Complications of Diagnostic and Therapeutic Endovascular Procedures
Paul G. Bove
Graham W. Long
As with open vascular surgical procedures, the potential exists for life- and limb-threatening complications with endovascular procedures. Certain complications are unique to endovascular procedures. In this chapter, general mechanisms of morbidity that are potentially experienced during any endovascular procedure will be presented; recommendations on how they may be prevented will also be discussed. Complications associated with specific types of endovascular reconstructions will be discussed in detail in other sections of this text.
General Principles
There are basic tenets to the performance of endovascular procedures, which can help limit, control, and recognize complications when they occur.
A complete understanding of the patient’s medical history is necessary. Knowledge of medical comorbidities, such as preexisting renal disease, diabetes mellitus, contrast allergy, asthma, connective tissue disorder, and coagulopathy, as well as prior vascular procedures, is essential to delivering safe care. In addition, a full vascular examination should be documented. This is true for all procedures—from a simple diagnostic examination to a complex, combined open and endovascular procedure. Many of these components of the medical history can dictate the approach to the patient with respect to contrast selection and volume used, need for periprocedural hydration, and access strategy.
Basic principles such as vigilant fluoroscopic guidance during guidewire and catheter manipulation can prevent or limit complications such as arterial dissection, vessel perforation, and organ injury. This may appear obvious, but if the practitioner is not accustomed to gentle guidewire manipulation and tactile feedback during guidewire and catheter passage, iatrogenic perforation or dissection may occur, and it is a potentially life- or limb-threatening complication.
The technologic advances in catheter and wire construction allow the proper selection of tools for specific indications. Guidewires are designed with specific lengths of flexible tips to allow atraumatic passage through a vascular bed but to maintain enough columnar strength to act as a platform for other coaxial maneuvers. Catheters are preformed in specific shapes to aid in gentle manipulation to access desired target vessels. The practitioner should have access to a wide variety of these devices to maximize the likelihood of a successful procedure with a low risk of complications. Image quality is another essential component to limit complications. Imaging technology has advanced to the point that the practitioner should insist on a superb imaging unit for the performance of endovascular procedures. Proper imaging not only allows the physician to better perform the desired task but also to identify complications should they occur. To enhance the precision of each targeted endovascular procedure, care should be taken to optimize imaging angles to better define anatomy. Radiographic adjuncts, such as digital subtraction angiography and roadmapping, can greatly improve diagnostic accuracy and therapeutic precision. Such imaging is required for procedures ranging from accurate angioplasty and stent placement, to endoluminal stent graft placement in the immediate infrarenal location, to detecting and treating endoleaks. Adequate power is necessary to allow radiographic penetration of the morbidly obese patient. Adequate field of view is necessary to allow comprehensive assessment of anatomy. The practitioner with the same political vigor as is used by other disciplines should insist upon state-of-the-art equipment.
Access Site Complications
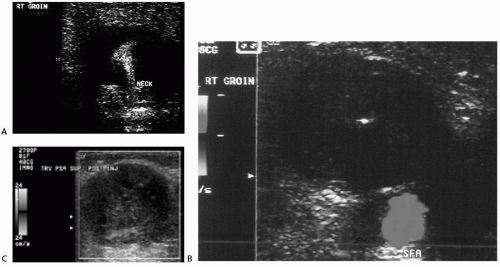
Following the decision to perform an endovascular procedure for either diagnostic or therapeutic benefit, the decision must be made about access location. Central to this decision are the complications that can arise from the proposed access site. The incidence of access site complications varies from 1% to 10%. Types of complications include chronic pain, hematoma, pseudoaneurysm, arteriovenous fistula, and vessel thrombosis. All vascular punctures result in some vessel injury. The very mechanism of hemostasis with the formation of a platelet plug is a result of vascular injury. In the venous bed this may result in venous thrombosis, just as it can in an access artery. The formation of the platelet plug combined with overzealous manual compression, intimal dissection, or challenged outflow can ultimately contribute to vessel thrombosis. Clinically evident hematoma occurs in 2% to 8% of patients, while pseudoaneurysm formation occurs less than 2% of the time (Fig. 59-1A-C). Arteriovenous fistulae are less common, occurring in less than 0.5% of patients. Large
sheath size, access vessel location, access vessel intrinsic disease, and extrinsic scarring, coagulopathy, and hypertension are the most common factors that contribute to hemorrhagic complications of access. Access sites involving the axillobrachial arterial tree are more likely than femoral access sites to develop postprocedural hemorrhage. In addition, bleeding in the former location can cause nerve sheath hematomas, resulting in permanent neurologic impairment in the involved extremity.
sheath size, access vessel location, access vessel intrinsic disease, and extrinsic scarring, coagulopathy, and hypertension are the most common factors that contribute to hemorrhagic complications of access. Access sites involving the axillobrachial arterial tree are more likely than femoral access sites to develop postprocedural hemorrhage. In addition, bleeding in the former location can cause nerve sheath hematomas, resulting in permanent neurologic impairment in the involved extremity.
There are many adjuncts that can be employed to decrease access site complications. For palpation-directed arterial puncture to be successful, the pulse should be easily palpable. A complete vascular examination should be performed prior to choosing the access site. Pulses should be compared from one side versus the other; consideration should be given to using the more prominent pulse. Factors such as obesity and prior vascular access or surgical intervention increase the complexity of percutaneous access at that site. Adjuncts to consider in these situations include ultrasound guidance of the vessel to be punctured; palpation of the inguinal ligament, rather than the groin crease, in localizing an appropriate puncture site; and fluoroscopic imaging of anatomic landmarks, such as the femoral head. In more complex cases, accessing a remote location and using digital subtraction angiography to visualize and roadmap a potential primary access vessel are appropriate. For example, in the case of an occluded common iliac artery, the contralateral femoral or brachial approach can be accessed to perform a distal aortogram with delayed imaging of the target femoral vessel. This roadmapping can then be used as a guide to ipsilateral access. The use of micropuncture sets can also facilitate difficult access cases.
In an attempt to limit hemorrhagic complications of arterial access and shorten immobilization times, various closure devices have been developed. These may be suture mediated or may involve placement of topical hemostatic devices at the arterial puncture site. There are no high-level data regarding the use of these devices. The most common complication of their use is failure of the device with resultant hematoma, pseudoaneurysm, or arteriovenous fistula. Malfunction or failure of closure devices can result in the need for immediate open surgical repair and removal of the device. A more significant complication reported anecdotally involves development of an infectious arteritis secondary to suture-mediated closure devices, which requires arterial resection, vascular reconstruction, and often muscle flap coverage. Most compiled data demonstrate no advantage in reduction of complications but show a shorter time to hemostasis with the possible increased risk of complications related to the presence of a foreign body.
Contrast-related Complications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree