Radial access coronary procedures are associated with fewer access site complications compared to femoral access. There is controversy regarding greater radiation exposure to patient and operator using radial access. We aimed to compare radiation dose during coronary procedures for the 2 access routes and assess the effect of operator experience with radial access on radiation dose. Fluoroscopy time (FT) and dose–area product (DAP) were recorded for all radial access and femoral access procedures during default femoral access, transition phase (femoral access and early radial access), and default radial access. Femoral access cases (n = 848, 412 diagnostic, 436 percutaneous coronary interventions [PCIs]) and radial access cases (n = 965, 459 diagnostic, 506 PCIs) were assessed. For diagnostics, median FT for radial access was longer than for femoral access (4.43 minutes, interquartile range [IQR] 2.55 to 8.18, vs 2.34 minutes, IQR 1.49 to 4.18, p <0.001) and associated with larger DAP (radial access 1,837 μGy·m 2 , IQR 1,172 to 2,783, vs femoral access 1,657 μGy·m 2 , IQR 1,064 to 2,376, p <0.001). For PCI, FT was longer for radial access (median 12.02 minutes, IQR 7.57 to 17.54, vs femoral access 9.36 minutes, IQR 6.13 to 14.27, p <0.001)—this did not translate into an increased DAP (femoral access median 3,392 μGy·m 2 , IQR 2,139 to 5,193, vs radial access 3,682 μGy·m 2 , IQR 2,388 to 5,314, p = NS). For diagnostic radial access, FT decreased from the transition phase (n = 134) to the default radial access phase (n = 323, 5.12 minutes, IQR 3.07 to 9.40, vs 4.21 minutes, IQR 2.49 to 7.52, p = 0.03). This was not observed for PCI. In conclusion, transition from femoral access to radial access for diagnostics and PCI increased FT. DAP increased for diagnostic radial access but not PCI compared with femoral access. FTs for radial access diagnostic cases decreased with experience.
Transradial coronary procedures have been shown to have fewer access-site complications compared to the transfemoral approach and is preferred by patients. There is controversy with respect to quantity of radiation delivered to patient and operator using the transradial approach. There are recent reports of increased radiation exposure when using the radial arterial approach. Factors such as imaging system used and operator experience and stage on the “learning curve” may influence radiation dose delivered, but these effects have not been fully elucidated. We have looked at cases across a period when our high-volume practice has transitioned from default transfemoral access through to default transradial access. We compared fluoroscopy time (FT), dose–area product (DAP), and contrast agent delivery between the 2 access routes for diagnostic procedures and for percutaneous coronary intervention (PCI). We also assessed the influence of operator experience and the effect of a learning curve on these radiation variables.
Methods
The study was completed in the Belfast City Hospital (Belfast, Northern Ireland)—a high-volume tertiary cardiology center (1,400 PCIs/year) with 5 cardiologists experienced in femoral access cardiac catheterization (>2,000 diagnostic studies) and coronary interventions (>1,000 PCIs). All practitioners have been fully trained in the principles of radiation protection in accordance with mandatory regulations. Data were recorded retrospectively from studies in 1 catheterization laboratory only. The imaging system used was Siemens Axiom Artis dFC (Siemens, Erlangen, Germany) installed in 2005 and serviced biannually. Fluoroscopic settings were 7.5 pulses/s and cinematic acquisition imaging frame rates were set at 10 frames/s for coronary images and 15 frames/s for left ventricular angiography. Iontomat (Siemens) automatic exposure control was used. Images were acquired in the standard manner with the assistance of an experienced radiographer and adhering to United Kingdom ionizing radiation medical exposure regulations. Standard operator shielding (lead aprons, lead thyroid collar, lead spectacles, transparent 1.0-cm lead screening between operator and patient) was used throughout. Most operators exchanged catheters over the wire for radial access but not for femoral access. No identifying patient data were collected.
Three specified periods were studied: January 1 to April 1, 2007, using the default femoral access approach; January 1 to July 1, 2008, with some operators continuing with femoral access and other operators beginning to use radial access (transition phase); and January 1 to July 1, 2009, with all operators deferring to radial access as the first choice (default radial approach).
Data recorded for all studies within the defined periods were body mass index (BMI; kilograms per meter squared), access site (femoral or radial artery), procedure complexity (diagnostic angiography or coronary intervention), FT (minutes; has some influence on radiation dose delivered and is an indicator of procedure duration), DAP (micrograys meter squared; reflects radiation dose delivered to patient during fluoroscopy and cinematic image acquisition), and volume of contrast used. The studies consisted of elective and emergency procedures and included complex PCI cases. Because operator experience in femoral access cases was unlikely to be a factor in radiation dose delivery, all femoral access cases were analyzed together regardless of period. Numbers were sufficient for comparison with radial cases using 3 months for the default femoral period.
All analyses were performed using SPSS 11 for Windows (SPSS, Inc., Chicago, Illinois). Continuous normally distributed variables are reported as mean ± 1 SD; median and interquartile range (IQR) are quoted for data of skewed distribution. Nonparametric correlations were assessed with Spearman rank correlation. Proportions were compared using Pearson chi-square test. Means were compared using Student’s t test or analysis of variance and Mann-Whitney U test or Kruskal-Wallis tests were performed to compare data of non-normal distribution. A p value <0.05 was statistically significant.
Results
In total 1,813 cases were studied—848 with femoral access and 965 with radial access. Table 1 presents the distribution of cases across the 3 phases of transition. There was a progressive increase in radial access with time. Similar proportions of diagnostic angiographies and PCIs were performed in each period. Overall mean BMI was 29 ± 5 kg/m 2 ; BMI correlated with DAP (Spearman rank correlation coefficient 0.42, p <0.001). Neither FT nor contrast use correlated with BMI.
| Variable | Default Femoral Phase | Transition Phase | Default Radial Phase | p Value |
|---|---|---|---|---|
| (n = 340) | (n = 685) | (n = 788) | ||
| Body mass index (kg/m 2 ), mean ± SD | 29 ± 5 | 29 ± 5 | 30 ± 6 | 0.04 ⁎ |
| Access | <0.001 † | |||
| Femoral | 340 (100%) | 405 (59%) | 103 (13%) | |
| Radial | 0 | 280 (41%) | 685 (87%) | |
| Diagnostic angiography | 171 (50%) | 330 (48%) | 370 (47%) | 0.64 † |
| Percutaneous coronary intervention | 169 (50%) | 355 (52%) | 418 (53%) |
Analyzing all femoral cases together (412) and all radial cases together (459), for diagnostic angiography ( Figures 1 and 2 ) , BMI was greater in the radial access group (30 ± 6 kg/m 2 ) compared to the femoral access group (29 ± 5 kg/m 2 , p = 0.03). Radial access was associated with a longer FT (4.43 minutes, IQR 2.55 to 8.18) and larger DAP (1,837 μGy·m 2 , IQR 1,172 to 2,783) compared to femoral access (FT 2.34 minutes, IQR 1.49 to 4.18, DAP 1,657 μGy·m 2 , IQR 1,064 to 2,376, p <0.001). Before correction for BMI, radial access was associated with a 70% (95% confidence interval [CI] 54 to 89) increase in FT and a 20% (95% CI 10 to 31) increase in DAP compared to femoral access. After correction for BMI by analysis of covariance the increase in FT (70%, 95% CI 53 to 88) and DAP (14%, 95% CI 6 to 23) remained significant. Contrast volumes used were similar (radial access 100 ml, IQR 90 to 130, femoral access 100 ml, IQR 90 to 130, p = 0.30).
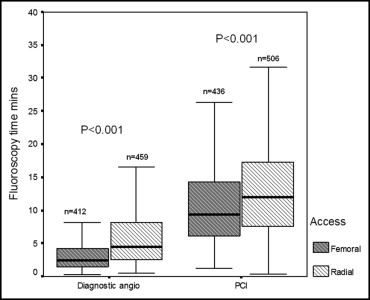
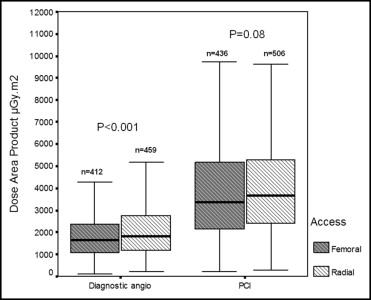
Analyzing all femoral cases together (436) and all radial cases together (506) for PCI ( Figures 1 and 2 ), BMI was similar between groups (radial 29 ± 5 vs femoral 29 ± 5 kg/m 2 , p = 0.85). FT was longer in the radial access group (12.02 minutes, IQR 7.57 to 17.54) compared to the femoral access group (9.36 minutes, IQR 6.13 to 14.27, p <0.001). This did not translate into significantly greater DAP (radial access DAP 3,682 μGy·m 2 , IQR 2,388 to 5,314, vs femoral access DAP 3,392 μGy·m 2 , IQR 2,139 to 5,193, p = 0.08). Contrast volumes used were similar (radial access 193 ml, IQR 150 to 240, femoral access 190 ml, IQR 150 to 240, p = 0.53).
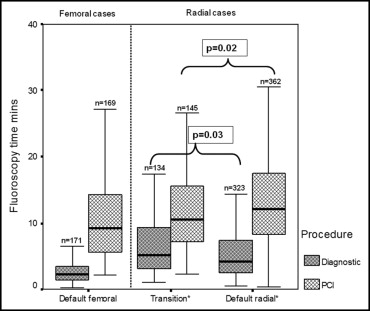
To test the effect of increased operator experience and to assess the duration of any learning curve, radiation variables from radial access cases during the transition phase were compared to radial cases from the subsequent default radial phase ( Figures 3 and 4 ). For diagnostic procedures FT during the transition phase was 5.12 minutes (IQR 3.07 to 9.40) and decreased during the default radial phase to 4.21 minutes (IQR 2.49 to 7.52, p = 0.03). This was not associated with a decrease in DAP. BMI and contrast volume used did not change (transition phase BMI 29 ± 5 vs default radial phase BMI 30 ± 7 kg/m 2 , p = 0.14; transition phase contrast use 100 ml, IQR 90 to 130, vs default radial phase 100 ml, IQR 90 to 130, p = 0.95).