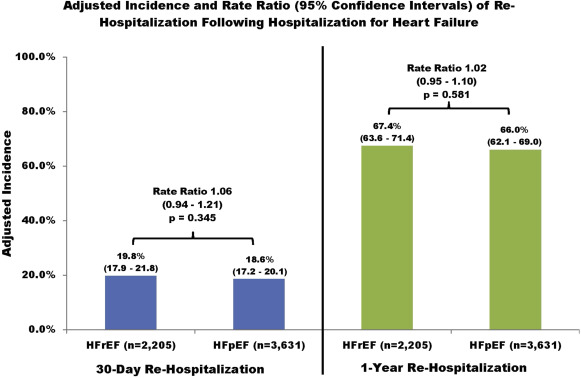
Because heart failure (HF) with reduced ejection fraction (HFrEF) and preserved ejection fraction (HFpEF) are different clinical entities with differing demographic characteristics, common HF outcomes may occur at different rates. Comparative outcome studies have been equivocal, and studies comparing resource utilization are scant. We used an observational cohort design to study 6,513 patients hospitalized for HF who had an EF measured during the hospitalization and were discharged alive within 30 days. We excluded 677 patients with borderline EF values (41% to 49%) and categorized the remaining as HFrEF (EF ≤40%, n = 2,205) and HFpEF (EF >50%, n = 3,631). Patients were followed for up to 1 year for all-cause re-hospitalization and mortality and annualized medical resource utilization. Patients with HFrEF and HFpEF experienced similar adjusted incidence rates of re-hospitalization, but those with HFrEF had a 39% increased risk of mortality at 30 days (rate ratio 1.39, 95% confidence interval 1.10 to 1.76) and 25% greater risk at 1 year (rate ratio1.25, 95% confidence interval 1.12 to 1.41). After adjustment for covariates, patients with HFpEF incurred significantly more annualized outpatient visits (21.5 vs 20.1, p = 0.002) and emergency room visits (3.24 vs 2.94, p = 0.002) than those with HFrEF, but absolute differences were small. High inpatient and pharmacy utilization did not differ. Our study suggests that whether a patient has HFrEF or HFpEF has little bearing on risk of re-hospitalization or inpatient resource utilization in the year after an HF hospitalization. Both groups experienced high mortality, but those with HFrEF had greater risk. In conclusion, from the standpoint of resource use, HF can be considered a single entity.
Heart failure (HF) can have different origins with the most common distinction being drawn on the basis of ejection fraction (EF). In addition to poor left ventricular function, patients with HF with reduced EF (HFrEF) tend to be younger and more likely to be men than those with HF with preserved EF (HFpEF). Because HFrEF and HFpEF are different clinical entities with differing demographic characteristics, it is reasonable to expect that common HF outcomes such as re-hospitalization and mortality would occur at different rates. Some studies report greater mortality, whereas others report similar or lower mortality among patients with HFrEF compared with those with HFrEF. Similarly, rate of re-hospitalization was also been found to be higher in patients with HFrEF in 1 study but equal to that of HFpEF in another. One study found medical costs for a period of 5 years to be similar in patients with HFpEF and HFrEF, but to our knowledge, no study has examined whether medical resource utilization differs between patients with HFrEF and HFpEF. We undertook the present study to compare risk of re-hospitalization, all-cause mortality, and medical resource utilization for up to 1 year after discharge for an HF hospitalization.
Methods
We conducted a retrospective cohort study of members from Kaiser Permanente Southern California (KPSC), serving approximately 3.6 million subjects of Southern California and Kaiser Permanente Northwest (KPNW), serving approximately 480,000 subjects in the Portland, Oregon, area. Virtually, all medical care provided by KPSC and KPNW are captured in electronic databases, including inpatient admissions, outpatient visits, laboratory values, and pharmaceutical dispensings. The KPNW Institutional Review Board approved the study with a waiver of informed consent, and the KPSC Institutional Review Board ceded oversight to KPNW.
We identified all members of these 2 integrated health systems aged ≥18 years who had a hospitalization with a primary discharge diagnosis of HF ( International Classification of Diseases, Ninth Edition [ ICD-9-CM ] 428.xx) and were discharged alive from January 1, 2008, to December 31, 2011, and had no previous HF hospitalization in the preceding 12 months. Patients with <12 months of health plan membership before the index hospitalization were excluded. Of the ∼19,000 potential patients who met these criteria, we excluded 53 patients with length of stay >30 days to avoid undue influence of these uncommon cases on the overall results.
We limited our analyses to the 6,513 patients (34% of potential subjects) who had an echocardiogram during the index hospitalization. Because EF measurements are often imprecise or entered as free text, we implemented a computerized algorithm to categorize EF as reduced (EF ≤40%), borderline (EF 41% to 49%), or normal (EF ≥50%) and excluded the 677 patients who fell into the borderline category, resulting in a final analysis sample of 5,836.
Baseline patient demographic characteristics, clinical risk factors, and medical history were captured from electronic medical record (EMR) data during the 12 months before the index hospitalization. Medical history included previous diagnosis of HF and other co-morbidities including coronary heart disease ( ICD-9-CM 410.x to 414.x), diabetes mellitus ( ICD-9-CM 250.xx), hypertension ( ICD-9 code 401.x to 405.x), and depression ( ICD-9-CM codes 296.2 to 296.8 and 311). We also characterized baseline kidney function using outpatient serum creatinine concentration values to estimate glomerular filtration rate using the Modification Diet in Renal Disease equation, defining chronic kidney disease as an estimated glomerular filtration rate <60 ml/min/1.73 m 2 or the presence of a 585.x ICD-9-CM code.
Our 2 clinical outcomes of interest were re-hospitalization for any reason and all-cause mortality, each of which was assessed 30 days and 1 year after the discharge date of the index HF hospitalization. Re-hospitalizations were captured from the EMR. Deaths were identified from health plan databases, state death registries, and Social Security Administration Death Master files.
We collected inpatient, outpatient, and pharmacy utilization for up to 12 months after the index hospitalization, counting for each patient the total number of inpatient admissions, inpatient hospital days, emergency room visits, outpatient visits, and pharmaceutical dispenses (in 30-day increments, eg, a 90-day supply counted as 3 dispenses). Not all patients remained health plan members for the entire year of follow-up either because of mortality or disenrollment for other reasons, so we annualized each of these forms of utilization by dividing by months of eligibility and then multiplying by 12.
We compared baseline characteristics of patients with HFrEF versus HFpEF using simple t tests for continuous variables and the chi-square tests for dichotomous variables. To compare rates of re-hospitalization and mortality, we used generalized linear models with Poisson errors and the natural log of person-time as an adjustment for unequal follow-up, including adjustments for covariates. We compared annualized medical utilization using generalized linear models weighted by months of eligibility. These models were also adjusted for covariates and included an indicator variable for mortality within 1 year. All analyses were performed using SAS, version 9.3 (SAS Institute, Cary, North Carolina).
Results
Of the 5,847 patients, 38% (n = 2,205) had HFrEF and 62% (n = 3,631) had HFpEF ( Table 1 ). The crude prevalence of the 4 clinical outcomes of interest is compared in Table 2 . The incidence of re-hospitalization was not statistically significantly different between patients with HFrEF and HFpEF after adjustment for covariates at either 30 days or 1 year ( Figure 1 ). However, Figure 2 shows that patients with HFrEF had 39% greater adjusted mortality at 30 days. After adjustment for covariates including mortality, patients with HFpEF incurred significantly more annualized outpatient visits and emergency room visits compared with those with HFrEF, although the absolute differences were small ( Table 3 ). Inpatient utilization and pharmaceutical dispenses were nearly identical and not statistically significantly different between the 2 groups.
| Variable | HFrEF (n=2,205) | HFpEF (n=3,631) | P Value |
|---|---|---|---|
| Age (Years) | 71.4 ± 13.8 | 75.9 ± 12.3 | <0.001 |
| Men | 64% | 45% | <0.001 |
| Hispanic | 21% | 20% | 0.605 |
| Non-Hispanic Black | 19% | 14% | <0.001 |
| Non-Hispanic White/Other | 60% | 66% | <0.001 |
| Current Smoker | 11% | 6% | <0.001 |
| Pre-existing Heart Failure | 52% | 45% | <0.001 |
| Coronary Artery Disease | 40% | 36% | <0.001 |
| Diabetes Mellitus | 40% | 49% | <0.001 |
| Chronic Kidney Disease | 51% | 66% | <0.001 |
| Hypertension | 76% | 90% | <0.001 |
| Depression | 19% | 25% | <0.001 |
| Systolic Blood Pressure (mmHg) | 127 ± 16 | 133 ± 15 | <0.001 |
| Diastolic Blood Pressure (mmHg) | 71 ± 11 | 68 ± 9 | <0.001 |
| Length of Stay of Index Hospitalization (Days) | 4.0 ± 3.2 | 3.8 ± 3.2 | 0.064 |
| Outcome | HFrEF (n=2,205) | HFpEF (n=3,631) | P Value |
|---|---|---|---|
| Re-Hospitalization | |||
| Within 30 Days | 429 (20%) | 688 (19%) | 0.633 |
| Within 1 Year | 1,203 (55%) | 2,107 (58%) | 0.010 |
| All-Cause Mortality | |||
| Within 30 Days | 133 (6%) | 187 (5%) | 0.151 |
| Within 1 Year | 534 (24%) | 836 (23%) | 0.297 |