23 Complex and Multi-vessel Percutaneous Coronary Intervention
Patients with multi-vessel coronary disease represent an important group of patients with coronary artery disease (CAD). Although various definitions of multi-vessel disease have been used in different studies, in clinical terms, this generally refers to the presence of two-vessel or three-vessel disease as delineated by coronary angiography. Patients with three-vessel coronary disease or two-vessel disease with proximal left anterior descending (LAD) artery involvement represent a subgroup of patients with CAD, in whom survival benefit with bypass surgery has been clearly established.1 Over the years, considerable advances have been made in revascularization techniques by means of CABG and with PCI. With the constant evolution of techniques, there has been a tremendous interest in comparing the outcomes of these modalities with a view to determining appropriate clinical practice. In broad terms, the clinical studies that have compared CABG with PCI can be viewed in terms of three major groups when evaluated from the standpoint of important developments in the history of PCI. With the advent of percutaneous coronary balloon angioplasty (PTCA), multiple studies were conducted to compare PTCA with CABG. These represent the first group of studies comparing PCI with CABG. The development of coronary stents leads to a second series of comparisons of PCI with stenting to CABG. Important lessons have been learned from both these groups of studies, and the findings of the important literature from this period will be presented below. With the arrival of the DES, more recent studies have continued to focus on comparisons of PCI with the DES to CABG. This last group of studies is the most relevant to contemporary clinical practice and will be discussed in detail.
 Percutaneous Coronary Balloon Angioplasty Versus Coronary Artery Bypass Grafting
Percutaneous Coronary Balloon Angioplasty Versus Coronary Artery Bypass Grafting
BARI
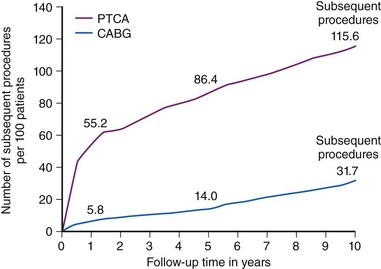
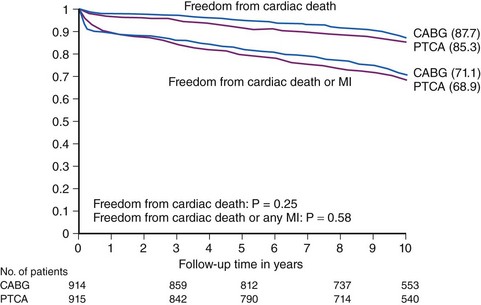
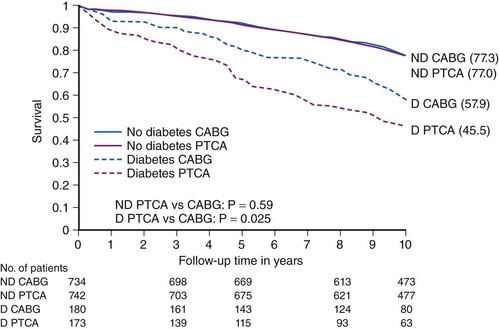
In the BARI (Bypass Angioplasty Revascularization Investigation) trial, symptomatic patients with multi-vessel CAD (n = 1829) were randomly assigned to initial treatment with PTCA or CABG. The 10-year survival was 71% for PTCA and 73.5% for CABG (P = 0.18). At 10 years, the PTCA group had substantially higher subsequent revascularization rates compared with the CABG group (76.8% vs. 20.3%, P < 0.001), but the angina rates for the two groups were similar. In the subgroup of patients who had not been treated for diabetes, survival rates were nearly identical by randomization (PTCA 77% vs. CABG 77.3%, P = 0.59). In the subgroup who had been treated for diabetes, the CABG group had higher survival compared with the PTCA group (PTCA 45.5% vs. CABG 57.8%, P = 0.025) (Figs. 23-1, 23-2 and 23-3).2
RITA
In the RITA (Randomised Intervention Treatment of Angina) trial, 1011 patients with coronary heart disease (45% single-vessel, 55% multi-vessel) were randomly assigned to initial treatment with PTCA or CABG. The median follow-up was 6.5 years. The primary endpoint of death or nonfatal MI occurred in 17% of the PTCA group and 16% of the CABG group (P = 0.64). Subsequent nonrandomized CABG was undertaken in 134 (26%) of the PTCA group, and a second CABG was undertaken in 14 (3%) of the CABG group. In the PTCA group, 138 (27%) patients required an additional nonrandomized PTCA at some point; 45 of these also required a nonrandomized CABG. In the CABG group, 47 (9%) required nonrandomized PTCA subsequently; 7 of these also required a second CABG. The prevalence of angina was consistently higher in the PTCA group, with an absolute average 10% increase compared with the CABG group (P < 0.001).3
GABI
The GABI (German Angioplasty versus Bypass surgery Investigation) trial compared the outcomes in patients 1 year after complete revascularization with CABG or PTCA. A total of 8981 patients with multi-vessel CAD were randomly assigned to undergo CABG (177 patients) or PTCA (182 patients). During the first year of follow-up, further interventions were necessary in 44% of the patients in the PTCA group (repeated PTCA in 23%, CABG in 18%, and both in 3%) but in only 6% of the patients in the CABG group (repeated CABG in 1% and PTCA in 5%, P < 0.001). Seventy-four percent of the patients in the CABG group and 71% of those in the PTCA group were free of angina 1 year after treatment.4
EAST
The Emory Angioplasty versus Surgery Trial (EAST) was a single-center, randomized comparison of a strategy of initial coronary angioplasty (n = 198) or CABG (n = 194) for patients with multi-vessel CAD. The primary endpoint (death, MI, or a large ischemic defect at 3 years) was not different, and repeat revascularization was significantly greater in the angioplasty group. Survival at 8 years was 79.3% in the angioplasty group and 82.7% in the surgical group (P = 0.40). Patients with proximal LAD artery stenosis and those with diabetes tended to have better rates of late survival with surgical intervention, although not reaching statistical significance. After the first 3 years, repeat interventions remained relatively equal for both treatment groups.5
CABRI
The Coronary Angioplasty versus Bypass Revascularization Investigation (CABRI) was a multi-national, multi-centre, randomized trial comparing the strategies of revascularization with CABG and PTCA in patients with symptomatic multi-vessel CAD. Of the 1054 patients recruited, 513 were randomized to CABG and 541 to PTCA. After 1 year of follow-up, 2.7% of those randomized to CABG and 3.9% of those randomized to PTCA had died; this difference was not significant. However, patients randomized to PTCA required significantly more re-interventions; at 1 year, only 66.4% required a single-vessel revascularization procedure compared with 93.5% of patients randomized to CABG (relative risk [RR] = 5.23; 95% confidence interval [CI] 3.90–7.03, P < 0.001). The patients in the PTCA group took significantly more medication at 1 year (RR = 1.30; CI 1.18–1.43, P < 0.001). They were also more likely to have clinically significant angina (RR = 1.54; CI 1.09–2.16, P = 0.012); this association was present in both genders but was significant only in females.6
ERACI
In ERACI (Argentine Randomized trial of Percutaneous Transluminal Coronary Angioplasty vs. coronary artery bypass surgery), 127 patients who had multi-vessel CAD and clinical indication of myocardial revascularization were randomized to undergo coronary angioplasty (n = 63) or bypass surgery (n = 64). At 3 years, freedom from combined cardiac events (death, Q wave MI, angina, and repeat revascularization procedures) was significantly greater for the bypass surgery group compared with the coronary angioplasty group (77% vs. 47%, P < 0.001). There were no differences in overall (4.7% vs. 9.5%, P = 0.5) and cardiac mortality (4.7% vs. 4.7%) or in the frequency of MI (7.8% vs. 7.8%, P = 0.8) between the two groups. However, patients who had bypass surgery were more frequently free of angina (79% vs. 57%, P < 0.001) and required fewer additional re-interventions (6.3% vs. 37%, P < 0.001) compared with patients who had coronary angioplasty.7 These early trials, although perhaps no longer directly relevant to current clinical practice, yielded a series of important findings. Firstly, survival in patients with multi-vessel disease was found to be similar for PTCA and CABG except in patients with diabetes, for whom CABG was advantageous. The key difference between the procedures was found to lie in the substantially greater need for revascularization procedures in patients treated with PTCA. With the development of coronary stents, it was clearly established that coronary stenting was associated with a lower risk of repeat revascularization procedures compared with balloon angioplasty alone. This led to a second series of comparisons of CABG with PCI, this time with the use of coronary artery stents. These trials are summarized below.
 Percutaneous Coronary Intervention with Bare Metal Stenting Versus Coronary Artery Bypass Grafting
Percutaneous Coronary Intervention with Bare Metal Stenting Versus Coronary Artery Bypass Grafting
ARTS
In the ARTS (Arterial Revascularization Therapies Study) trial, a total of 1205 patients were randomly assigned to CABG (n = 605) or stent implantation (n = 600). At 5 years, there was no significant difference in survival between the stent and CABG groups (8% for stents vs. 7.6% for CABG, P = 0.83). In a subgroup of 208 patients with diabetes, mortality trended higher in the stent group (13.4%) compared with 8.3% in the CABG group (P = 0.27). The overall freedom from death, stroke, or MI was not significantly different between the groups (18.2% in the stent group vs. 14.9% in the surgical group, P = 0.14). However, the incidence of repeat revascularization was significantly higher in the stent group (30.3%) than in the CABG group (8.8%, P < 0.001). The composite event-free survival rate was 58.3% in the stent group and 78.2% in the CABG group (P < 0.0001). This difference was largely driven by the differences in revascularization rates.8
AWESOME
In the AWESOME (Angina With Extremely Serious Operative Mortality Evaluation) study, patients from 16 Veterans Affairs Medical Centers were screened to identify those with myocardial ischemia refractory to medical management and the presence of one or more risk factors for adverse outcome with CABG. A total of 232 patients were randomized to CABG and 222 to PCI. The 30-day survivals for CABG and PCI were 95% and 97%, respectively. At 36 months, there was no significant difference in survival—79% and 80% for CABG and PCI, respectively. However, there was a difference in survival free of revascularization: 66% and 44% for CABG and PCI, respectively (P = 0.001).9
MASS-II
MASS-II (Medicine, Angioplasty, or Surgery Study II) included 611 patients, who were randomly assigned to undergo CABG (n = 203), PCI (n = 205), or medical therapy (n = 203). The inclusion of the medical therapy arm made this trial different from many of the other studies. The rates of event-free survival, namely, the combined incidence of overall mortality, MI, or refractory angina that required revascularization, were significantly different among patients in the 3 therapeutic groups at 5-year (P = 0.0026) and 10-year (P < 0.0001) follow-up. Pairwise treatment comparisons of the primary end points at 5-year follow-up demonstrated no significant difference between PCI and medical therapy (hazard ratio [HR] 0.93, 95% CI 0.67 to 1.30). At 10-year follow-up, this comparison continued to demonstrate a nonsignificant difference between the PCI and medical therapy groups (HR 0.79, 95% CI 0.62 to 1.01). After multivariate Cox analysis at 10-year follow-up, a protective effect of CABG compared with medical therapy (HR 0.43, 95% CI 0.32 to 0.58, P < 0.001) and PCI (HR 0.53, 95% CI 0.39 to 0.72, P < 0.001) was observed.10,10a
SOS
The aim of the Stent or Surgery (SoS) trial was to assess the effect of stent-assisted PCI versus CABG in the management of patients with multi-vessel disease. In 53 centers in Europe and Canada, symptomatic patients with multi-vessel CAD were randomized to CABG (n = 500) or stent-assisted PCI (n = 488) and then followed up for a median of 2 years. Twenty-one percent (n = 101) of patients in the PCI group required additional revascularization procedures compared with 6% (n =30) in the CABG group (P < 0.0001). At a median follow-up of 6 years, 53 patients (10.9%) died in the PCI group compared with 34 (6.8%) in the CABG group (HR 1.66; CI 1.08–2.55, P = 0.022). The incidence of death or Q wave MI was similar in both groups (PCI 9%; [n = 46], CABG 10% [n = 49], P = 0.80). There were fewer deaths in the CABG group than in the PCI group (PCI 5% [n = 22], CABG 2% [n = 8], P = 0.01). This seemed to result, at least in part, from a higher proportion of noncardiovascular deaths in the PCI arm (from cancer) compared with the CABG arm. Additionally, the mortality rate in the CABG group was lower than the rates that had been reported in previous studies. Subsequently, it was seen that at a median follow-up of 6 years, 53 patients (10.9%) had died in the PCI group compared with 34 (6.8%) in the CABG group (HR 1.66; CI 1.08–2.55, P = 0.022).11
ERACI II
The ERACI II trial randomized a total of 450 patients with multi-vessel disease to undergo either PCI (n = 225) or CABG (n = 225). At the 5-year follow-up, patients initially treated with PCI had similar survival and freedom from nonfatal acute MI than those initially treated with CABG (92.8% vs. 88.4% and 97.3% vs. 94%, respectively, P = 0.16). Freedom from repeat revascularization procedures (PCI or CABG) was significantly lower with PCI compared with CABG (71.5% vs. 92.4%, P = 0.0002). Accordingly, driven by a greater need for revascularization, freedom from major adverse cardiac events (MACEs) was also significantly lower with PCI compared with CABG (65.3% vs. 76.4%, P = 0.013). However, at 5 years, similar numbers of patients randomized to each revascularization procedure were asymptomatic or with class I angina.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree