Left main coronary artery (LMCA) percutaneous coronary intervention (PCI) has emerged as an appealing alternative to bypass surgery for significant LMCA disease, especially in high-risk candidates. PCI for unprotected LMCA stenosis is currently designated a class IIb indication. Direct comparisons between unprotected LMCA PCI and multivessel PCI are lacking. We aimed to determine the incremental risk associated with unprotected LMCA PCI compared to multivessel PCI. We queried the Cleveland Clinic PCI database to identify patients who underwent unprotected LMCA PCI from 2003 through 2009 and compared these to patients undergoing multivessel PCI in the same period. Patients undergoing PCI for acute myocardial infarction were excluded. Mortality was derived using the Social Security Death Index. Short-term (≤30-day) mortality rates in the LMCA PCI group (n = 468, 1.9%) were similar to the death rate in the multivessel PCI group (n = 1,973, 1.3%, p = 0.3). There was no significant difference in adjusted mortality between the 2 study groups. Stratifying LMCA PCI by the number of concomitant vessel territories treated, there was no significant difference in mortality in any LMCA PCI category (LMCA only, LMCA + 1-vessel PCI, LMCA + multivessel PCI) compared to multivessel PCI. In conclusion, there was comparable short-term and long-term mortality in the LMCA PCI and multivessel PCI groups. LMCA stenting did not appear to incur incremental risk compared to multivessel PCI.
Multivessel percutaneous coronary interventions (PCIs) are commonly performed in the current era of drug-eluting stent (DES) interventions. Multivessel PCI has a class II indication for revascularization in the most recent American College of Cardiology/American Heart Association guidelines for stable or unstable angina pectoris. Multivessel PCI could serve as a comparison group for left main coronary artery (LMCA) PCI for procedural and postprocedural outcomes. We aimed to calculate the short- and long-term incremental risks associated with LMCA PCI compared to multivessel coronary PCI.
Methods
The study population was obtained from the prospective PCI database maintained by trained research staff at the Cleveland Clinic. All patients who underwent an index PCI procedure on an unprotected LMCA with a bare-metal stent (BMS) or DES from March 1, 2003 through July 31, 2009 were included. Unprotected LMCA was defined as an LMCA trunk devoid of any patent bypass grafts to the left anterior descending or left circumflex coronary artery or any of their downstream branches. These patients undergoing LMCA PCI were compared to all those who underwent concomitant PCI on ≥2 major vessel territories excluding the LMCA. Patients undergoing PCI for acute ST-segment elevation myocardial infarction were excluded from the study. The study protocol was approved by the Cleveland Clinic institutional review board.
We queried the database for baseline characteristics, cardiac history, risk factors, European System for Cardiac Operative Risk Evaluation score, angiographic and procedural data and extensive data about each lesion’s morphologic characteristics including Synergy between PCI with Taxus and cardiac surgery trial (SYNTAX) score, lesion length, eccentricity, tortuosity, calcification, percent stenosis, Thrombolysis In Myocardial Infarction flow grade, and characteristics of totally occluded lesions and lesions around bifurcations/trifurcations. Treatment characteristics retrieved from the database included stent type, device diameter, device length, postprocedural stenosis, and final Thrombolysis In Myocardial Infarction flow. The primary outcome was long-term all-cause mortality, which was determined using the Social Security Death Index. Secondary outcomes included direct procedure-related events including 30-day mortality, postprocedure myocardial infarction, shock, congestive heart failure, arrhythmias, renal failure, respiratory failure, and bleeding complications. Postprocedure acute myocardial infarction was defined as an increase in creatine kinase-MB to >3 times the upper limit of normal (8.8 ng/ml).
All statistical analyses were performed using STATA 10.0 (STATA Corporation, College Station, Texas). Continuous variables are presented as mean ± SD and categorical variables are presented as proportions. Comparisons between the 2 study groups were drawn using Student’s t test for continuous variables and chi-square test for categorical variables. All statistical tests were 2-tailed and a p value <0.05 was considered statistically significant. Unadjusted survival analysis comparing LMCA PCI to multivessel PCI was conducted using the Kaplan–Meier method, and statistical comparisons were drawn using log-rank test. Adjusted survival analysis was carried out using 2 strategies. The first strategy involved use of nonparsimonious semiparametric Cox proportional hazard modeling. In this modeling approach, we used patient-level data such as demographics, clinical characteristics, cumulative patient SYNTAX score, and logistic European System for Cardiac Operative Risk Evaluation score as covariates. Cox proportional hazard modeling requires data to be organized such that each patient or unit constitutes a single row in the datasheet. Statistical mechanisms that account for an unstructured clustering in the dataset are lacking in this type of regression method. Because of restriction to patient-level data only in this modeling strategy, it was not possible to incorporate angiographic parameters for each lesion into these regression models.
The second strategy involved use of generalized estimating equations with robust SEs. For this modeling strategy, each lesion and its corresponding intervention were treated as the smallest unit for statistical analysis. Organizing data in this fashion allowed us to incorporate individual lesion and morphologic characteristics, interventional data, and postprocedure characteristics into the regression model. Regression models were designed in 2 discrete ways: the first set of regression models incorporated pre- and postprocedure characteristics, and the second set included only preprocedural characteristics. The second set of regression models was primarily constructed to determine the predictive role of preprocedural characteristics in determination of long-term mortality.
Data were analyzed as “clustered data” with multiple lesions in the same patient being treated as a single cluster. An autoregressive correlation structure was used to account for the cluster structure because measurements taken through time in the same patient were assumed to be highly correlated if spaced more closely in time.
Results
In total 468 patients underwent LMCA PCI and 1,973 patients underwent multivessel PCI from March 1, 2003 through July 31, 2009 at our institution. Baseline characteristics of the study population are listed in Table 1 . Patients undergoing LMCA PCI were significantly older compared to the control population. Prevalences of hypertension, previous congestive heart failure and acute myocardial infarction, peripheral vascular disease, chronic renal failure, and New York Heart Association class III or IV symptoms were significantly higher in the LMCA PCI group. In addition, mean preprocedural left ventricular ejection fraction in the LMCA PCI group was significantly lower compared to the multivessel PCI group. Mean ± SD follow-up durations in the LMCA PCI group and multivessel PCI group were 2.8 ± 1.7 and 3.4 ± 1.6 years, respectively. Table 2 presents differences in distribution of patients according to duration of follow-up.
| Characteristic | LMCA PCI (n = 468) | Multivessel PCI (n = 1,973) | p Value |
|---|---|---|---|
| Age (years), mean ± SD | 69 ± 11 | 65 ± 11 | <0.001 |
| Men | 338 (72.2%) | 1,400 (71.0%) | 0.6 |
| White | 435 (93.0%) | 1,695 (85.9%) | <0.001 |
| Black | 22 (4.7%) | 185 (9.4%) | <0.001 |
| Other races | 11 (2.3%) | 93 (4.7%) | <0.001 |
| Body mass index (kg/m 2 ), mean ± SD | 29.1 ± 6.2 | 30.2 ± 6.4 | <0.001 |
| Hypertension | 410 (87.6%) | 1,627 (82.5%) | 0.007 |
| Dyslipidemia | 439 (93.8%) | 1,802 (91.3%) | 0.08 |
| Stroke | 42 (9.0%) | 143 (7.3%) | 0.2 |
| Diabetes mellitus | 175 (37.4%) | 765 (38.8%) | 0.6 |
| Previous heart failure | 102 (21.8%) | 273 (13.8%) | <0.001 |
| Peripheral vascular disease | 122 (26.1%) | 268 (13.6%) | <0.001 |
| Chronic obstructive pulmonary disease | 93 (19.9%) | 268 (13.6%) | 0.001 |
| Smoker | |||
| Never | 125 (26.7%) | 669 (33.9%) | <0.001 |
| Former | 300 (64.1%) | 1,027 (52.1%) | <0.001 |
| Current | 43 (9.2%) | 277 (14.0%) | <0.001 |
| Previous myocardial infarction | 205 (44.2%) | 729 (37.3%) | 0.006 |
| Chronic renal failure | 49 (10.5%) | 102 (5.2%) | <0.001 |
| Preprocedure ejection fraction (%), mean ± SD ⁎ | 48 ± 14 | 51 ± 12 | <0.001 |
| Preprocedure New York Heart Association class 3/4 | 169 (36.1%) | 499 (25.3%) | <0.001 |
| EuroSCORE predicted mortality, mean ± SD | 15.7 ± 15.1 | 7.7 ± 10.1 | <0.001 |
| SYNTAX score, mean ± SD | 18.4 ± 8.9 | 11.1 ± 6.0 | <0.001 |
⁎ Ejection fraction was available in 90% of the group with left main coronary artery percutaneous coronary intervention and 91% of the multivessel intervention group.
| Follow-Up (years) | LMCA PCI | Multivessel PCI |
|---|---|---|
| ≤1 | 468 (100%) | 1,973 (100%) |
| ≤2 | 384 (82.1%) | 1,749 (88.6%) |
| ≤3 | 303 (64.7%) | 1,503 (76.2%) |
| ≤4 | 211 (45.1%) | 1,178 (59.7%) |
| ≤5 | 117 (25.0%) | 795 (40.3%) |
| >5 | 46 (9.8%) | 473 (24.0%) |
In total 480 LMCA interventions were performed in 468 patients during the study period, consisting of 123 BMS PCIs and 357 DES PCIs. Of the 480 interventions, 158 (32.9%) were performed on the LMCA alone. In the remaining lesions, 220 LMCA interventions (45.8%) were accompanied by concomitant 1-vessel PCI, and 102 LMCA interventions (21.3%) were accompanied by multivessel PCI. Mean ± SD preprocedural estimated stenosis in the LMCA was 70.2 ± 14.2%, which decreased to 3 ± 10.7% after PCI. Thrombolysis In Myocardial Infarction grade 3 flow was obtained in all but 2 patients after the procedure.
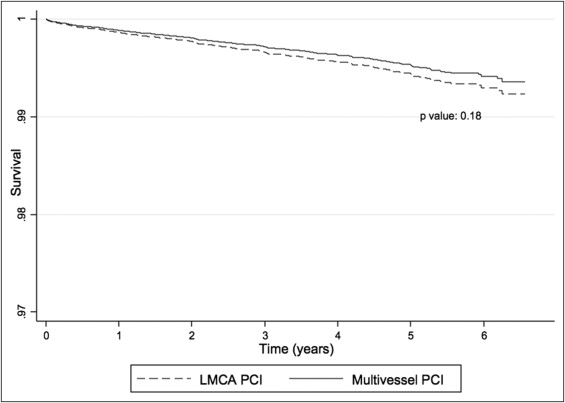
Nine patients (1.9%) undergoing LMCA PCI died within the 30-day postintervention period compared to 25 (1.3%, p = 0.3) in the multivessel PCI group. Using Cox proportional hazard modeling, no significant difference in adjusted long-term mortality ( Figure 1 ) was observed between the LMCA PCI and multivessel PCI groups (hazard ratio [HR] 1.20, 95% confidence interval [CI] 0.92 to 1.56). Figure 1 displays adjusted Kaplan–Meier survival curves comparing long-term mortality in the 2 study groups.
Adjusted mortality estimates derived from the generalized estimating equations approach are shown in Figure 2 . Using this modeling strategy, no significant differences in survival were evident between the LMCA PCI category and the multivessel PCI group (HR 0.81, 95% CI 0.49 to 1.37). Regression models with only preprocedural characteristics also showed similar results.
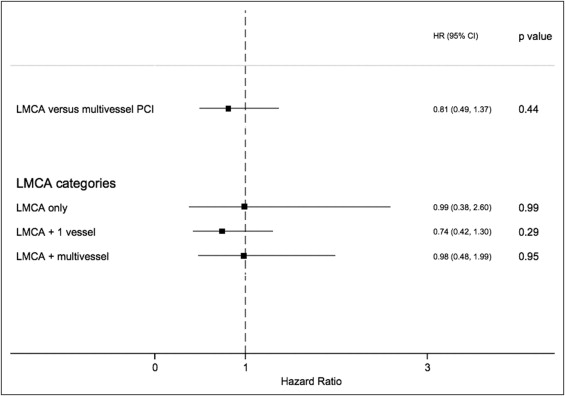
No significant differences in long-term mortality were observed when individual LMCA PCI categories, namely LMCA only, LMCA + 1-vessel PCI, and LMCA + multivessel PCI, were compared to the multivessel PCI group. Furthermore, no significant difference in long-term adjusted mortality was found between ostial LMCA PCI compared to nonostial LMCA PCI (HR 0.76, 95% CI 0.52 to 1.12). Comparison of unadjusted mortality estimates between the DES PCI and BMS PCI groups demonstrated that patients undergoing LMCA PCI with BMSs had a significantly higher mortality than patients undergoing LMCA PCI with DESs (p <0.001). However, adjusted analysis using the generalized estimating equations approach failed to demonstrate any statistically significant difference in mortality between the 2 groups (HR 0.83, 95% CI 0.59 to 1.18). Table 3 presents significant predictors of mortality in our study population. We observed that SYNTAX score, European System for Cardiac Operative Risk Evaluation score, diabetes, renal failure, former and current smoking, and decreased ejection fraction were significant predictors of mortality.
| Variable | HR | 95% CI | p Value |
|---|---|---|---|
| Age | 1.03 | 1.01–1.05 | <0.001 |
| Former smoker | 1.27 | 1.07–1.50 | 0.01 |
| Current smoker | 1.59 | 1.25–2.03 | <0.001 |
| Congestive heart failure | 1.52 | 1.26–1.84 | <0.001 |
| Diabetes mellitus | 1.29 | 1.11–1.50 | <0.001 |
| Renal failure | 1.91 | 1.46–2.50 | <0.001 |
| Chronic obstructive pulmonary disease | 1.30 | 1.08–1.57 | 0.01 |
| Ejection fraction | 0.98 | 0.97–0.99 | 0.03 |
| SYNTAX score | 1.02 | 1.01–1.03 | 0.02 |
| EuroSCORE | 1.02 | 1.01–1.03 | 0.02 |
We performed a time-sensitive analysis to observe the change in mortality trend over years caused by multiple factors including differential follow-up, improvement in intervention techniques, and change in patient selection criteria for high-risk PCI. Table 4 presents the improvement in mortality over years in the multivessel PCI and LMCA PCI groups (p for trend <0.001 for the 2 comparisons). However, no significant differences in mortality were observed between the 2 study groups in individual annual strata.



