic cusps show fibrous thickening as with discrete subaortic stenosis. The aortic root is not dilated (see Figure 7-7).28,45
Fixed subaortic stenosis as just defined is not present during intrauterine cardiac morphogenesis, is therefore not con genitus, and accordingly is uncommon if not rare in neonates and infants.41 The disorder becomes manifest after the first year of life and then changes in both severity and morphology. In contrast to rapid progression in infants and children, fixed subaortic stenosis in adults progresses slowly.40,41,45,46 Aortic regurgitation is common but is usually mild and nonprogressive (see Figure 7-6B).
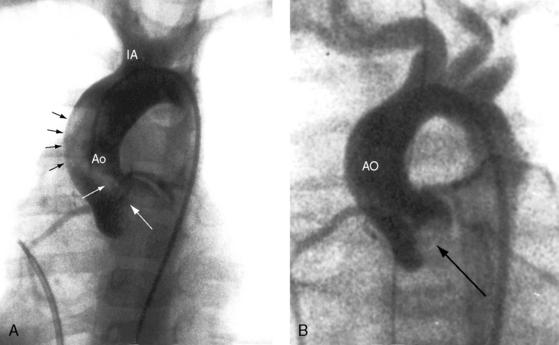
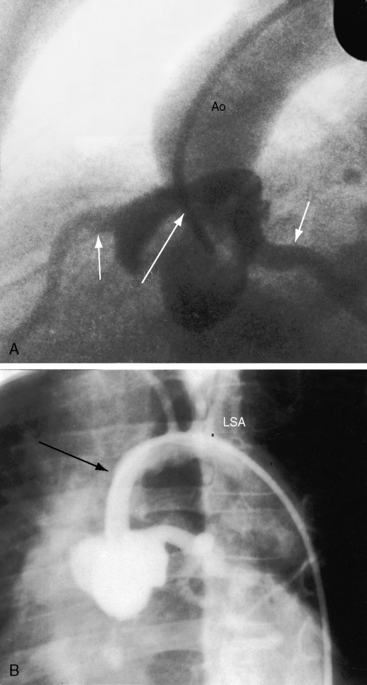
Supravalvular aortic stenosis is the least common variety of congenital obstruction to left ventricular outflow. The most frequent type is a localized segmental hourglass deformity immediately above the aortic sinuses with medial thickening and fibrous intimal proliferation (Figure 7-8A).6 The size of the aorta distal to the obstruction is normal or reduced. The sinuses of Valsalva are enlarged.47 Localized supravalvular aortic stenosis is occasionally caused by a fibrous membrane with a central opening.6 An uncommon variety is represented by tubular hypoplasia of the ascending aorta beginning above the sinuses of Valsalva and associated with narrowing of the orifices of the brachiocephalic arteries (Figure 7-8B).6,48 The aortic leaflets are usually thickened and adherent to the supravalvular stenosing ridge,6,47 are occasionally dysplastic, and may fuse to a coronary ostium.6 The aortic valve abnormalities usually cause no more than mild regurgitation.6
Three additional features of supravalvular aortic stenosis include: (1) the anatomy of the extramural coronary arteries; (2) the condition of the aortic leaflets and aortic sinuses; and (3) the association with Williams syndrome. Obstruction of a coronary ostium can be caused by adherence of a distorted aortic leaflet to the supravalvular stenotic ridge, by aortic medial proliferation, and by the supravalvular ridge itself, which can impede diastolic flow into an ostium.49 Because the coronary ostia are proximal to the supravalvular obstruction, the coronary arteries are exposed to elevated left ventricular systolic pressure6 and become thick-walled and dilated (see Figure 7-8). Coronary artery aneurysms have been described.50 and hypertension is a risk factor for premature atherosclerosis.6
In 1961, Williams, Barratt-Boyes, and Lowe51 described the association of supravalvular aortic stenosis with distinctive elfin facies and mental retardation. In 1962, Beuren, Apitz, and Harmjanz52 expanded the syndrome to include pulmonary artery stenosis. Williams syndrome or Williams-Beuren syndrome now includes elfin facies, mental retardation, small stature, infantile hypercalcemia, supravalvular aortic stenosis, pulmonary artery stenosis, and important vascular abnormalities, especially in adults.53,54 Renal abnormalities occur in nearly half of afflicted patients and are represented by renal artery stenosis, segmental scarring, cystic dysplasia, nephrocalcinosis, marked asymmetry in kidney size, solitary kidney, and pelvic kidney.53,55 Systemic hypertension is not necessarily related to the renovascular abnormalities56 but instead is related to stiffness of arterial walls.57 A generalized arteriopathy is characterized by medial thickening and luminal narrowing of systemic and pulmonary arteries.58 Long segment narrowing of the aorta may occur with or without localized coarctation.56 Involvement of cerebral arteries is responsible for strokes. Tortuous retinal arteries similar to those that accompany coarctation of the aorta (see Chapter 8, Figure 8-8) were described in the original report of Williams, Barratt-Boyes, and Lowe,51 and in 1985, the observation was confirmed.56
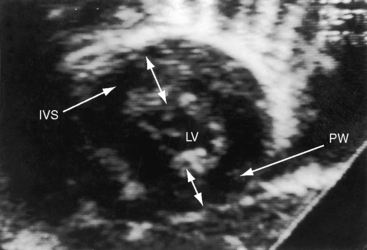
The physiologic consequences of congenital aortic valve stenosis are reflected in the response of the left ventricle to increased afterload. An adaptive increase in left ventricular mass in the immature heart is chiefly the result of hyperplasia (replication) of cardiomyocytes. In contrast, the increase in left ventricular mass in the mature heart is the result of hypertrophy (an increase in cell size) of terminally differentiated cardiomyocytes.59 The afterloaded immature heart is capable of capillary replication that is proportional to cardiomyocyte replication, so capillary density remains normal and coronary flow reserve remains normal.59,60 The increase in left ventricular mass characterized by myocyte hyperplasia with proportionate growth in the microvascular bed sets the stage for low left ventricular systolic wall stress and supernormal ejection performance.59 The left ventricle thickens concentrically and the cavity size is normal or small,59 so distensibility decreases. A greater force of left atrial contraction generates the end-diastolic fiber length necessary for left ventricular performance appropriate for the increased afterload without an increase in end-diastolic volume or left atrial mean pressure. The normal trileaflet aortic valve and its annulus increase in anatomic cross-sectional area with age even after maturity.61 The normal trileaflet physiologic orifice, which is the cross-sectional area defined by the leaflets in systole, is flow-dependent, varying directly with the volume and rate of left ventricular ejection. In the resting state, less than half the cross-sectional area of a normal trileaflet aortic valve is used during ejection, so a large reserve is available during high-flow states.
The physiologic consequences of congenital aortic stenosis take into account the morphology of the obstruction, the degree of obstruction, the age of onset, and whether or not the obstruction is progressive. A functionally normal bicuspid aortic valve awaits adulthood to become stenotic as its leaflets thicken and calcify. An stenotic aortic valve in infants and young children tends to generate an increasingly higher gradient in response to the progressive increase in transaortic flow that accompanies the normal age-related increase in body mass.62 In Williams syndrome, progressive supravalvular aortic stenosis results from inadequate growth of the sinotubular junction.63 Fixed subaortic stenosis is not present in utero but usually begins after the first year of life and undergoes a progressive decrease in cross-sectional area (see previous discussion).41,46 The time course in adults is much slower.
The subendocardium of the left ventricle in aortic stenosis is vulnerable to ischemia because of a selective decrease in perfusion.49 In neonates and infants with severe aortic stenosis, subendocardial ischemia is responsible for papillary muscle infarction with mitral regurgitation49 and for endocardial fibrosis and reduced cavity size that depress left ventricular contractility.64 A progressive rise in left ventricular filling pressure, in left atrial mean pressure, and in pulmonary arterial pressure provokes right ventricular failure.65 Supravalvular aortic stenosis incurs the additional impediment of compromised coronary perfusion (see previous discussion).
The physiologic response of the neonate to severe aortic stenosis is best understood in light of the fetal circulation. Intrauterine left ventricular volume is low because pulmonary blood flow is virtually nil. When lungs expand at birth, pulmonary blood flow commences and a severely obstructed, thick-walled left ventricle with reduced cavity size suddenly receives a sizable increment in volume. Left ventricular filling pressure rises steeply, left atrial pressure rises in parallel, and a left-to-right shunt is established across a stretched valve-incompetent foramen ovale. If a small left ventricular cavity is beset with endocardial fibrosis or fibroelastosis, the hemodynamic consequences are correspondingly worse.64 Vasoreactive pulmonary arterioles constrict, pulmonary artery pressure rises, and pressure overload is imposed on an already volume-overloaded right ventricle. Temporary patency of the ductus arteriosus diverts right ventricular blood into the aorta and delays the onset of symptoms, but when the ductus closes, that advantage is lost because the entire right ventricular output enters the pulmonary circulation and the left side of the heart.
The response to dynamic exercise mild aortic stenosis is normal, but when stenosis is severe, left ventricular stroke volume is blunted at each level of graded isotonic stress.66–68 In congenital aortic valve stenosis, the augmented flow and increased left ventricular systolic pressure induced by exercise result in a larger computed aortic valve area, which implies that the stenotic valve is sufficiently mobile to open more widely when stressed.66 Activation of canine left ventricular baroreceptors in response to an increase in left ventricular pressure or stretch induces hypotension from skeletal muscle vasodilation. Reflex vasodilation and bradycardia induced by activation of left ventricular baroreceptors during isotonic exercise are responsible for hypotension and exertional syncope.69
History
Congenital aortic valve stenosis is considerably more common in males, with a gender ratio of approximately 4:1.4,39,70 Male prevalence is less common in supravalvular aortic stenosis, depending in part on genetic transmission. Discrete and tunnel subaortic stenosis both have a distinct female prevalence.38 In the Newfoundland dog, genetically transmitted subaortic stenosis has an equal gender ratio.44
When congenital aortic stenosis is present at birth, the murmur is also present because the anatomic and physiologic conditions required to generate the murmur exist.41,46 An exception is fixed subaortic stenosis, which is not present at birth, and an additional qualification relates to specific types of congenitally malformed aortic valves.6 As a rule, the fewer the cusps and commissures, the greater the likelihood of an intrinsically stenotic valve and of a murmur in the newborn.6 Intrinsically stenotic valves are usually unicuspid unicommissural or bicuspid,6 but when a bicuspid aortic valve is functionally normal,4,6 the onset of the murmur awaits the development of fibrocalcific thickening in adulthood.1,4,6,39 Stenosis of a unicommissural aortic valve occasionally follows a protracted course similar to that of a bicuspid aortic valve.2,14
An impression of murmur intensity (loudness) can be inferred in the history with determination of how readily a murmur was heard during follow-up examinations. A loud murmur is likely to be heard even in uncooperative infants, whereas the soft murmur of mild obstruction is likely to be overlooked or mistaken for a normal murmur, even in cooperative infants and older children (see Chapter 2).
Growth and development are affected in patients with Williams syndrome (see subsequent discussion). Symptoms associated with aortic stenosis, especially in children, may be absent even in the presence of severe obstruction,39 and progression from mild to severe is not necessarily accompanied by symptomatic deterioration.71 Effort dyspnea and fatigue reflect an inadequate increment in cardiac output and an increase in left ventricular end-diastolic pressure. Effort syncope arouses suspicion of aortic stenosis in an acyanotic patient with a prominent cardiac murmur dating from infancy or childhood. Syncope depends on the degree of obstruction, not on its morphologic type,70 and is the result of reflex vasodilation and bradycardia induced by activation of left ventricular baroreceptors during isotonic exercise (see previous discussion).69 Syncope can be recurrent,39 and sudden death looms as a threat,70 although the risk in children is small compared with adults. Subtle cerebral symptoms consist of mild giddiness, faintness, or lightheadedness with effort. Syncope-induced hypotension may provoke electrical ventricular instability in adults with atherosclerotic coronary artery disease but not in young patients with aortic stenosis and normal coronary arteries.49,72
A potential disparity exists between the oxygen requirements of an hypertrophied left ventricle and coronary blood flow and flow reserve. The disparity is aggravated by acquired coronary artery disease in adults with fibrocalcific bicuspid aortic stenosis and in children with coronary artery abnormalities that accompany supravalvular aortic stenosis.73 Angina pectoris in young patients is a symptom of congenital aortic stenosis that arrests attention.
Inappropriate diaphoresis increases with the onset of congestive heart failure, especially in neonates.64,74 In infants with severe aortic stenosis, mitral regurgitation from papillary muscle infarction adds to the hemodynamic burden.72
Bicuspid aortic stenosis and subaortic stenosis are genetically transmitted (see previous discussion).44,75–77 Familial and nonfamilial types of supravalvular aortic stenosis are the basis of the following classification: (1) familial with normal facies and normal intelligence; (2) nonfamilial with normal facies and normal intelligence; and (3) nonfamilial with Williams syndrome,51,78 which results from mutation or deletion of the elastin gene located at chromosome 7q11.23.79–82 Pulmonary artery stenosis in Williams syndrome tends to improve with time, and the supravalvular aortic stenosis is progressive because of growth failure of the sinotubular junction, which may be associated with obstruction of coronary artery ostia.63 Supravalvular aortic stenosis has been experimentally produced in newborn rabbits with administration of maternal vitamin D during gestation83 and has occurred in human offspring when infantile hypercalcemia resulted from administration of vitamin D during pregnancy. The history should therefore include questions regarding maternal vitamin D ingestion.
Infective endocarditis is a potential risk in all types of congenital aortic stenosis,6,39 but the bicuspid aortic valve is especially vulnerable, whether functionally normal, stenotic, or incompetent, an observation made by William Osler84 more than a century ago. Dissecting aneurysm of the ascending aorta may dramatically interrupt the clinical course of bicuspid aortic stenosis (see Figure 7-5).85 Gastrointestinal bleeding associated with aortic stenosis, sometimes called Heyde’s syndrome, occurs in older adults.86 Angiodysplasia has been used to designate the offending lesions that tend to be present in the ascending colon but may be distributed throughout the gastrointestinal tract.86 Aortic stenosis is not thought to cause the lesions but is thought to increase the likelihood that the lesions will bleed.
Physical Appearance
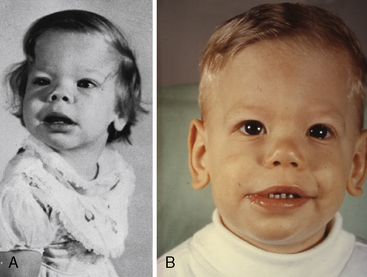
Williams syndrome (nonfamilial supravalvular aortic stenosis) is characterized by peculiar facies, short stature, and mental retardation.3,51,52 The chin is small (hypoplastic mandible), the mouth is large, the lips are patulous, the nose is blunt and upturned, the eyes are widely set with occasional internal strabismus, the cheeks are baggy (Figure 7-9), the teeth are malformed, and the bite is abnormal (malocclusion; Figure 7-10). Flat molar regions accentuate the prominence of a wide mouth with full lips, small jaw, and long philtrum.54 The brow is broad with prominent supraorbital ridges. The nasal tip is broad, and the nacres are anteverted. Adults with Williams syndrome are relatively short and tend to have lordosis, kyphoscoliosis, and joint abnormalities of the lower limbs that result in a stiff awkward gait.54 Friendly temperaments and deep, somewhat metallic voices further emphasize the similarities. XO Turner’s syndrome (see Chapter 8) represents another distinctive physical appearance that coexists with a bicuspid aortic valve.87 Congenital heart disease with Turner’s syndrome has been known since the initial description by Morgagni, and is coupled with different patterns of X monosomies.88 Abnormal karyotypes consist of 45 X mosaicism and X structural abnormalities.89 Patients with severe dysmorphic features have a significantly higher prevalence rate of congenital heart disease,89 and patients with 45 X Turner’s syndrome have the highest prevalence rate.89 X structural abnormalities are associated with an increased prevalence rate of bicuspid aortic valve,89 but with X deletion, the incidence rate of congenital heart disease is not increased.88 In Noonan’s syndrome (Turner’s phenotype with normal genotype), obstruction to left ventricular outflow is the result of hypertrophic obstructive cardiomyopathy (Figure 7-11).
Arterial Pulse
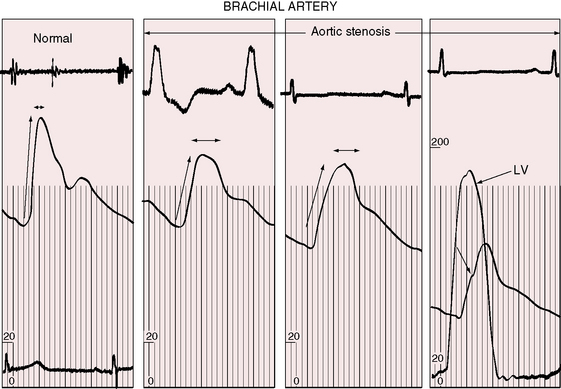
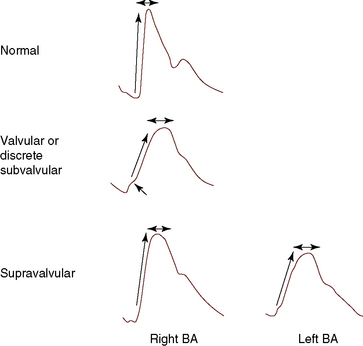
The object of the following paragraphs is to consider the aid in the diagnosis of aortic stenosis that may be supplied by a study of the pulse (Graham Steell, The Lancet, November 1894). Fixed obstruction to left ventricular outflow distinctively alters the arterial pulse.3,90 The pulse pressure is small, the rate of rise is slow, the peak is sustained, and the decline is gentle (Figures 7-12 and 7-13). This typical configuration is not as frequent in children as in adults with equivalent aortic stenosis.90,91 Children with severe obstruction may have a brachial arterial pulse that is interpreted as normal, although palpation of the carotid artery improves accuracy.91,92 A bisferiens pulse (twin peaked) implies coexisting aortic regurgitation.90
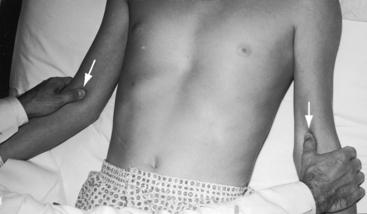
The right and left brachial and carotid arterial pulses are symmetric in valvular or fixed subvalvular aortic stenosis, but in supravalvular aortic stenosis, the rate of rise, the systolic pressure, and the pulse pressure are greater in the right brachial artery and in the right carotid artery (see Figure 7-13)93,94 because the hourglass deformity directs the high-velocity jet toward the right wall of the aorta and the Coanda effect (affinity of a jet stream for adherence to a wall) carries the jet into the innominate artery.93–95 Experimental observations with an aortic arch model showed that kinetic energy developed in a jet stream under conditions simulating supravalvular aortic stenosis is sufficient to account for the clinically observed differences in arterial pressure.93 Selective narrowing of the origins of the left carotid and left subclavian arteries (see Figure 7-8B) is an uncommon cause of asymmetric pulses.95 In healthy adults, the systolic pressure in the right arm is 10 to 15 mm Hg higher than in the left arm.90 Simultaneous determination of blood pressure in both arms minimizes these differences, and the technique of palpation shown in Figure 7-14 is useful in the clinical comparison of the right and left brachial pulses.3,90
In valvular and fixed subaortic aortic stenosis, arterial thrills or shudders are common in the suprasternal notch and over the carotid and subclavian arteries.3,90,92 In supravalvular aortic stenosis, the thrill is distinctly more pronounced over the right carotid artery, which exhibits an increased pulsation.
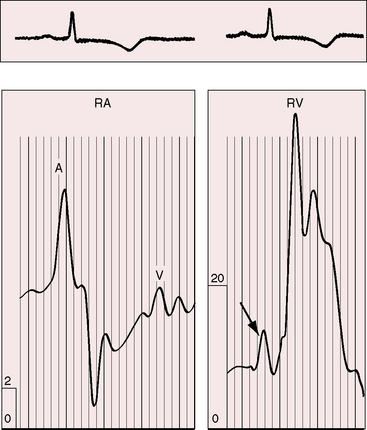
Jugular Venous Pulse
Directing attention to the amplitude of the jugular venous A wave in subjects with isolated obstruction to left ventricular outflow is seemingly paradoxical.3,90 However, left ventricular hypertrophy serves to decrease right ventricular distensibility, so the right atrium contracts with greater force and the amplitude of the jugular venous A wave increases in the absence of pulmonary hypertension (Figure 7-15).3,90,96
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree