It has been unclear the impact of manual thrombus aspiration (TA) on procedural outcomes in patients with ST-elevation myocardial infarction (STEMI) who underwent rescue percutaneous coronary intervention (PCI) after failed fibrinolytic therapy in comparison with primary PCI. Our aim was to test the hypothesis that manual TA may improve myocardial reperfusion and clinical outcomes in patients with STEMI who underwent rescue PCI after failed fibrinolytic therapy. From March 2011 to March 2014, 70 patients with STEMI after unsuccessful fibrinolysis were randomized to either rescue PCI with TA (TA group) or without TA (NTA group). Primary end points were rate of myocardial blush grade ≥2 and ST-segment resolution ≥70%. The secondary end point included 30 days follow-up for major adverse cardiac events (MACEs). Baseline clinical and angiographic characteristics were similar in the 2 groups. The TA and NTA groups were compared as follows: myocardial blush grade ≥2, 71% versus 46% (p <0.05); complete ST-segment resolution 71% versus 46% (p <0.05); no reflow 20% versus 49% (p <0.05); procedure time (min) 65.0 ± 38.6 versus 90.1 ± 28.8 (p <0.05); contrast amount (ml) 99.0 ± 45.2 versus 121.2 ± 33.4 (p <0.05); and direct stenting 60% versus 37% (p <0.05). There was a significant reduction of MACE in the TA group, 20% versus 37% (p <0.05). In conclusion, rescue PCI with manual TA leads to better myocardial reperfusion and significant reduction of MACE.
The preferred treatment for myocardial infarction with ST-segment elevation is primary percutaneous coronary intervention (PPCI), which is effective in opening the infarct-related artery. However, intravenous thrombolysis remains the first-line therapy in 30% to 70% of cases worldwide. Patients in whom fibrinolysis fails to restore patency of infarct-related artery within 90 minutes have worse convalescent left ventricular function, an increased probability of developing mechanical complications of transmural infarction and greater mortality. Rescue PCI is known as the strategy of urgent catheterization after fibrinolytic therapy has clinically failed to restore reperfusion of the infarct artery. The high frequency of suboptimal myocardial reperfusion after PPCI for ST-elevation myocardial infarction (STEMI) has resulted in the development of various studies to evaluate the use of a manual aspiration catheter to improve myocardial perfusion. The results of randomized clinical trials (RCTs), including a meta-analysis of 11,321 patients from 20 RCT showing lower rates of late mortality, reinfarction, and stent thrombosis in patients who underwent manual TA compared with conventional PPCI, led to a recommendation class IIb for manual TA in patients who underwent PPCI for STEMI. In contrast, the results of some studies as the recently published TOTAL (ThrOmbecTomy with PCI vs PCI ALone in patients with STEMI undergoing PPCI) trial did not show any impact of manual TA on mortality or any of several other clinical outcomes in patients with STEMI during PPCI that may change the recommendation of routine TA in PPCI. Moreover, the potential effect of TA on optimization of stent implantation has not been elucidated yet. What about TA in rescue PCI? To date, it has been unclear the impact of TA on procedural outcomes in acute STEMI in patients in whom fibrinolytic therapy is unsuccessful.
Methods
The study was carried out at 2 centers, the first was the department of internal medicine, cardiology division, coronary care, and cathlab units of the Sohag University Hospital and the second was Al-Noor Cardiovascular Intervention Center in the period from March 2011 to March 2014. All patients provided written informed consent, and the study protocol was reviewed and approved by the scientific and ethical committees at the faculty of medicine of the Sohag University Hospital.
We conducted prospective randomized trial at 2 centers for evaluation of end points. The inclusion criteria included patients with symptoms consistent with acute myocardial infarction and the presence of ST-segment elevation >0.1 mV in 2 contiguous or more leads on the electrocardiogram or new left bundle branch block who were treated with recommended therapy, including aspirin, clopidogrel, low–molecular weight heparin, and streptokinase, within 6 hours and able to perform intervention within 12 hours of symptom onset after failed reperfusion documented by clinical and electrocardiographic criteria. Patients with re-infarction or recurrent chest pain with changeable electrocardiogram during the first day of admission were also included. Exclusion criteria included patients who underwent PPCI, those with previous coronary artery bypass graft surgery, those with congenital heart disease or any myocardial disease apart from ischemia, the known existence of a disease resulting in a life expectancy of <12 months, for example, malignancy, and those with the lack of informed consent.
Before coronary angiography was performed, patients were randomly assigned in 1: 1 fashion to undergo either rescue PCI with manual thrombus aspiration (TA group) or standard rescue PCI without thrombus aspiration (NTA group), according to a computer-generated random series.
Coronary angioplasty and stent implantation were performed according to the institutional standards. For all patients, the first procedural step was the passing of a 0.014″ floppy, steerable guidewire through the target lesion. In conventional rescue PCI patients group (NTA group), this step was followed by balloon dilations to establish antegrade flow before implantation of stents. In the TA group, the step of guidewire passage was followed by the advancing of the rapid exchange, 6Fr compatible Manual Thrombus Aspiration Catheter (Diver C; Invatec Company, Roncadelle, Italy, or Stemicath; Minvasys Co., Gennevilliers, France) into the target coronary segment; aspiration was started proximal to the occluded site, gently pushing the catheter through the occlusion and then pulling it in a proximal direction, keeping negative pressure even when the occlusion was crossed or when there was no longer back bleeding in the syringe. Withdrawal of the catheter from the artery and from the guiding catheter was performed with permanent negative pressure. When necessary for stent delivery, balloon dilation was performed before stenting. In all patients, after the restoration of antegrade flow, intracoronary nitrates were given to ensure maximal epicardial vasodilation, to determine the size and length of the stent, and to facilitate stent placement. All placed stents were bare-metal stents (BMS) as MULTI-LINK VISION Coronary Stent System (Abbott Vascular Corporation, Illinois) or Liberté Bare-Metal Coronary Stent (Boston Scientific Corporation, Marlborough, Massachusetts).
Failed reperfusion was defined as at 90 minutes (±15 minutes) after the beginning of initial thrombolytic therapy, and electrocardiogram shows failed thrombolytic therapy—that is, (a) <50% resolution of the ST segment in the lead showing the greatest ST-segment elevation measured from the baseline (isoelectric line) to 80 ms beyond the J point with or without chest pain and (b) chest pain without relief and the absence of reperfusion arrhythmias at 2 hours after treatment.
The primary end point of this study was the rate of angiographic success, which was defined as final Thrombolysis In Myocardial Infarction (TIMI) flow equals ≥2 plus the absence of any angiographic complication. The TIMI flow grade was evaluated pre-wiring and after PCI.
“No-reflow” was defined as a TIMI flow grade <2 in the absence of coronary dissection, coronary hematoma, or epicardial coronary spasm. Thrombus embolization was defined as circumscribed filling defects and/or abrupt cutoff of a vessel distal to the target lesion or in other coronary vessel on the angiogram after PCI. Coronary dissection was defined by the presence of a curvilinear filling defect parallel to the vessel lumen, contrast medium outside the vessel lumen persisting after passage of contrast medium, or a spiral-shaped filling defect partially or totally obstructing the coronary artery lumen. The primary end point also included technical and clinical issues related to the procedure as the number of implanted stents, the rates of direct stenting and post-dilation, the maximal diameter of the implanted stents, the total stent length segment, procedure time (min), contrast amount (ml), and the resolution of the ST-segment elevation after rescue PCI.
Secondary end point was defined as the clinical follow-up data obtained up to 30 days from hospital records and clinical visit or telephone interview. Clinical outcomes were evaluated by measuring the rate of major adverse cardiac event (MACE), that is, a composite of death due to a cardiac cause, re-infarction, target lesion revascularization (TLR), heart failure, and stroke.
All continuous variables were statistically described in terms of mean ± SD. Categorical variables were described with absolute and relative (percentage) frequencies that were compared using the chi-square test or Fisher’s exact test. Comparison of continuous variables between the study groups was done using the Student’s t test; p values were used to describe significance. Statistical significance was set as a p value <0.05. All statistical calculations were done using Statistical Package for Social Sciences (SPSS for Windows) software (version 20.0; SPSS Inc., Chicago, Illinois).
Results
A total of 70 patients had acute STEMI with unsuccessful fibrinolysis were prospectively enrolled in the study from March 2011 to March 2014 and were allocated to the 2 treatment groups: 35 patients were randomized to rescue PCI with manual TA (TA group) arm and 35 to standard rescue PCI (NTA group) arm. Streptokinase was administered to all patients. The 2 groups were matched regarding age, gender, and risk factors of coronary artery disease. There were no significant differences in the baseline characteristics of patients between the 2 groups. The mean time from thrombolytic treatment until the rescue PCI was 117.3 ± 22.6 minutes (range 90 to 190 minutes). Tables 1 and 2 summarize the baseline demographics and clinical and lesion characteristics of the 2 study groups.
| Characteristic | Thrombus aspiration | All Patients (n =70) | P value | |
|---|---|---|---|---|
| Yes (n =35) | No (n =35) | |||
| Age (years) | 0.819 | |||
| Mean ±SD | 53.6±10.7 | 54.2±12.2 | 53.9±11.4 | |
| Range | 33-75 | 31-80 | 31-80 | |
| Men | 21 (60%) | 23 (66%) | 44 (63%) | 0.62 |
| Current Smoker | 9 (26%) | 10 (29%) | 19 (27%) | 0.89 |
| Ex-smoker | 9 (26%) | 7 (20%) | 16 (23%) | |
| Non smoker | 17 (49%) | 18 (51%) | 35 (50%) | |
| Family history of Coronary heart disease | 16 (46%) | 18 (51%) | 34 (49%) | 0.63 |
| Previous myocardial infarction | 17 (49%) | 12 (34%) | 29 (41%) | 0.22 |
| Diabetes Mellitus | 15 (43%) | 17 (49%) | 32 (46%) | 0.63 |
| Hypertension | 21 (60%) | 19 (54%) | 40 (57%) | 0.62 |
| Vascular disease | 14 (40%) | 11 (31%) | 25 (36%) | 0.45 |
| Dyslipidemia ∗ | 15 (43%) | 17 (49%) | 32 (46%) | 0.63 |
| Obesity † | 13 (37%) | 12 (34%) | 25 (36%) | 0.80 |
| Localization of myocardial infarction | ||||
| Anterior | 17(49%) | 17(49%) | 34 (49%) | |
| Inferior | 11(31%) | 10(29%) | 21 (30%) | 0.944 |
| Postero-Lateral | 7(20%) | 8(23%) | 15 (21%) | |
∗ Diagnosis of dyslipidemia is made when either type of lipid abnormalities is present (LDL-cholesterol ≥140 mg/dL, HDL-cholesterol <40 mg/dL l, Triglycerides ≥150 mg/dL) (Serum sampled after overnight fasting).
† Obesity is defined as body mass index exceed 30 kg/m 2 (a measurement obtained by dividing a person’s mass by the square of the person’s height) (WHO 2000).
| Characteristic | Thrombus aspiration Yes (n =35) | Thrombus aspiration No (n =35) | P value |
|---|---|---|---|
| Symptom Onset to lysis time (h) | 6.4±1.9 | 6.7±1.7 | 0.504 |
| Lysis to angio time (min) | 117.0±22.3 | 117.7±23.2 | 0.896 |
| Number of diseased vessels | |||
| 1 | 20 (57%) | 17 (49%) | |
| 2 | 8 (23%) | 10 (29%) | 0.766 |
| 3 | 7 (20%) | 8 (23%) | |
| Infarct-related vessel | |||
| Left anterior descending | 17 (49%) | 17 (49%) | |
| Right coronary | 11 (31%) | 11 (31%) | 1.00 |
| Left Circumflex | 7 (20%) | 7 (20%) | |
| Initial TIMI flow grade | |||
| 0 | 23 (66%) | 24 (69%) | 0.80 |
| 1 | 12 (34%) | 11 (31%) | |
| Number of stents (Mean ±SD) | 1.26±0.44 | 1.60±0.65 | 0.01 |
| Length of stented segment — mm | 26.74±6.10 | 30.43±6.14 | 0.01 |
| Diameter of stented segment — mm | 3.0±0.4 | 2.60±0.32 | 0.04 |
| Procedure Time (min) | 65.0±38.6 | 90.1±28.9 | 0.03 |
| Contrast amount (ml) | 99.0±45.2 | 121.2±33.4 | 0.01 |
| Intra-procedural complications | |||
| No | 28 (80%) | 18 (51%) | 0.01 |
| Yes (No-reflow or Flow-limiting dissections) | 7 (20%) | 17 (49%) | |
| Post-procedural TIMI flow grade ≥2 | 25 (71%) | 18 (51%) | 0.02 |
| MBG ≥2 | 25 (71%) | 16 (46%) | 0.02 |
| Rate of direct stenting | 21 (60%) | 13 (37%) | 0.04 |
| ST segment Resolution (STR) at 30 min | |||
| Complete (≥70%) | 25 (72%) | 16 (46%) | 0.03 |
| Partial (30–70%) | 8 (23%) | 12 (34%) | 0.55 |
| None (<30%) | 2 (5.7%) | 7 (20.0%) | 0.04 |
All patients received 300 mg clopidogrel and low–molecular weight heparin (Sanofi Company, Paris, France) 0.35 to 0.5 mg/kg intravenously, and a stent was positioned in all patients.
No statistically significant difference was recorded between the 2 study groups regarding the number of diseased vessels and infarct-related vessel. However, stent length, number of stents implanted per patient, procedure time (min), and contrast amount were significantly less in the TA group (p <0.05). Diameter of stented segment was significantly more in the TA group (p <0.05). The incidence of angiographic no-reflow was significantly less in the TA group (p = 0.012).
No serious periprocedural complications were recorded in both study groups. None of the complications were thought to be related to the aspiration catheter used. There were no intraprocedural deaths or strokes.
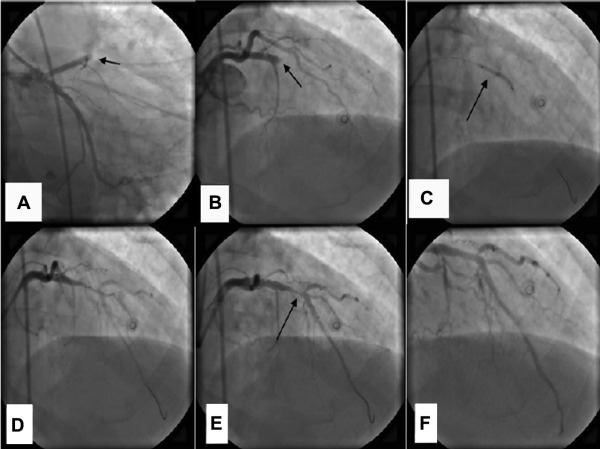
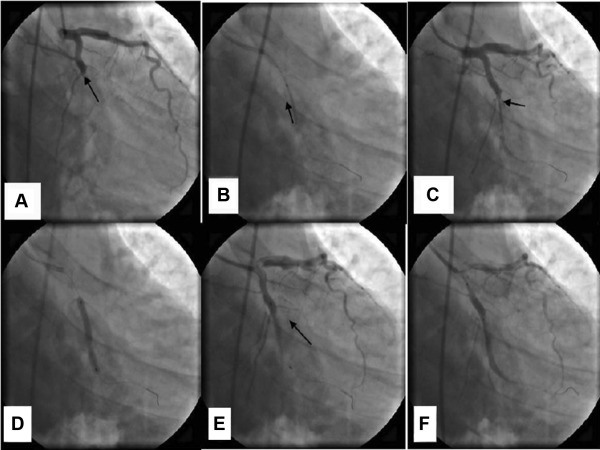
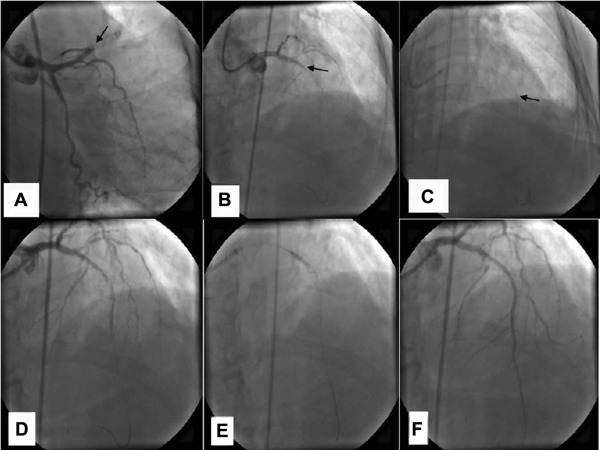
Patients included in the TA group showed higher prevalence of angiographic success and better final TIMI flow (p = 0.022) in comparison with the NTA group. Patients treated with the TA arm versus the standard rescue PCI received higher rate of direct stenting (p <0.05). Stent implantation without predilation was impossible in the TA group (40%) and in the standard rescue PCI group (63%). Figures 1 to 3 and electronic supplementary material online summarize procedural data. The technical success of TA was observed in 100% of patients assigned to TA. After aspiration, final TIMI flow significantly improved in patients with thrombus removal in comparison with standard rescue PCI ( Figure 4 ).