The efficacy of primary percutaneous coronary intervention (PPCI) has been documented in several randomized-controlled trials. We sought to examine the clinical outcome after PPCI of real-world patients eligible and ineligible for inclusion in a randomized trial (DANAMI-2) and to compare it to the outcome of the DANAMI-2 population. We did a population-based follow-up study comparing 1,320 consecutive real-world patients treated with PPCI from 2004 to 2006 to 686 patients treated with PPCI in the DANAMI-2 trial. By reviewing medical records we determined whether the real-world patients were eligible in the DANAMI-2 trial. The real-world population had a more adverse baseline risk profile. Cumulative incidences of the composite end point of all-cause mortality, reinfarction, and stroke after 1 year and 2 years were 17.8% and 22.0%, respectively, in the real-world population compared to 13.6% and 17.3% in the DANAMI-2 population. After adjustment for differences in baseline characteristics and treatment, differences persisted after 1 year (adjusted hazard ratio 1.8, 95% confidence interval 1.3 to 2.6) and 2 years (adjusted hazard ratio 1.7, 95% confidence interval 1.2 to 2.3). Results for the real-world patients eligible according to DANAMI-2 criteria were comparable to the results from the DANAMI-2 trial. In conclusion, real-world patients had a more adverse baseline prognostic profile and a poorer clinical outcome compared to the DANAMI-2 patients. However, clinical outcome in the real-world patients eligible in the DANAMI-2 trial was comparable to that for the DANAMI-2 patients after invasive and medical treatment.
To our knowledge, a direct comparison of unselected patients treated with primary percutaneous coronary intervention (PPCI) versus those enrolled in a trial has not been performed. We therefore conducted a follow-up study comparing characteristics, treatment, and outcome after PPCI between real-world patients treated after widespread implementation of PPCI and those in the Danish Multicenter Randomized Study on Thrombolytic Therapy versus Acute Coronary Angioplasty in Acute Myocardial Infarction (DANAMI-2) population to assess whether it is possible to achieve trial results in real-world settings.
Methods
We completed a population-based historical follow-up study in the central Denmark region (approximately 1.2 million). The National Health Service provides tax-supported health care for all inhabitants, allowing free access to general practitioners and hospitals. All acute medical conditions, including ST-elevation myocardial infarction, are exclusively treated at public hospitals in Denmark. Each Danish citizen receives a unique identification number at birth that encodes gender and date of birth and allows accurate linkage among public registries.
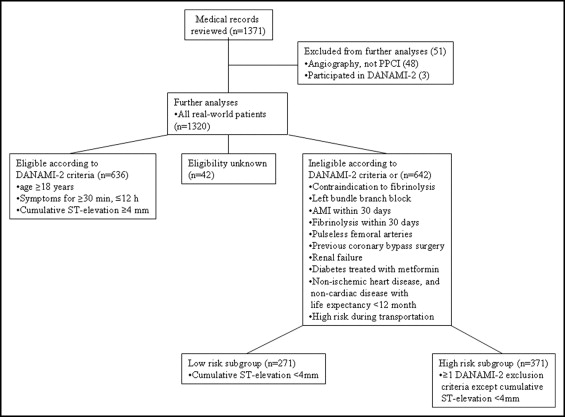
The Western Denmark Heart Registry (WDHR) collects detailed patient- and procedure-related data for all interventions carried out in western Denmark since 1999. We identified all PPCIs performed at Aarhus University Hospital (Skejby, Denmark), which serves the central Denmark region, from April 2004 to December 2006 (n = 1,371; Figure 1 ). Medical records were reviewed. We determined whether patients fulfilled criteria for eligibility in the DANAMI-2 trial or met 1 of the exclusion criteria. The first author reviewed all records. If it was uncertain whether the electrocardiogram fulfilled the inclusion criteria, a consultant in cardiology (TN) reviewed them, and an agreement was reached. Based on data from the patient records, the real-world population was divided into subgroups according to whether they fulfilled the criteria for eligibility in the DANAMI-2 trial. Patients ineligible for the DANAMI-2 trial were further divided into high-risk and low-risk subgroups.
The DANAMI-2 trial was conducted from December 1997 to October 2001. Patients were enrolled from 24 referral hospitals without angioplasty facilities and 5 invasive-treatment hospitals with such facilities. Of 4,278 screened patients, 1,572 (37%) were included in the study and randomly assigned to fibrinolysis at the referral hospital or PPCI at an invasive-treatment hospital. The primary end point was a composite end point of death, reinfarction, and stroke at 30 days. Of the 790 patients randomly assigned to PPCI, balloon inflation was performed in 686 patients (87%). The DANAMI-2 population in our study consisted of these 686 patients.
The National Patient Registry, established in 1977, collects data for all nonpsychiatric hospitalizations at Danish hospitals, including dates of admission and discharge and up to 20 discharge diagnoses assigned by the treating physician and coded according to the International Classification of Diseases, 10th Revision , since 1993. In the 2 patient groups data on previous health status was obtained from the registry. Based on the complete hospitalization history of each patient, we computed the Charlson Comorbidity Index score. The Charlson Comorbidity Index has been validated for the prediction of mortality for patients with a wide range of conditions and has been adapted and validated for use with hospital discharge registry data. We defined 3 levels of co-morbidity: 0 co-morbidity (“none”) for patients with no recorded underlying diseases included in the Charlson Comorbidity Index; a score of 1 to 2 (“low co-morbidity”); and a score >2 (“high co-morbidity”).
We obtained data on use of cardiovascular drugs by real-world patients from population-based prescription databases. These databases contain information on all redeemed prescriptions for reimbursable drugs dispensed from all pharmacies in the central Denmark region. Information includes type of drug according to the anatomic therapeutic chemical classification system and date dispensed. We identified all prescriptions for antiplatelet drugs, nitroglycerin, statins, angiotensin-converting enzyme inhibitors, angiotensin II receptor antagonists, and selective and nonselective β blockers filled within 90 days, 1 year and 2 years after hospital discharge. All drugs are available only by prescription, except for aspirin. However, aspirin is also available by prescription, and patients with chronic diseases and pensioners are reimbursed for it. Data on use of cardiovascular drugs in the DANAMI-2 population were obtained from the DANAMI-2 database except for data on clopidogrel, which were obtained from prescription databases.
Data on location of the culprit lesion, number of diseased vessels, and type and number of stents used were obtained from the WDHR and the DANAMI-2 database.
The primary end point was a composite end point of all-cause mortality, reinfarction, and stroke at 30 days and at 1 year and 2 years. Secondary end points were all-cause mortality, reinfarction, stroke, and target vessel revascularization (TVR) at 30 days and at 1 year and 2 years. Admission with myocardial infarction within 28 days of the index infarction was not regarded as a new event according to the World Health Organization MONICA definition. TVR was defined as a repeated PCI on the index vessel or coronary artery bypass grafting.
Data on reinfarction and stroke were obtained from the National Patient Registry, and deaths were ascertained from the Danish Civil Registration System, which has kept records on changes in vital status of the entire Danish population since 1968. Data on TVR were obtained from the WDHR and the DANAMI-2 database.
Patients were censored at the time of death or followed up for 2 years. We compared baseline characteristics of the real-world population to the DANAMI-2 population using Student’s t test for continuous variables and chi-square test for categorical variables. We used Cox proportional hazards regression to compute crude and adjusted hazard ratios and 95% confidence intervals for the end points. The DANAMI-2 population served as the reference in all analyses. We included covariates in multivariable analyses using the “change-in-estimate” method and retained only covariables that changed the hazard ratio for an outcome by >10%. The final models included gender, age, duration of symptoms, smoking status, type of stent (drug-eluting/bare metal), periprocedural use of glycoprotein IIb/IIIa inhibitor, and use of aspirin, clopidogrel, statins, and β blockers after 1 year. All tests of significance were 2-tailed with a p value <0.05 considered statistically significant.
The number of patients with no missing data was 1,164. Of the 30 covariates listed in Tables 1 and 2 , data were missing in 18, ranging from 1% to 9%, except for clopidogrel in which 15.5% were missing. To account for missing values of these covariates, a multiple imputation strategy was applied. All variables in Tables 1 and 2 and the combined end point were included in the imputation model. Factors known to influence the occurrence of missing data were also included (i.e., real-world patient/DANAMI-2 patient). We also included the logarithm of the survival time, as recommended by van Buuren et al. Imputation and subsequent analyses were conducted using the ice and micombine procedures in STATA 10.0 (STATA Corp., College Station, Texas). Analyses were carried out on 5 imputed datasets and the results combined appropriately using the rules of Rubin.
| Variable | Real World, All (n = 1,320) | Real World, Eligible (n = 636) | Real-World, Not Eligible, High Risk (n = 371) | Real-World, Not Eligible, Low Risk (n = 271) | DANAMI-2 (n = 686) |
|---|---|---|---|---|---|
| Age (mean) | 65.2 (64.5–65.9) † | 65.0 (64.0–66.0) ⁎ | 65.9 (64.7–67.1) † | 64.2 (62.7–65.8) | 63.1 (62.2–64.0) |
| Male gender (%) | 978/1,320 (74.1%) | 471/636 (74.1%) | 281/371 (75.7) | 200/271 (73.8%) | 508/686 (74.0%) |
| Co-morbidity | |||||
| None | 784/1,320 (59.4%) † | 403/636 (63.4%) | 197/371 (53.1%) ‡ | 161/271 (59.4%) ⁎ | 463/686 (67.5%) |
| Low | 396/1,320 (30.0%) | 171/636 (26.9%) | 122/371 (32.9%) ⁎ | 88/271 (32.5%) | 185/686 (27.0%) |
| High | 140/1,320 (10.6%) † | 62/636 (9.7%) ⁎ | 52/371 (14.0%) ‡ | 22/271 (8.1%) | 38/686 (5.5%) |
| Previous myocardial infarction | 164/1,320 (12.4%) ⁎ | 62/636 (9.7%) | 48/371 (12.9%) | 46/271 (17.0%) † | 63/686 (9.2%) |
| Previous heart failure | 55/1,320 (4.2%) ⁎ | 24/636 (3.8%) | 20/371 (5.4%) ⁎ | 9/271 (3.3%) | 15/686 (2.2%) |
| Previous cerebrovascular disease | 113/1,320 (8.6%) ⁎ | 43/636 (6.7%) | 45/371 (12.1%) † | 20/271 (7.4%) | 38/686 (5.5%) |
| Previous peripheral vascular disease | 85/1,320 (6.4%) | 34/636 (5.3%) | 30/371 (8.1%) ⁎ | 20/271 (7.4%) | 31/686 (4.5%) |
| Diabetes mellitus | 118/1,310 (9.0%) | 42/633 (6.6%) | 55/366 (15.0%) ‡ | 15/269 (5.6%) | 49/686 (7.1%) |
| Moderate/severe renal disease | 30/1,320 (2.3%) | 9/636 (1.4%) | 14/371 (3.8%) ⁎ | 6/271 (2.2%) | 8/686 (1.2%) |
| Any tumor | 101/1,320 (7.7%) ⁎ | 58/636 (9.1%) ⁎ | 27/371 (7.3%) | 14/271 (5.2%) | 33/686 (4.8%) |
| Coronary heart disease in family | 455/1,200 (37.9%) | 230/597 (38.5%) | 101/308 (32.8%) | 112/260 (43.1%) | 250/664 (37.7%) |
| Smoker | |||||
| Never | 287/1,197 (24.0%) ⁎ | 143/602 (23.8%) | 77/301 (25.6%) ⁎ | 54/258 (20.9%) | 133/677 (19.7%) |
| Previous | 270/1,197 (22.6%) | 126/602 (20.9%) | 78/301 (25.9%) | 61/258 (23.6%) | 146/677 (21.6%) |
| Active | 640/1,197 (53.5%) ⁎ | 333/602 (55.3%) | 146/301 (48.5%) ⁎ | 143/258 (55.4%) | 398/677 (58.8%) |
| Hypertension | 370/1,225 (30.2%) ‡ | 164/607 (27.0%) ‡ | 107/317 (33.8%) ‡ | 84/263 (31.9%) † | 137/682 (20.1%) |
| Duration of symptoms (hours) | 4.4 (4.2–4.6) ‡ | 3.5 (3.4–3.7) ⁎ | 7.5 (6.7–8.4) ‡ | 4.1 (3.9–4.4) | 3.8 (3.7–4.0) |
| Patient delay | 1.4 (1.3–1.5) ‡ | 1.2 (1.0–1.3) ‡ | 2.1 (1.7–2.7) ‡ | 1.3 (1.2–1.5) ‡ | 0.8 (0.7–0.9) |
| Admission delay | 1.4 (1.3–1.4) ‡ | 1.1 (1.1–1.2) ‡ | 2.0 (1.8–2.2) ‡ | 1.3 (1.2–1.4) ‡ | 0.7 (0.7–0.8) |
| Variable | Real World, All (n = 1,320) | Real World, Eligible (n = 636) | Real World, Not Eligible, High Risk (n = 371) | Real World, Not Eligible, Low Risk (n = 271) | DANAMI-2 (n = 686) |
|---|---|---|---|---|---|
| Door-to-balloon time | 0.67 (0.65–0.69) | 0.61 (0.59–0.64) | 0.72 (0.67–0.78) ⁎ | 0.74 (0.69–0.80) ⁎ | 0.65 (0.61–0.68) |
| Number of narrowed coronary arteries | |||||
| 0 | 26/1,242 (2.1%) ⁎ | 13/604 (2.2%) ⁎ | 8/351 (2.3%) ⁎ | 5/251 (2.0%) ⁎ | 2/686 (0.3%) |
| 1 | 627/1,242 (50.5%) ⁎ | 322/604 (53.3%) | 161/351 (45.9%) † | 123/251 (49.0%) ⁎ | 397/686 (57.9%) |
| 2 | 343/1,242 (27.6%) | 163/604 (27.0%) | 101/351 (28.8%) | 70/251 (27.9%) | 184/686 (26.8%) |
| 3 | 246/1,242 (19.8%) ⁎ | 106/604 (17.5%) | 81/351 (23.1%) ⁎ | 53/251 (21.1%) ⁎ | 103/686 (15.0%) |
| Sited culprit lesion | |||||
| Left main coronary artery | 15/1,283 (1.2%) | 5/617 (0.8%) | 8/359 (2.2%) ⁎ | 2/265 (0.8%) | 4/686 (0.6%) |
| Left anterior descending coronary artery | 597/1,283 (46.5%) | 344/617 (55.8%) ⁎ | 170/359 (47.4%) | 58/265 (21.9%) ‡ | 333/686 (48.5%) |
| Left circumflex coronary artery | 212/1,283 (16.5%) ⁎ | 82/617 (13.3%) | 63/359 (17.5%) ⁎ | 61/265 (23.0%) † | 86/686 (12.5%) |
| Right coronary artery t | 459/1,283 (35.8%) | 186/617 (30.1%) ⁎ | 118/359 (32.9%) | 144/265 (54.3%) ‡ | 263/686 (38.3%) |
| Stent implantation | 1,210/1,320 (91.7%) | 583/636 (91.7%) | 340/371 (91.6%) | 246/271 (90.8%) | 638/686 (93.0%) |
| Number of stents | |||||
| 0 | 110/1,320 (8.3%) | 53/636 (8.3%) | 31/371 (8.4%) | 25/271 (9.2%) | 48/686 (7.0%) |
| 1 | 922/1,320 (69.8%) | 451/636 (70.9%) | 253/371 (68.2%) | 187/271 (69.0%) | 496/686 (72.4%) |
| 2 | 218/1,320 (16.5%) | 104/636 (16.4%) | 62/371 (16.7%) | 45/271 (16.6%) | 121/686 (17.6%) |
| 3 | 53/1,320 (4.0%) | 24/636 (3.8%) | 16/371 (4.3%) | 11/271 (4.1%) | 18/686 (2.6%) |
| ≥4 | 17/1,320 (1.3%) | 4/636 (0.6%) | 9/371 (2.4%) ⁎ | 3/271 (1.1%) | 3/686 (0.4%) |
| Drug-eluting stents | 633/1,170 (54.1%) ‡ | 278/566 (49.1%) ‡ | 201/328 (61.3%) ‡ | 131/236 (55.5%) ‡ | 0 |
| Bare metal stents | 537/1,170 (45.9%) ‡ | 288/566 (50.9%) ‡ | 127/328 (38.7%) ‡ | 105/236 (44.5%) ‡ | 636/636 (100%) |
| Glycoprotein IIb/IIIa during primary percutaneous coronary intervention | 1,065/1,317 (80.9%) ‡ | 539/635 (84.9%) ‡ | 263/369 (71.3%) ‡ | 227/271 (83.8%) ‡ | 302/686 (44.0%) |
| Clopidogrel 1 year | 1,166/1,303 (89.5%) ‡ | 587/629 (93.3%) ‡ | 301/366 (82.2%) ‡ | 241/266 (90.6%) ‡ | 178/392 (45.4%) |
| Statin 1 year | 1,134/1,303 (87.0%) ‡ | 561/628 (89.3%) ‡ | 301/367 (82.0%) ‡ | 237/266 (89.1%) ‡ | 424/619 (68.5%) |
| β blocker 1 year | 1,111/1,301 (85.4%) | 552/627 (88.0%) ⁎ | 290/366 (79.2%) | 231/266 (86.8%) | 509/619 (82.2%) |
| Nitroglycerin 1 year | 558/1,258 (44.4%) ‡ | 261/599 (43.6%) ‡ | 152/359 (42.3%) ‡ | 128/258 (49.6%) ‡ | 65/619 (10.5%) |
| Aspirin 1 year | 1,184/1,304 (90.8%) ‡ | 584/627 (93.1%) ⁎ | 318/368 (86.4%) ‡ | 243/267 (91.0%) † | 598/619 (96.6%) |
| Angiotensin-converting enzyme inhibitor/angiotensin II receptor antagonist | 776/1,280 (60.6%) ‡ | 377/612 (61.6%) ‡ | 240/363 (66.1%) ‡ | 130/263 (49.4%) ⁎ | 232/619 (37.5%) |
We analyzed data using STATA 10.0. Our study was approved by the Danish Data Protection Agency (journal number 2008-41-1835).
Results
Of the total study population of 2,006 patients, follow-up data were missing for 1 patient from the real-world population. Of the 1,320 real-world patients, 636 (48.2%) fulfilled the DANAMI-2 inclusion criteria, 642 (48.6%) did not, and in 42 patients (3.2%), there was insufficient information to determine whether they fulfilled the criteria. Contraindications for fibrinolysis were present in 32 patients; 229 patients had a prehospital delay >12 hours; 48 patients had left bundle branch block; 465 did not fulfill the electrocardiographic criteria; and in 208 patients, another exclusion criterion was present. Patients ineligible according to DANAMI-2 criteria consisted of 371 high-risk patients (28.1%) and 271 low-risk patients (20.5%).
Tables 1 and 2 present patient, procedural, and medical treatment characteristics of real-world and DANAMI-2 patients. Compared to DANAMI-2 patients, real-world patients were older and had a higher prevalence of previous myocardial infarction, congestive heart failure, cerebrovascular disease, tumors, and hypertension. In contrast, there were fewer smokers in real-world patients. Time from symptom onset to revascularization was longer in real-world patients, and more patients had a nonpathological angiogram or 3-vessel disease. The left circumflex artery was more often the culprit lesion in the real-world group. There were no differences in the number of stents used, but a larger proportion of real-world patients had a drug-eluting stent implanted. A larger proportion of the real-world population used cardiovascular medications after 1 year, except for aspirin.
In contrast, real-world patients eligible according to DANAMI-2 criteria did not differ from the DANAMI-2 population regarding prevalence of previous myocardial infarction, congestive heart failure, cerebrovascular disease, 1- and 3-vessel disease, culprit lesion in the left circumflex artery, and smoking status. In addition, these patients had a shorter time from symptom onset to revascularization, their culprit lesion was more often located in the left anterior descending artery, and a larger proportion used β blockers compared to the DANAMI-2 population.
In the high-risk subgroup of patients ineligible according to DANAMI-2 criteria, prevalences of peripheral vascular disease, diabetes, and renal insufficiency were higher than in the DANAMI-2 group. The culprit lesion was more often located in the left main artery or left circumflex artery, and a larger proportion of patients had ≥4 stents implanted.
The low-risk subgroup of patients ineligible according to DANAMI-2 criteria had a higher prevalence of previous myocardial infarction, and the culprit lesion was more often located in the right coronary artery or left circumflex artery.
Table 3 presents clinical outcomes for the populations. In a comparison between the entire real-world population and the DANAMI-2 population, cumulative risks of the composite end point after 1 year and 2 years were 17.8% and 22.0%, respectively, in the real-world population compared to 13.6% and 17.3% in the DANAMI-2 population. These differences remained after adjustment. The difference was primarily the result of higher mortality and a higher incidence of stroke in the real-world population after 1 year and 2 years. There was no difference in the incidence of reinfarction and TVR.



