Presentation
Hypotonic infant
Delayed psychomotor development
Swallowing disorder
Gait alteration, frequent falls
Central neurological symptoms: epileptic seizures
Lack of strength, fatigability
Muscular pain, cramps
Orthopedic alterations: clubfoot, equinus foot, pes cavus, scoliosis
Recurrent pneumonia, recurrent or persistent atelectasis with no clear respiratory cause
Sleep disturbances, snoring, obstructive and central apneas
Pathophysiology and clinical signs in neurological disease
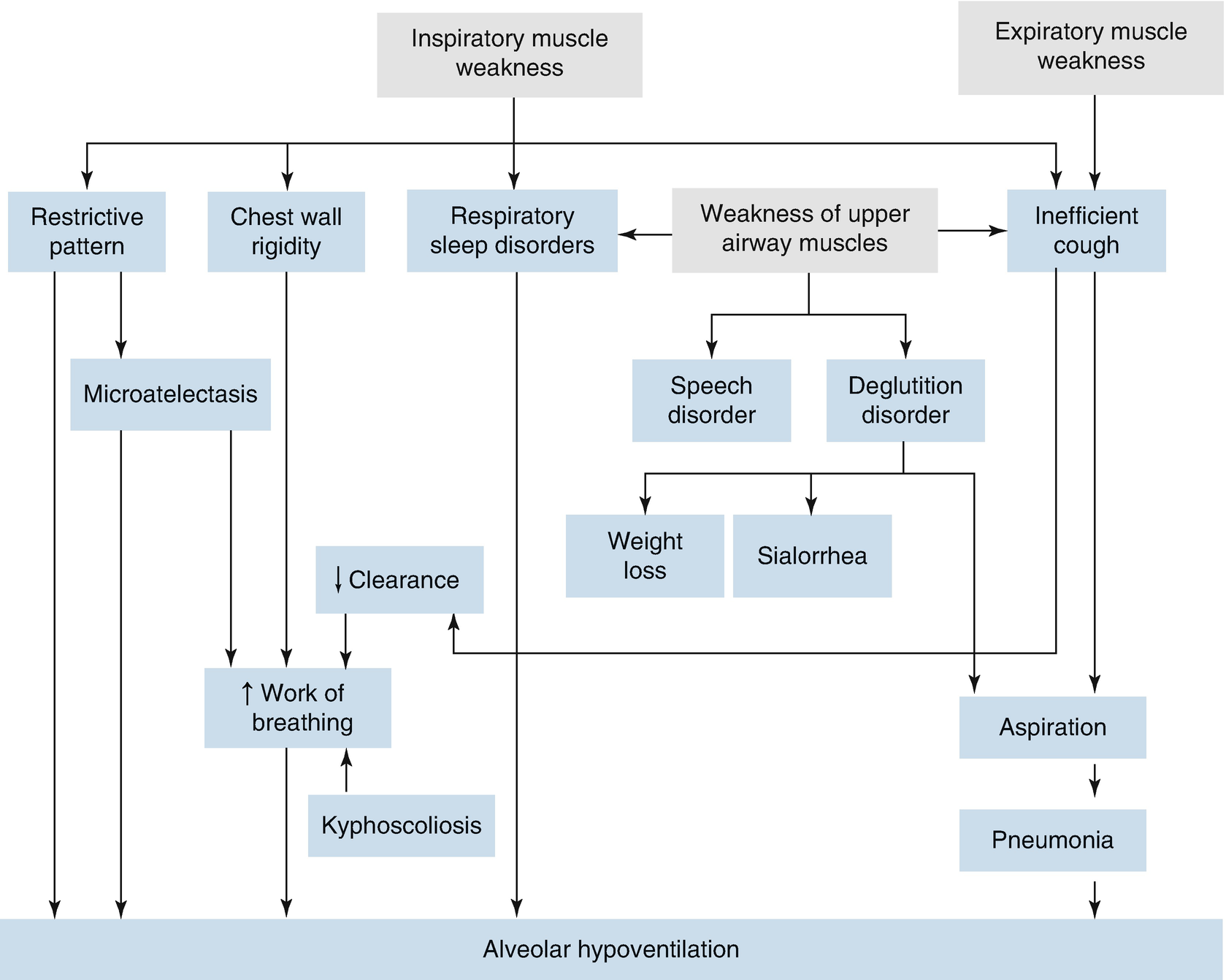
The respiratory clinical picture depends on the severity and timing of respiratory muscular compromise. For example, in patients with SMA type 1, who have an early and severe presentation, the infant’s chest is bell shaped, with tachypnea and paradoxical breathing, in a context of generalized hypotonia. With diseases that progress more slowly, such as DMD, the respiratory symptoms are insidious and often go unnoticed, such as sleep alterations due to nocturnal hypoventilation, resulting in hypoxia and sleep fragmentation, in turn leading to neurocognitive and behavioral problems, hyperactivity or lethargy, morning headaches, and anorexia.
Symptoms and signs of alterations of the respiratory system in neurological disease
System | Symptoms and signs |
|---|---|
Constitutional | Fatigue Weakness Retarded growth |
Cardiopulmonary | Cyanosis Tachycardia Dyspnea Tachypnea Diaphragmatic paradox Use of accessory muscles Decreased diaphragmatic excursion Bell-shaped thorax Weak cough Recurrent or persistent atelectasis Recurrent pneumonia |
Central nervous | Morning headache Hypersomnolence Neurocognitive alterations Hyperactivity Speech disorder |
Sleep | Restless sleep Nightmares Nocturnal enuresis Frequent awakenings Snoring Apneas |
Others | Blockages Sialorrhea Speech disorder |
Diagnostic Foci
A complete initial assessment that includes the medical history is needed, besides a complete physical examination that seeks the signs and symptoms described above, with evaluation by specialists in the relevant fields.
Neurological Focus
To determine the prognosis, it is necessary to have a topographical neurological diagnosis that identifies the level of compromise of the nervous system. A complete neurological examination is essential, which includes nuclear magnetic resonance (NMR) imaging of the brain and/or bone marrow; neurophysiological studies such electroencephalography, evoked potentials, muscle enzyme levels, electromyography, and peripheral nerve conduction velocity; muscular imaging studies; muscle and/or nerve biopsies; and specific molecular and genetic studies.
Respiratory Focus
Evaluation of Sleep Alterations
Peripheral oxygen saturation: The peripheral oxygen saturation (SpO2) can be assessed continuously during sleep to determine the base and average levels, besides the levels during desaturation events or clusters in relation to snoring or sleep stages in particular. More sophisticated and sensitive equipment has been developed in recent years, using signal purification techniques that better show periods of desaturation, although this test does not adequately identify respiratory sleep disorders (RSDs) in this type of patient.
Capnography: Expirated or transcutaneous carbon dioxide levels can be measured. This parameter indicates alveolar ventilation. This measurement is more useful as a complement to sleep study than in isolation.
Gases in arterial blood: The partial pressure of carbon dioxide (PaCO2) shows the severity of hypoventilation, while the pH, bicarbonate, and base excess indicate the repercussions in terms of the acid–base balance and the degree of metabolic correction, adding specificity to the diagnosis. Studies by Hukins (2000) and Mellies (2003) showed that PaCO2 values above 40 mmHg and 45 mmHg, respectively, correlated with nocturnal hypoventilation, with sensitivity of more than 90% and specificity of around 75%.
Polysomnography: Polysomnography studies play an important role in early detection of RSDs among patients with neurological diseases, including in the absence of significant clinical manifestations and in the absence of examinations of pulmonary function in normal wakefulness. Active (REM) sleep inhibits muscular activity, and slow-wave non-REM (NREM) sleep impedes nonchemical afferences to the respiratory center, increasing the risk of nocturnal hypoventilation, obstruction of the upper airway, and apnea. Polygraph testing, which is derived from polysomnography, uses other criteria besides electroencephalographic waves to determine sleep stages. The polygraph has the advantage of being portable, and this type of test is relatively inexpensive. Respiratory alterations during sleep should be assessed at least once a year in patients presenting any of the following criteria: VC <60% of the predicted value, loss of mobility, symptoms or signs of obstructive apnea–hypoventilation, and diaphragmatic weakness (level of recommendation: D). If rapid worsening, repeated infections, or sleep alteration symptoms occur, the studies should be repeated with the necessary frequency for early diagnosis and intervention.
Assessment of Pulmonary Force and Function
Spirometry: There is a characteristically restrictive pattern (reduced forced vital capacity (FVC) and reduced forced expiratory volume in 1 second (FEV1)). The flow curve is useful to show a reduction in force-dependent respiratory flows: the maximum inspiratory flow (MIF) and maximum expiratory flow (MEF). VC should be measured as part of lung function studies in all patients diagnosed with NMDs who can perform this maneuver (level of recommendation: C).
Muscular strength assessment: Decreases in muscular strength and resistance in the context of fatigue are the first clinical elements that present in NMDs. The assessment includes measurement of the maximum voluntary ventilation (MVV), maximum inspiratory pressure (MaxIP), and maximum expiratory pressure (MaxEP), and it is more sensitive than VC measurement at the initial stages of the disease. MaxIP is the maximum pressure generated during inspiration with the airway occluded and is based on the residual volume or the functional reserve capacity. MaxEP is the maximum pressure generated during expiration with the airway occluded and is based on the total lung capacity. The effort should be maintained for 1 second, and at least five maneuvers of each type should be done until at least two reproducible results are obtained. A MaxIP value of >80 cm H2O is of great value in excluding muscular compromise of clinical importance. A 75% decrease in the MaxIP value or a predicted value close to 30% is needed to observe a significant decrease in FVC. Thus, spirometry and the volume/time relationship are not very sensitive tests to evaluate muscular failure at the initial stages.
Maximum flow with cough: This is a tool to assess the effectiveness of coughing and can be measured using a mask or mouthpiece. There is evidence in adults that a minimum of 160 l/min is necessary to adequately mobilize secretions, and that values above 270 l/min represent respiratory indemnity (level of evidence: 3). Although no specific values have been established in children, this test is recommended for respiratory evaluation in subjects over 12 years of age.
Evaluation of Complications
Imaging studies: A chest x-ray determines the presence of associated pneumonia or atelectasis. Radioscopy and echoscopy assess diaphragmatic mobility.
The chest of a patient with NMDs is bell shaped when there is thoracic muscle involvement. The esophagus–stomach–duodenum (ESD) transit, assessed with a specific videodilution study, evaluates the presence of gastroesophageal reflux (GER) and deglutition disorders as causes of pulmonary aspiration, recurrent pneumonia, or chronic interstitial lung compromise.
Assessment of the airway: Suspicion of bulbar or pharyngeal and suprahyoid musculature compromise makes it necessary to evaluate the airway. Fiber bronchoscopy is useful to diagnose hypotonic or pharyngeal incoordination and vocal cord paralysis or paresis, which is related to a potentially unstable airway. In patients with a tracheostomy, it is useful to anatomically evaluate the intervened airway. In the case of persistent atelectasis, fiber bronchoscopy can indicate appropriate therapy.
Cardiological Focus
Patients with neurological disease can have primary or secondary compromise of the cardiovascular system. Primary myocardial involvement must be ruled out in myopathies such as DMD or Becker disease, some congenital myopathies, mitochondrial diseases, and other conditions, as determined by a specialist in NMDs. Cardiovascular compromise is secondary to muscle-based diseases or to the development of pulmonary hypertension due to chronic hypoxemia, which at the advanced stage constitutes pulmonary heart disease. Hyperpulmonary flow, due to increased transpulmonary pressures, is also a cause of pulmonary hypertension, as occurs in patients with obstructive sleep apnea. Other alterations of the airway, such as heart rhythm disorders, should be evaluated in patients with central hypoventilation syndromes and patients with specific NMDs, such as Emery–Dreyfus syndrome or certain congenital myopathies.
Treatment
In neurological diseases, respiratory failure accounts for most acute and chronic morbidity, as well as mortality. Until curative therapies are available for the underlying neurological disease, efforts must be made to slow the progressive deterioration of musculoskeletal and respiratory function, thus improving the quality of life. The treatment is multidisciplinary, including respiratory medicine, neurology, nutrition, kinesiology, gastroenterology, orthopedics, and other specialties.
Nutrition
Patients with neurological diseases often suffer from malnutrition , due to both deficiency and excess. Situations of malnutrition occur more in a context of low nutritional intake (due to difficulty in swallowing) or greater energy expenditure (due to excessive respiratory work). Excesses occur in a context of assured nutrition, without consideration of the fact that the patients have lower basal energy expenditure, so their requirements are also lower.
Malnutrition affects the functioning of the respiratory musculature, and at the same time it facilitates recurrent infections. Thus, when diagnosed, the patient must be supported until an acceptable nutritional status is reached, which varies from one person to another. Slow growth is common, so it is advisable to adapt the height/weight ratio to limit the diet in order to avoid overfeeding. Enteral feeding via a nasogastric tube or gastrostomy is usually necessary. It is also useful to consider specific nutritional gaps—in particular, those related to bone metabolism—because of a higher risk of multicausal osteopenia and related fractures.
Respiratory Kinesiotherapy
The main objectives of respiratory kinesiotherapy are to prevent and treat atelectasis, permeabilize the airway, and assist respiratory rehabilitation. Multiple maneuvers of successive inspirations and forced expirations with assisted coughing add to the workload and to respiratory muscle fatigue in children with ventilatory insufficiency, so this therapy should be conducted with caution.
There are now cough assist devices that can be used in patients with neurological disease. These devices are applied through interfaces such as masks, mouthpieces, and tracheostomies as part of the management of respiratory exacerbations, minimizing the risk of intubation and providing mechanical cough assistance for stable patients who are too weak to cough.
Respiratory muscle training with adjustable valves has allowed the development of training plans for adult patients with chronic obstructive pulmonary disease. These have begun to be applied to children, with positive results, although long-term research will be needed, especially considering that the muscles of patients with NMDs are diseased and their training capacity does not necessarily follow the same principles that apply to healthy muscles.
Scoliosis
The rapid progression of scoliosis in patients with neurological diseases is directly related to the progression of the disease and to the sitting postures that patients maintain, which do not always preserve correct alignment, making the gravitational effect on the curvature of their spine accelerate the progression of the kyphoscoliosis. Respiratory complications are an indication for treatment with arthrodesis, because systems for support and maintenance with corsets in these cases have not been shown to be useful, while hindering respiratory mechanics. Surgery should be deferred for as long as possible; however, the presence of a Cobb angle of >40° correlates with respiratory failure.
Neurorehabilitation
Neurorehabilitation aims to improve the general functioning of the patient in relation to the activities that correspond to their age. Two types of interventions are generally carried out: one involves techniques to stimulate the generation or restoration of central or peripheral motor circuits to improve motor functionality, while the other employs external support for neuromuscular functioning—for example, padding to keep the head erect, chairs adapted for sitting requirements, a tilting table to put patients without control over head movement in a standing position, or a prone-position table for patients with partial control over their heads.
Standing systems are based on the extensive published evidence of the benefits of patients being in a standing position in several respects: it improves gastric and urinary emptying, and it strengthens ossification, according to studies in quadriplegic patients, who stand for an hour five times a week. This evidence can be extrapolated to patients with more serious NMDs, who commonly experience fractures of long bones as a result of low-impact trauma associated with movement and postural changes.
Evaluation and management of swallowing are essential to avoid pulmonary complications. Although oral feeding is not an objective, techniques of desensitization and intra- and perioral management are essential for development of reflexes. Establishment of motor sequences and muscle strengthening through speech therapy intervention techniques must also be considered early on. Swallowing rehabilitation is aimed at maintaining and/or recovering suction–swallowing mechanisms.
Pharmacological Treatment
The use of steroids is indicated in patients with DMD; prednisone and deflazacort have been shown to be effective in increasing force and delaying loss of force, prolonging autonomy for around 2 years. The increase in strength, and especially the increase in the time spent walking, has a direct effect on the ventilatory capacity of affected children, although side effects must be monitored. Recent studies have shown that treatment with lower doses of corticosteroids in nondaily regimens has the same beneficial effects as daily use of prednisone, but without the traditional side effects. However, once the ability to walk is lost, this therapy merely increases potential adverse effects such as osteoporosis.
Creatine is a dietary supplement that has been shown to improve strength in both healthy individuals and carriers of disabling diseases. The beneficial effect is due to increased muscle protein synthesis—in particular, heavy chain myosin—and to increased intramuscular glycogen. However, it should be kept in mind that this effect is beneficial only when it supplements creatine associated with strength training and antiresistance techniques. Carnitine may be useful in patients with myopathies secondary to metabolic syndromes with carnitine deficiency.
Assisted Ventilation
Publications on the impact of noninvasive assisted ventilation—especially in relation to NMDs and thoracic deformities such as kyphoscoliosis—recommend its use in investigation of nocturnal hypoventilation, a condition associated with disorders of pulmonary function and blood gases during wakefulness.
Thus, investigation of nocturnal hypoventilation and RSDs, involving sleep and pulmonary function studies, makes it possible to decide whether or not to employ noninvasive ventilatory assistance.
Long-term follow-up of this type of assistance has shown improvements in the quality of life, RSDs, nocturnal hypoventilation, and daytime hypercapnia, with decreased health care costs. It has also been recently verified that the frequency and severity of respiratory infections are reduced, with a decreased incidence of hospitalizations for complications of infections.
Oxygen Therapy
The cardinal disorder in NMDs is hypoventilation. Treatment should aim to correct this situation; thus, ventilation support is fundamental. In the case of chronic hypercapnic respiratory insufficiency, oxygen therapy can accentuate hypoventilation by inhibiting the only other stimulus for ventilation that remains: hypoxemia. Therefore, special care should be taken when considering indications for oxygen therapy in these patients.
Prognosis
Prognostic features of neuromuscular diseases
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


