Chapter 29 Congenital Anomalies of Vena Caval Connection
Anomalous vena caval connections comprise a wide range of malformations that vary from minor to major and that occur in isolation or with coexisting congenital heart disease. Persistent left superior vena cava occurs in 0.3% of the general population and in 4.3% of congenital heart disease.1 A left-sided inferior vena cava occurs in 0.2% to 0.5% of the general population.1 This chapter focuses on isolated anomalous vena caval connections in situs solitus hearts (Table 29-1). Anomalies of vena caval connection with cardiac malpositions or with atrial isomerism are dealt with in Chapter 3.
Table 29-1 Congenital Anomalies of Vena Caval Connection
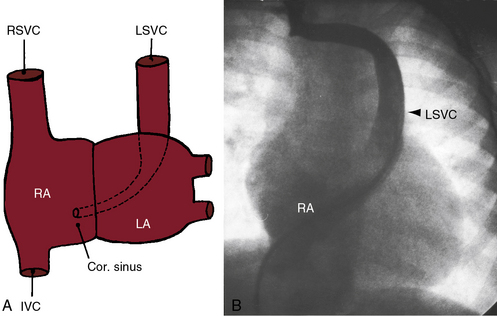
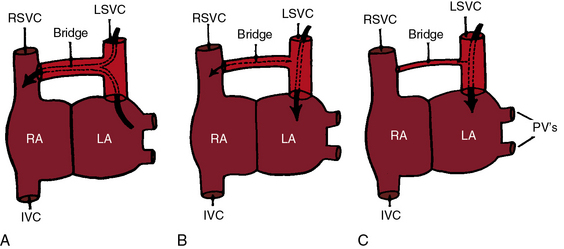
In early embryonic development, the common cardinal veins are bilaterally symmetric and are potentially responsible for bilateral superior vena cavae.2 The left common cardinal vein initially drains into the left portion of the sinus venosus, which becomes the coronary sinus.2 Failure of obliteration of the left common cardinal vein results in persistent connection of a left superior vena cava to the coronary sinus (Figure 29-1),2 a relatively common anomaly estimated at 0.3% to 0.5% of the general population and 1.5% to 10% of patients with congenital heart disease.3 An isolated left superior vena cava in itself produces no physiologic derangements when it drains harmlessly into the right atrium via the coronary sinus (see Figure 29-1). However, the coronary sinus dilates sometimes appreciably,4 especially if there is atresia of its right atrial orifice5 or absence of the right superior vena vava.6,7 When the right superior cava is absent, the sinus node pacemaker is absent because the pacemaker is normally located at the junction of the right superior vena cava and the morphologic right atrium.8–11 A persistent left superior vena cava is a significant anomaly when it connects to the left atrium (Figures 29-2 and 29-3).12–14 The coronary sinus is usually absent15 with partial or complete unroofing of its anterosuperior wall. Unroofing results in a connection between the left atrium and the right atrium—a coronary sinus type of atrial septal defect (see Chapter 15).16 A right-to-left shunt coexists through the left superior vena caval to left atrial connection.14,17 An absent coronary sinus with bilateral superior vena cavae (right superior cava connected to the right atrium, left superior cava connected to the left atrium) is thought to represent a developmental complex.18 If the right superior vena cava is absent or atretic (see Figure 29-3), the innominate vein crosses the midline and terminates in the left superior vena cava.19 The left atrium occasionally receives the azygos vein, the hepatic vein, or the coronary sinus,14 variations that are not considered in this chapter.
Direct connections between vena cavae and left atrium are uncommon.7,20,21 Rarely, a right superior vena cava connects to the left atrium.22–24 Still more rarely, a right superior vena cava connects to the left atrium, and a left superior vena cava connects to the right atrium.25 Connection of a right superior vena cava to the left atrium must be distinguished from drainage of a right superior vena cava into both atria caused by a contiguous superior vena caval sinus venosus atrial septal defect (see Chapter 15).20 When a right superior vena cava is congenitally absent (see Figure 29-3), brachiocephalic veins join a left superior vena cava that connects to the coronary sinus.6,26
Bilateral superior vena cavae3 are illustrated in Figure 29-2. The innominate bridge that connects the two superior cavae may be widely patent, narrow, or atretic (see Figure 29-2), and the size of the left superior vena cava ranges from large to rudimentary.3 Bilateral superior vena cavae with atrial isomerism are dealt with in Chapter 3.
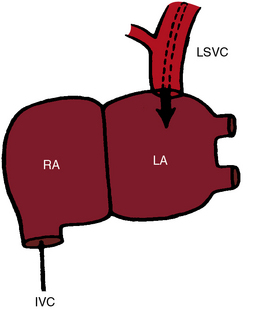
Anomalous connection of the inferior vena cava to the left atrium consists of a morphogenetic spectrum represented by combinations of persistence of the valve of the right sinus venosus, fusion of the valve with the septum secundum, and incomplete development of the atrial septum.27 The inferior vena cava penetrates the diaphragm at its expected site. An enlarged azygos vein may arise from the anomalous inferior cava and convey inferior caval blood into the right atrium (Figure 29-4).21,28,29 An isolated left-sided abdominal inferior vena cava usually crosses to the right after receiving the renal veins, then penetrates the diaphragm and enters the right atrium at the normal site. A distinction must be made between connection of the inferior vena cava to the left atrium and anomalous inferior vena caval drainage into the left atrium from persistence of a large Eustachian valve (right valve of the sinus venosus) that directs flow toward a patent foramen ovale or across an ostium secundum atrial septal defect (see Chapter 15).27
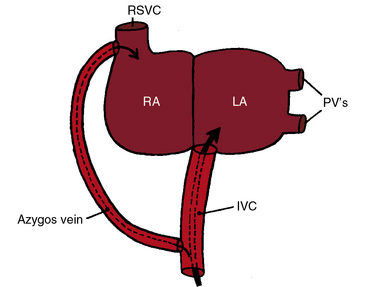
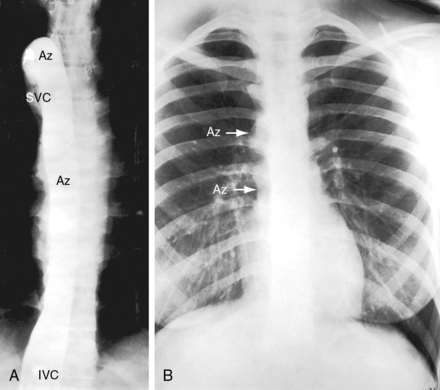
Inferior vena caval interruption with azygous continuation is rare as an isolated malformation and is of no physiologic significance but can be mistaken for the descending thoracic aorta (Figure 29-5).30 Interruption is immediately proximal to the renal veins and continues into a dilated azygos vein that enters the thorax to the right of the aorta, runs in the posterior mediastinum, and connects to a right superior vena cava (see Figure 29-5). There is an association with congenital absence of the portal vein.31 Inferior vena caval interruption with azygos continuation and left isomerism are dealt with in Chapter 3.
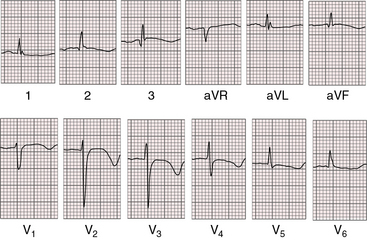
Anomalous connection of either vena cava to the left atrium is rare enough, but connection of the right superior vena cava and the inferior vena cava to the left atrium—total anomalous systemic venous connection—is even rarer (Figures 29-6 and 29-7). 7,20,32 Survival depends on adequate mixing through an interatrial communication.
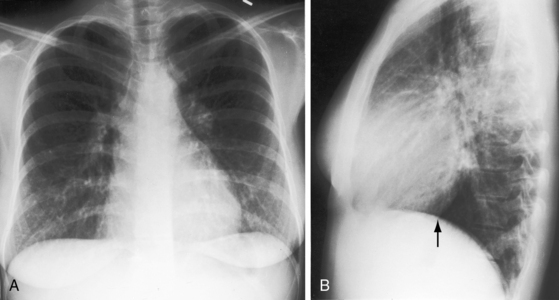
Figure 29-7 X-rays from the 28-year-old woman with total anomalous systemic venous connection whose electrocardiogram is shown in Figure 29-6. A, The size and configuration of the heart are normal. Pulmonary vascularity is not reduced. Increased markings in the left lower lung fields are superimposed breast tissue. B, In the lateral projection, the inferior vena caval shadow is absent (arrow).
The physiologic consequences of anomalous vena caval connections to the left atrium take into account two variables: (1), the direction and volume of blood flow through the connection; and (2), the effect of the connection on the amount of blood flow entering the right and left sides of the heart. Flow patterns are complex when a persistent left superior vena cava communicates with the left atrium (see Figure 29-2).14,17 The left superior vena cava may be the only superior cava (see Figure 29-3), or bilateral superior cavae may fail to communicate with each other because of stenosis or atresia of the innominate bridge (see Figures 29-2B and C). All or nearly all of left superior vena caval blood is then channeled into the left atrium (Figure 29-2B and C), so cyanosis is obligatory. Alternatively, when bilateral superior vena cavae communicate freely through a nonrestrictive innominate bridge, the direction of blood flow is from the left atrium into the anomalous left superior vena cava, across the innominate bridge and into the right superior vena cava (Figure 29-2A).17,33 The pathway constitutes a left-to-right shunt, so cyanosis is absent.14 With this exception, communications between vena cavae and left atrium result in right-to-left shunts and in a decrease in systemic arterial oxygen saturation. When a right superior vena cava connects to the left atrium, caval blood flow is into the left atrium, so cyanosis is inevitable. When the inferior vena cava connects to the left atrium, unoxygenated blood is directed into the left atrium despite a large azygos vein, so cyanosis is obligatory (see Figure 29-4).
Now consider the relative volume of blood flowing through the two sides of the heart in the presence of vena caval–to–left atrial connections. Normally, the entire systemic venous return from the superior and inferior vena cavae enters the right side of the heart, and the entire pulmonary venous return from the pulmonary veins enters the left side of the heart. If one vena cava connects to the left atrium, the right side of the heart is effectively bypassed, so right ventricular output and pulmonary blood flow fall reciprocally.34 Left ventricular output theoretically remains unchanged because the increment in anomalous caval flow into the left atrium is matched by the reciprocal decrement in pulmonary venous flow. Accordingly, as systemic venous return to the left atrium increases, pulmonary venous return to the left atrium decreases by the same amount, so total blood flow to the left side of the heart remains unchanged. In the absence of compensatory mechanisms, anomalous caval connections to the left atrium should be associated with reduced pulmonary flow and normal systemic flow,34 patterns that should pertain irrespective of whether the superior or inferior vena cava connects anomalously. Do these circulatory patterns really exist? Clinical and experimental observations indicate that right atrial and right ventricular pressures are normal or low34 and pulmonary blood flow is usually,34 but not always, reduced. Necropsy descriptions of a small right atrium and a small right ventricle are relevant.35 However, left ventricular output tends to be moderately increased.34 The mechanisms responsible for these deviations from theoretical blood flow patterns are not known.
When the superior vena cava and inferior vena cava both connect to the left atrium (total anomalous systemic venous connection), flow patterns are modified by obligatory mixing at atrial level. The left atrium receives blood from both cavae and from the pulmonary veins. Part of this mixture reaches the left ventricle directly across the mitral valve, and the remainder enters the right side of the heart across an atrial septal defect. Pulmonary blood flow is not increased even in the presence of a nonrestrictive atrial septal defect and normal pulmonary vascular resistance (see Figure 29-7).
History
Isolated anomalous vena caval connection to the left atrium has an equal gender distribution. Cyanosis dates from birth or infancy20,27 unless bilateral superior cavae are connected by a nonrestrictive innominate bridge (see Figure 29-2A). Despite conspicuous cyanosis, there is a paucity of symptoms.21,27 the syndrome of cyanosis and clubbing with normal heart. Adult survival is expected, with longevities recorded in the sixth, seventh, and eighth decades.12,20 Effort intolerance, dyspnea, and light-headedness develop late if at all and are generally mild.20,21 One man tolerated training in the armed forces.27 Brain abscess and paradoxical embolus have been reported.20,23
The cause of death is usually unrelated to the isolated congenital anomalies of vena caval connection. However, unexplained sudden death has been reported with isolated left superior vena caval connection to the coronary sinus, especially if the right superior vena cava is absent.9