Chapter 85
Complex Regional Pain Syndrome
Ali F. AbuRahma
Complex regional pain syndrome (CRPS), previously called posttraumatic pain syndrome, causalgia, or reflex sympathetic dystrophy, is one of the most poorly understood and frequently misdiagnosed entities encountered in clinical practice. This painful condition can develop after damage to peripheral nerves in a variety of settings. In susceptible patients, the initiating event may be relatively insignificant or even obscure.
The term causalgia is derived from the Greek causos, meaning “heat,” and algos, meaning “pain” (i.e., burning pain).1 Although it was described in detail by Mitchell et al1 in 1864, Paré may have reported the first case in the 16th century.2 These early reports described incomplete peripheral nerve injury secondary to penetrating trauma with subsequent burning pain, autonomic dysfunction, and “limb atrophy.” With time, however, symptoms of similar severity were noted to occur subsequent to trauma of a less serious nature and even in the absence of obvious injury to a peripheral nerve. In 1973, Patman et al3 consolidated the many terms that had appeared in the literature describing a variety of pain syndromes similar to causalgia but of different causes under the name mimocausalgia. This term, also derived from Greek, means “imitating causalgia.” Previously, it had been popular to refer to these syndromes as minor causalgia, in contrast to the full-blown symptom complex associated with incomplete nerve injuries, referred to as major causalgia.
Etiology and Incidence
The exact incidence of CRPS is unknown, but it has been estimated to occur in at least 1% to 12% of patients with peripheral nerve injury.4 A North American population-based study and a European study reported incidences of 5.6 and 26.2 per 100,000 person-years, respectively.5 Three precipitating causes of CRPS have been identified.
Traumatic
Traumatic causes include peripheral nerve injuries, fractures, dislocations, sprains, crush injuries, burns, and iatrogenic injuries. Most cases of CRPS are posttraumatic.5 CRPS has also been reported in 0.2% to 11% of patients with Colles’ fracture6 and in 12% to 20% of patients with hemiplegia.7 The incidence of CRPS type 2 (as defined later) has been reported as 1.5% in the Vietnam War, 8% in the Persian Gulf War,8 and a high of 32% in the Civil War.9 CRPS has also been reported in patients with spinal cord and brain injuries with an incidence of 5% to 12%.8–10 Hassantash11 reported the results of a meta-analysis of the literature on the subject of causalgia; 110 articles contained a total of 1528 cases of causalgia. High-velocity missiles caused at least 77% of the injuries. The median nerve alone or in combination with other nerves (56%) and the sciatic nerve (60%) were most commonly involved. In 92%, the nerve injury was incomplete.
Nontraumatic
Nontraumatic causes include prolonged bed rest, neoplasms, metabolic bone disease, deep venous thrombosis, myocardial infarction,5 and stroke.5 The incidence of CRPS in patients experiencing myocardial ischemia varies between 5% and 20%.8 Chronic painful conditions of the upper extremity subsequent to myocardial infarction have been grouped into a category designated shoulder-hand syndrome and have been reported in up to 15% of patients,4 although the incidence has recently been reduced because of much more rapid postinfarction mobilization. Other associated disorders, such as osteoporosis, migraine, neuropathies, and menstrual dysregulation, have been implicated.5
Idiopathic
No recognizable idiopathic cause is identified.
Classification and Terminology
Box 85-1 lists more than 40 terms that describe CRPS. The most common terms used to describe CRPS include the following: posttraumatic pain syndrome; causalgia—minor and major; minor and major traumatic dystrophy, describing the intensity of the syndrome when it develops after an injury that does not damage a peripheral nerve; shoulder-hand syndrome; reflex sympathetic dystrophy that involves the entire upper extremity; and Sudeck’s atrophy, a posttraumatic reflex dystrophy with bone involvement demonstrable on radiographs.
Stanton-Hicks and associates convened a consensus committee (International Association for the Study of Pain) to address the nomenclature of causalgia and reflex sympathetic dystrophy.12 The term complex regional pain syndrome was developed to replace the terms causalgia and reflex sympathetic dystrophy. Hallmarks of this syndrome include dysfunction and pain of duration or severity out of proportion to what might be expected from the initiating event.13,14
Syndrome Types
Two types of CRPS have been recognized. Type 1 corresponds to the former term reflex sympathetic dystrophy and type 2, to the former term causalgia. The definitions of CRPS types 1 and 2 contain criteria that exclude (1) pain and other findings that are physiologically, anatomically, and temporally appropriate to some form of injury and (2) myofascial pain syndrome.
The diagnostic criteria for CRPS type 1 (formerly reflex sympathetic dystrophy), as modified from Stanton-Hicks et al14 and Merskey and Bogduk,15 are as follows:
The diagnostic criteria for CRPS type 2 (formerly causalgia) are as follows:
Pathogenesis
Several theories have been proposed to explain CRPS during the past few decades, but none has been universally accepted. Past theories included the artificial synapses theory by Doupe et al,16 the vicious circle of reflexes theory proposed by Livingston,17 and the gate control theory.18 The currently accepted major theories that have been proposed to explain the pathogenesis of CRPS are summarized here.
Current Theories
Exaggerated Local Inflammatory Response Theory and Neurogenic Inflammation
Several authorities have suggested that CRPS can occur secondary to an exaggerated local inflammatory response to injury, resulting in disruption of the autoregulation of blood flow and in turn giving rise to the classic phases of CRPS.19 It has been suggested that some of the clinical features of CRPS in its early stage can be explained by an inflammatory process. This theory was originally proposed by Sudeck.20 The painful affected limb is usually hot, red, swollen, and with reduced function, which are signs of inflammation. Studies have shown that inflammatory mediators (e.g., tumor necrosis factor-α, interleukin-6) are elevated in blister fluid and blood samples obtained from affected limbs.21 This theory is supported by the fact that corticosteroids are often successful in the treatment of patients with acute CRPS.22 The reported efficacy of low-dose intravenous immune globulins could be due to an anti-inflammatory effect.23 Bisphosphonates, which have immune modulatory properties, were also effective in four small randomized controlled trials involving CRPS of less than 6 months in duration.19
Neurogenic inflammation has been implicated further on the basis of studies of calcitonin gene–related peptide, which was found to be elevated in the sera of CRPS patients.21 It has been suggested that a localized neurogenic inflammation may be involved in the production of vasodilatation, acute edema, and increased sweating. Neuropeptides released from sensory neurons cause skin reddening and swelling, which are seen in affected limbs. When C fibers in affected and to a lesser degree in unaffected limbs are experimentally activated, CRPS patients respond with much stronger neuropeptide-mediated skin reddening and swelling than control patients do.19
The importance of neuropeptides in the pathophysiologic process of CRPS is further underlined by the finding that CRPS is associated with angiotensin-converting enzyme inhibitor therapy.19 Angiotensin-converting enzyme metabolizes the neuropeptide substance P and bradykinin to inactive forms; thus angiotensin-converting enzyme inhibitors may lead to higher tissue levels of these neuropeptides. These findings have not yet been translated into clinical management of CRPS.
CRPS as a Sympathetically Mediated Syndrome
The role of the sympathetic nervous system in CRPS remains controversial. Evidence in favor of a role for this system is in part based on color, temperature, and sweating differences between CRPS-affected and unaffected limbs. These differences are thought to be mediated by sympathetic dysregulation. There is a low centrally mediated sympathetic outflow to cutaneous vasoconstrictors in an affected limb, which may produce a red and warm extremity.19 Local anesthetic application to the sympathetic ganglia (e.g., stellate or lumbar sympathetic block) can relieve pain for the short term in selected patients,19,24 although repeated applications do not necessarily prolong the effect.25 The sympathetically maintained pain can be reduced by sympathetic blockade, particularly in the early stage of CRPS, but this is rare in long-standing CRPS.26
Evidence that does not support a primary role for the sympathetic system includes the finding that other vasomotor signs, such as bluish discoloration and cold temperature, may be due to supersensitivity or upregulation of receptive adrenal receptors rather than a dysregulation of the sympathetic outflow.19 The vasomotor and sudomotor signs often diminish with time. It has been suggested that the permanent cold temperature in some cases of late CRPS may be due to endothelial rather than sympathetic dysfunction.19 Hannington-Kiff 27 noted that agents that deplete the limb autonomic nerve endings of norepinephrine (e.g., regional guanethidine) should therefore be effective; however, all four randomized controlled trials conducted to assess this therapy have been negative.19 Many clinicians using this method (i.e., intravenous regional sympathetic block) have demonstrated that it reduced pain in some patients,19 and one wonders whether this effect was the result of the application of a tourniquet. Intravenous regional sympathetic block may be more effective with saline than with guanethidine.19
CRPS as the Result of Limb Ischemia-Reperfusion Injury
Some investigators believe that CRPS type 1 is an abnormal inflammatory response to a deep tissue injury, producing a picture of a compartment syndrome with resultant oxygen free radical–induced microvascular dysfunction, further ischemia and inflammation, and nociceptor excitement.19 Coderre et al28 reported in an animal model that transient application of limb ischemia produced a syndrome similar to CRPS. Koban et al29 showed that there was some evidence for low oxygen tension in the superficial skin layers of affected limbs, potentially enhancing the idea that ischemia might also be present in deeper tissues. The use of vitamin C in preventing the development of CRPS after radius fracture has been thought to be due to the scavenging of free oxygen radicals.19 Groeneweg et al,30 in a pilot study, showed that tadalafil (a phosphodiesterase inhibitor) reduced pain in some CRPS patients with cold limbs. This was thought to be secondary to its vasodilator property and may also explain the mechanism of sympathetic blocks in these patients.
Central Sensitization Theory
Central sensitization is the physiologic manifestation of severe peripherally induced pain.31 It is the molecular process that corresponds to the observation that after a period of repeated or intense noxious or innocuous stimuli, the involved extremity or site of pain becomes painful and remains so even after the initial stimulation has subsided.19 This theory is thought to be important in most chronic pain.19 It is believed that N-methyl D-aspartate (NMDA) receptors may play an important role in central sensitization. In two randomized clinical trials, low-dose intravenous ketamine (an NMDA antagonist) dramatically reduced CRPS pain, which may indicate an important role for such central sensitization.19 Ketamine strongly reduced the average pain intensity for several weeks, independent of the duration of CRPS syndrome, but without improving function. One limitation of ketamine infusion is its potential for neurotoxicity.19 The current protocols of ketamine treatment are also cumbersome and expensive; they are given during a 5-day hospital in-patient stay or a consecutive 10–working day outpatient therapy. Intravenous magnesium therapy, which is similar to ketamine therapy, may reduce central sensitization.19
CRPS Secondary to Nerve Damage
Permanent dysfunction of small-diameter primary afferent nociceptor axons distal to a site of trauma is associated with CRPS. The similarity of CRPS to small fiber–predominant polyneuropathy stimulated the idea that regionally restricted small nerve fiber damage may occur in CRPS, rather than sympathetic dysfunction, and may be responsible for CRPS signs.19 Studies of CRPS amputated limbs and skin biopsy specimens showed small fiber loss.19 Therefore, it is postulated that CRPS type 1 syndrome may, in fact, represent a neuropathic pain syndrome.
CRPS as an Autoimmune Disorder
Goebel19 showed evidence for antineuronal autoantibodies in 30% of patients in one study of CRPS patients. In another study, Blaes et al32 demonstrated these antibodies in 90% of the study group. Both groups of investigators demonstrated that passive transfer of patient serum immunoglobulin G antibodies elicits abnormal motor functions and behavior in mice similar to that found in CRPS, suggesting a functional effect.19 Goebel also demonstrated, in a randomized clinical trial, that a single infusion of low-dose intravenous immune globulin effectively reduces pain in patients with long-standing CRPS. It has been postulated that if autoantibodies are involved, therapeutic strategies such as plasmapheresis or reverse vaccination may be beneficial.19
Cortical Reorganization Theory
Functional magnetic resonance imaging (MRI) studies during the last several years have shown that sensory representations of CRPS-affected limbs are altered, that the degree of this alteration corresponds to pain intensity, and that reduction in pain is associated with normalization.19 There are also changes in the motor cortex. CRPS patients often feel alienation toward their affected limb; the limb can feel strange and disfigured. Computer-based graded motor imagery, which consists of exercise to train the brain in better recognition of the affected limb, can decrease swelling and pain in some CRPS patients.19 Mirror therapy (advocated by McCabe; see later) for the treatment of CRPS requires that the patient hide the affected limb behind a mirror placed perpendicular to the body midline. When the patient looks into the mirror and performs bilateral synchronized gentle movement, the affected limb (in actuality the reflection of the unaffected limb in the mirror) appears and moves normally. This therapy has been shown to minimize both early and late pain in some patients with CRPS33 and strongly suggests that signs such as swelling are, in part, under cortical control.
Genetic and Other Theories
A genetic association has been implicated in patients with CRPS. Most studies have examined HLA associations,19 but the data have not been robust. A few investigators have suggested that CRPS has a psychological origin.19 However, a systematic investigation did not confirm this association.34
Sympathetically Maintained Pain and Sympathetically Independent Pain
The term sympathetically maintained pain has been used to describe the pain maintained by sympathetic efferent innervation, circulating catecholamines, or neurochemical action; it can be relieved by pharmacologic blockade or local anesthetic block of the sympathetic ganglia that serve the painful area.35,36 Sympathetically independent pain refers to pain states not sustained by the sympathetic nervous system. Sympathetically maintained pain may vary over time, and it has been suggested that patients with CRPS may have a pain syndrome in which part of the pain is sympathetically maintained and another part is sympathetically independent (i.e., the patient can have both sympathetically independent pain and sympathetically maintained pain at the same time or may have sympathetically maintained pain at one time and sympathetically independent pain later).13
Clinical Presentation
Clinical Stages
Drucker et al37 have divided the natural history of CRPS into three clinical stages.
Stage 1, acute (0-3 months): Stage 1 is characterized by warmth, erythema, burning, edema, hyperalgesia, hyperhidrosis, and, after a few months, patchy osteoporosis. At this stage, a good result can be expected with Bier’s block or chemical sympathectomy, one that often lasts longer than the normal duration of the block. Spontaneous resolution may occur in this stage, and the clinical course is reversible.
Although these stages oversimplify the condition, they provide a framework for diagnosis, treatment, and prognosis of CRPS. For example, among patients who are in stage 1 or 2, prompt treatment may produce permanent relief of pain, and sympathectomy may not be required. However, for patients in stage 3, the likelihood of a poor result is greater, and even sympathectomy may not provide lasting relief.
Symptoms and Signs
CRPS type 1 can occur in any age group but has a peak incidence between the ages of 55 and 75 years, with a female-to-male ratio of 2 : 1. Although CRPS type 1 has been reported in children, it is less disabling than in adults.
The clinical criteria for the diagnosis of CRPS, as outlined by Stanton-Hicks et al,12,14 have been described previously and are summarized in Box 85-2 and Figure 85-1.
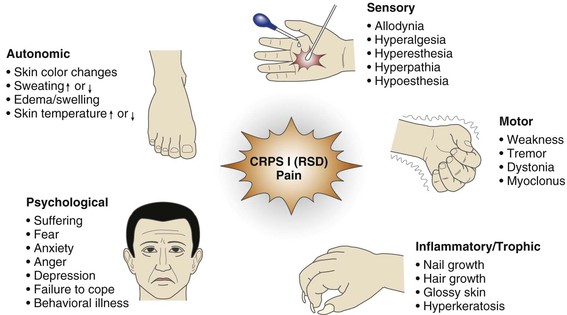
Figure 85-1 Clinical features of complex regional pain syndrome (CRPS) type 1 (reflex sympathetic dystrophy [RSD]).
Pain
Pain is a necessary symptom for the diagnosis of CRPS. It is located in the affected extremity and is disproportionate to what would be expected from the initial event. It may be spontaneous or evoked and is usually reported as diffuse. It is not consistent with the distribution of a peripheral nerve, even if the initial injury involved such a nerve. This important feature distinguishes CRPS from pain of other causes and from more specific neuropathic pain disorders. The pain may be reported as burning, throbbing or aching, intermittent or continuous, and exacerbated by physical or emotional stresses. The patient often adopts a protective posture to protect the affected extremity.
Sensory Changes
Sensory changes are usually reported at some stage and include allodynia and hyperesthesia in the region of the pain. Allodynia may occur in response to thermal stimulation (cold or warm), deep pressure, light touch, or joint movement.
Sympathetic Dysfunction
Sympathetic dysfunction is reported as a sudomotor or vasomotor instability in the affected extremity compared with the unaffected extremity. This dysfunction may vary in severity from time to time, and the patient may report that the extremity is warm and red or cold and blue, purple, or mottled. Veldman et al38 reported that 92% of patients had altered skin temperature. Sweating, particularly in the palms or soles, may be reported as increased, decreased, or unchanged. Normal sympathetic function may be present at certain times. Swelling may be reported at any stage of the syndrome and is typically peripheral. It may be intermittent or continuous and may be exacerbated by the dependent position of the extremity. There can also be pitting or brawny edema.
Trophic and Motor Changes
Trophic changes of the skin may be reported later in the course of the syndrome. The nails may be atrophic or hypertrophic. Hair growth and texture may be decreased or increased, and the skin may become atrophic. Motor dysfunction may include dystonia, tremor, and loss of strength of the affected muscle groups. Joint swelling and stiffness may also be reported, particularly of the digits.
Budapest Diagnostic Criteria
The Budapest diagnostic criteria were published to facilitate the clinical diagnosis39 and were updated in 2007.19,40 They are as follows:
• Must report at least one symptom in each of the following four categories:
• Sudomotor/edema: sweating changes and/or edema and/or sweating asymmetry
• Vasomotor: skin color changes and/or temperature asymmetry and/or skin color asymmetry
• Must display at least one sign in two or more of the following categories:
• Sensory: evidence of allodynia (to light touch) and/or hyperalgesia (to pinprick)
• Sudomotor/edema: evidence of sweating changes and/or edema and/or sweating asymmetry
• Vasomotor: evidence of skin color changes and/or temperature asymmetry and/or skin color asymmetry
Diagnostic Evaluation
Comprehensive Clinical Tests
With the foregoing features in mind, the clinical evaluation can be enhanced by focusing on particular aspects or by adjunctive tests, as follows.
Sensory Examination
Sensory impairment can include allodynia, mechanical or thermal hyperalgesia, hyperesthesia, or hypalgesia. These sensory impairments can be localized (glove-like) or generalized. Quantitative sensory testing to confirm the clinical findings of sensory abnormalities can be applied; however, this is not specific for patients with CRPS.41
Sudomotor Sympathetic Examination
Resting heat output may be estimated by skin impedance42; by quinizarin or cobalt blue testing43; or as part of the quantitative sudomotor axon reflex test,44 which measures resting sweat output by hygrometry and changes evoked by iontophoresis of acetylcholine into the skin.45 These tests are useful diagnostic tools for CRPS; however, they are difficult to conduct and are not generally recommended for the routine diagnosis of CRPS.41,46
Vasomotor Examination
Simultaneous temperature measurements of both the affected and unaffected extremities are taken at corresponding anatomic sites. The temperature of the digit pads, palms and soles, and forearms and calves can be measured with noncontact thermometry or thermography. Serial measurements should be taken because peripheral temperatures vary widely under normal circumstances. Skin perfusion can be evaluated visually or by pulse oximetry.
Edema
Edema is judged clinically by comparing one extremity with the other because most volume displacement methods are cumbersome.
Trophic Changes
The skin, hair, and nails of the two sides are compared.
Motor Dysfunction
The presence of dystonia, tremor, and changes in strength can be measured. Objective measurements should be taken (e.g., apposition and opposition pinch strength, grip, and weight bearing on lower extremity).
Psychological Testing
Psychological testing has been used to rule out concomitant mental illness but has not been validated in CRPS.34
Neurophysiologic Testing
The diagnosis of CRPS type 2 requires documentation of a peripheral nerve lesion. CRPS may also develop after central nervous system lesions (brain tumor or brain infarct); therefore, it is important to confirm or to exclude peripheral nerve or central nervous system lesions. Nerve conduction studies may show discrete abnormalities secondary to edema or peripheral vasoconstriction.41 Distinct abnormalities of more than 20% of normal values should be observed in CRPS type 2. Somatosensory evoked potentials after ulnar/median or tibial nerve stimulation testing can also be abnormal in patients with CRPS type 2, although they are usually normal in patients with CRPS type 1. Overall, these tests can be useful in the diagnosis of CRPS types 1 and 2, confirming peripheral nerve or central nerve system lesions. However, the findings are not specific.
Electromyography recordings are not frequently used in patients with CRPS because they are painful and may exaggerate the pain of CRPS.
Inflammatory Parameter Assessment
Neuroinflammatory mediators such as substance P, bradykinin, and calcitonin gene–related peptide are usually increased in patients with CRPS. Other systemic inflammatory markers (e.g., C-reactive protein, erythrocyte sedimentation rate, and leukocyte count) are not elevated.47
Radiologic Findings
The primary radiographic manifestations in patients with CRPS are diffuse osteoporosis with severe patchy demineralization, especially of the periarticular regions, with a subperiosteal bone resorption.20,41 However, these changes are late and nonspecific.
Three-Phase Bone Scans
Three-phase bone scans have been used for the diagnosis of CRPS during the past 3 decades.48,49 Accelerated blood flow into the diseased limb, combined with an increased diffuse activity during the blood pool phase and an increased periarticular uptake in the delayed static phase, is considered to be pathognomonic for CRPS (Fig. 85-2). In a meta-analysis of 24 studies analyzing imaging techniques for the diagnosis of CRPS type 1, Cappello et al50 supported the use of the triple-phase bone scan to rule out CRPS type 1 owing to its greater sensitivity and higher negative predictive value compared with both MRI and plain film radiography.

Figure 85-2 Three-phase bone scan in complex regional pain syndrome of the left hand, demonstrating osteopenia. (From Schurmann M, et al: Early diagnosis in post-traumatic complex regional pain syndrome. Orthopedics 30:450-456, 2007.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


