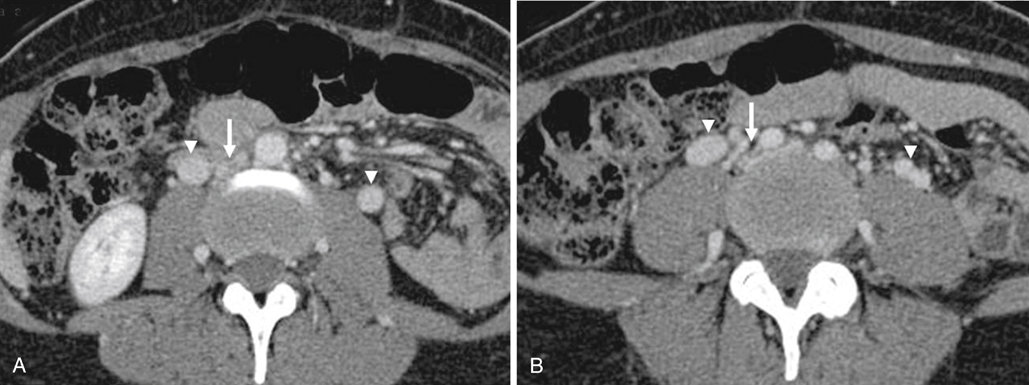
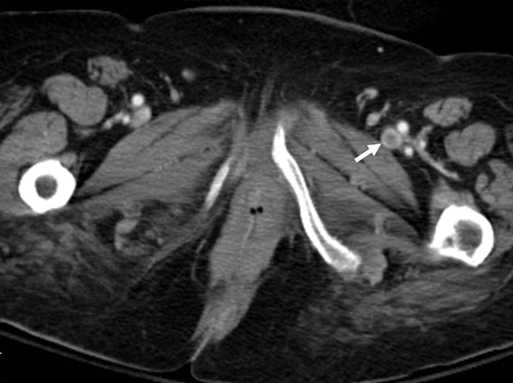
Although indirect CTV is less technically challenging to perform, the contrast bolus is essentially diluted by the patient’s entire blood volume. This necessitates administration of a higher volume of contrast (often 200 mL in our practice) and nevertheless results in an 11% rate of nondiagnostic studies. However, the technique still can be quite powerful and does show adjacent visceral anatomy as well (Figure 1). One potential advantage of CTV is that it can be combined with CT pulmonary angiography to provide a single examination (Figure 2) for pulmonary embolus (PE) and deep vein thrombosis (DVT). This is accomplished by imaging the pelvis and thighs 2 to 4 minutes after injection of the contrast bolus for pulmonary CT angiography (CTA), allowing venous recirculation and opacification of lower extremity veins. This has the advantage of rapid acquisition and use of a single contrast bolus.
Computed Tomographic Venography and Magnetic Resonance Venography
Computed Tomography Venography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


