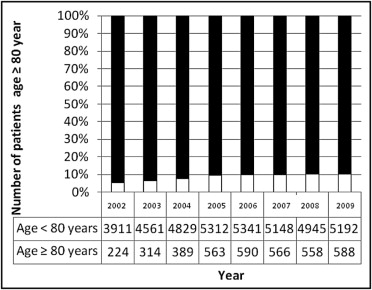
Patients ≥80 years old with coronary artery disease constitute a particular risk group in relation to percutaneous coronary intervention (PCI). From 2002 through 2008 we examined the annual proportion of patients ≥80 years old undergoing PCI in western Denmark, their indications for PCI, and prognosis. From 2002 through 2009 all elderly patients treated with PCI were identified in a population of 3.0 million based on the Western Denmark Heart Registry. Cox regression analysis was used to compare mortality rates according to clinical indications controlling for potential confounding. In total 3,792 elderly patients (≥80 years old) were treated with PCI and the annual proportion increased from 224 (5.4%) in 2002 to 588 (10.2%) in 2009. The clinical indication was stable angina pectoris (SAP) in 30.2%, ST-segment elevation myocardial infarction (STEMI) in 35.0%, UAP/non-STEMI in 29.7%, and “ventricular arrhythmia or congestive heart failure” in 5.1%. Overall 30-day and 1-year mortality rates were 9.2% and 18.1%, respectively. Compared to patients with SAP the adjusted 1-year mortality risk was significantly higher for patients presenting with STEMI (hazard ratio 3.86, 95% confidence interval 3.08 to 4.85), UAP/non-STEMI (hazard ratio 1.95, 95% confidence interval 1.53 to 2.50), and ventricular arrhythmia or congestive heart failure (hazard ratio 2.75, 95% confidence interval 1.92 to 3.92). In patients with SAP target vessel revascularization decreased from 7.1% in 2002 to 2.5% in 2008. In conclusion, the proportion of patients ≥80 years old treated with PCI increased significantly over an 8-year period. Patients with SAP had the lowest mortality rates and rates of clinically driven target vessel revascularization decreased over time.
Ischemic heart disease is the leading cause of death worldwide. The general population is aging and octogenarians are the fastest growing population segment. The prevalence of clinical coronary artery disease is high in elderly patients and this subgroup poses unique challenges in clinical management. As the number of elderly patients undergoing percutaneous coronary intervention (PCI) increases, it has become important to investigate invasive treatment procedures and outcomes in this subgroup. Although previous studies have shown that poor outcomes and mortality rates after PCI increase sharply with advanced age, improved outcomes have been reported more recently. Nevertheless, limited data are available on the safety and outcome of PCI in elderly patients with and without myocardial infarction. In most randomized trials age >75 or >80 years is an exclusion criteria ; thus elderly patients, particularly those with co-morbidities, have been under-represented. The purpose of this study was to assess trends in the annual proportion of patients undergoing PCI who were ≥80 years old, to identify their clinical indications, and to evaluate 30-day and 1-year mortality rates and rates of target lesion revascularization and target vessel revascularization according to clinical presentation.
Methods
This cohort study was conducted using western Denmark’s health care databases, which cover the region’s entire population (approximately 3.0 million inhabitants, 55% of Danish population). Data are registered prospectively in these databases. All patients were followed for 12 months except for patients treated in 2009. The databases have previously been described in detail. We used the Western Denmark Heart Registry (WDHR) to identify all PCIs recorded from January 1, 2002 through December 31, 2009 in elderly patients (≥80 years old). This registry has since 1999 collected detailed patient and procedure data for all interventions carried out in western Denmark’s 3 coronary intervention centers (Odense University Hospital, Odense; Aarhus University Hospital, Skejby; and Aarhus University Hospital, Aalborg).
Indications for PCI were (1) stable angina pectoris (SAP), (2) unstable angina pectoris (UAP)/non–ST-segment elevation myocardial infarction (NSTEMI), (3) STEMI, and (4) “other” (ventricular tachycardia, ventricular fibrillation, prehospital cardiac arrest with resuscitation without STEMI, and congestive heart failure). All patients were diagnosed and treated according to current standards with oral antiplatelet therapy according to current guidelines. Patients with SAP or UAP/NSTEMI were pretreated with aspirin (75 mg/day before the procedure or a loading dose of 300 mg) and clopidogrel (75 mg/day before the procedure or a loading dose of 300 to 600 mg). Patients with STEMI were pretreated with aspirin (300 mg), clopidogrel (300 to 600 mg), and intravenous heparin 10,000 IU during transport to or at the PCI center. The interventional strategy, stent selection, and use of periprocedural glycoprotein IIb/IIIa inhibitors were left to the discretion of the operator. Antiplatelet therapy after PCI included life-long aspirin (75 to 150 mg/day) and clopidogrel (75 mg/day). Since November 2002 the recommended duration of clopidogrel treatment has been 12 months for all stent types.
From 1977 until the implantation date we obtained data for each patient from the Danish National Registry of Patients on all hospital diagnoses. The Danish National Registry of Patients has covered all acute-care hospitals in Denmark since 1977. We computed co-morbidity scores using the Charlson Co-morbidity Index, which covers 19 major disease categories including diabetes mellitus, heart failure, cerebrovascular diseases, and cancer. The Charlson Co-morbidity Index score is a weighted summary of diagnoses with weights based on 1-year mortality associated with each disease in the original study by Charlson et al.
End points of the present study were all-cause 30-day and 1-year mortality and target lesion revascularization and target vessel revascularization at 1 year.
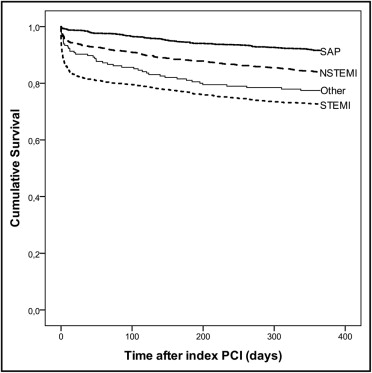
Data are presented as mean ± SD or median and interquartile range for continuous data or as counts. A Kruskal-Wallis test was used for quantitative dependent variables. Distributions of continuous data variables in the 4 groups were compared using the t test or the Mann-Whitney test depending on whether the data followed a normal distribution. We compared distributions of categorical variables using the chi-square test. The proportion of PCI procedures in elderly patients (≥80 years old) was counted. We constructed Kaplan–Meier curves for the prognosis of the 4 subgroups of elderly patients. We counted end-point events for the cohort of elderly patients during the follow-up period grouped by the following 4 indications: SAP, UAP/NSTEMI, STEMI, and “ventricular arrhythmia or congestive heart failure.” Follow-up began on the date of the index PCI procedure. In analyses of 30-day or 1-year all-cause mortality, follow-up continued until the date of death or until 12 months after implantation, whichever came first.
Cox regression analysis was used to compute hazard ratios as an estimate of relative mortality according to clinical indications controlling for the following potential confounding factors: age, gender, and co-morbidity. We controlled for co-morbidity index (100% complete data for all cases), whereas further variables presented in Table 1 were not used in adjusted analysis because of a substantial number of missing data. A p value ≤0.05 was considered statistically significant. SPSS 18.0 (SPSS, Inc., Chicago, Illinois) was used for analysis.
| Valid Cases | SAP | UAP/NSTEMI | STEMI | Other | p Value | |
|---|---|---|---|---|---|---|
| Number of patients | 3,792 | 1,145 | 1,126 | 1,326 | 195 | |
| Age (years) | 3,792 | 82.0 (81.0–84.0) | 83.0 (81.0–85.0) | 83.0 (81.0–86.0) | 82.0 (81.0–84.0) | <0.001 |
| Family history of coronary artery disease | 3,055 | 291 (27.7%) | 257 (28.0%) | 191 (20.8%) | 38 (22.4%) | <0.001 |
| Smoker | 2,907 | 116 (11.6%) | 122 (13.9%) | 195 (22.5%) | 24 (14.3%) | <0.001 |
| Diabetes mellitus | 3,144 | 145 (13.7%) | 154 (16.4%) | 96 (9.9%) | 27 (15.1%) | <0.001 |
| Hypertension | 3,184 | 668 (62.2%) | 537 (56.7%) | 398 (40.4%) | 104 (58.4%) | <0.001 |
| Previous coronary bypass | 3,215 | 111 (10.3%) | 67 (7.0%) | 26 (2.6%) | 16 (8.9%) | <0.001 |
| Previous percutaneous coronary intervention | 3,152 | 277 (26.0%) | 154 (16.4%) | 72 (7.4%) | 44 (25.1%) | <0.001 |
| Previous myocardial infarction | 3,152 | 357 (33.6%) | 380 (40.4%) | 136 (14.0%) | 71 (40.3%) | <0.001 |
| Lipid-lowering therapy | 3,189 | 672 (62.2%) | 508 (53.3%) | 156 (16.0%) | 77 (42.8%) | <0.001 |
| Glycoprotein IIb/IIIa inhibitor | 3,534 | 162 (15.2%) | 198 (18.8%) | 585 (47.1%) | 43 (24.7%) | <0.001 |
| Co-morbidity index score | 3,792 | <0.001 | ||||
| 0 | 301 (30.9%) | 293 (26.0%) | 533 (40.2%) | 44 (22.6%) | ||
| 1–2 | 537 (46.9%) | 535 (40.2%) | 563 (42.5%) | 93 (47.7%) | ||
| ≥3 | 307 (26.8%) | 298 (26.5%) | 230 (17.3%) | 58 (29.7%) | ||
| Number of lesions | 5,310 | 1,684 | 1,723 | 1,636 | 267 | |
| Treated coronary artery | <0.001 | |||||
| Left anterior descending | 688 (42.5%) | 674 (40.6%) | 717 (45.6%) | 102 (40.5%) | ||
| Left circumflex | 375 (23.2%) | 402 (24.2%) | 230 (14.6%) | 61 (24.2%) | ||
| Right | 476 (29.4%) | 444 (26.8%) | 584 (37.1%) | 79 (31.3%) | ||
| Left main | 79 (4.9%) | 139 (8.4%) | 43 (2.7%) | 10 (4.0%) | ||
| Lesion length (mm) | 12.0 (10.0–18.0) | 12.0 (10.0–18.0) | 18.0 (13.0–23.0) | 11.0 (8.0–17.0) | <0.001 | |
| Reference segment (mm) | 3.2 ± 0.6 | 3.2 ± 0.6 | 3.2 ± 0.6 | 3.1 ± 0.6 | 0.426 | |
| Stenosis (percent luminal diameter) | 92.0 (89.0–99.0) | 92.0 (89.0–99.0) | 100.0 (95.0–100.0) | 88.5 (75.0–96.0) | <0.001 | |
| Number of stents/lesion | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 0.286 | |
| Stent type | <0.001 | |||||
| Balloon angioplasty only | 184 (11.9%) | 188 (11.8%) | 192 (12.7%) | 33 (13.8%) | ||
| Drug-eluting stent | 929 (60.2%) | 820 (51.4%) | 518 (34.2%) | 86 (35.8%) | ||
| Bare-metal stent | 430 (27.9%) | 586 (36.8%) | 803 (53.1%) | 121 (50.4%) | ||
| Maximum balloon pressure (atm) | 16.2 ± 4.1 | 16.1 ± 4.1 | 15.4 ± 3.8 | 15.3 ± 3.7 | <0.001 | |
| Procedure time (minutes) | 3,681 | 24.0 (15.0–38.0) | 24.0 (15.0–38.0) | 21.0 (13.0–33.0) | 25.0 (17.0–35.0) | <0.001 |
| Fluoroscopic time (minutes) | 3,778 | 9.2 (5.3–15.7) | 9.2 (5.3–15.7) | 7.1 (4.1–11.8) | 8.3 (5.4–13.3) | <0.001 |
| Contrast (ml) | 42.0 (20.0–83.0) | 110.0 (70.0–175.0) | 100.0 (60.0–150.0) | 50.0 (24.8–80.0) | <0.001 |
Results
The study encompassed 3,792 consecutive elderly patients (≥80 years old) treated with PCI. From 2002 through 2009 the annual proportion of all patients undergoing PCI who were ≥80 years old increased from 224 (5.4%) in 2002 to 588 (10.2%) in 2009 ( Figure 1 ) . Indications for PCI were SAP (30.2%), UAP/NSTEMI (29.7%), STEMI (35.0%), and ventricular arrhythmia/congestive heart failure (5.1%). Patients’ median age was 83.0 years (81.0 to 85.0). Median age for the different clinical indications differed substantially among the 4 groups, with patients with STEMI being significantly older than patients with SAP (83.0 years, 81.0 to 86.0, vs 82.0 years, 81.0 to 84.0, p <0.001; Table 1 ). Most PCI-treated elderly patients were men (56.4%). Women receiving this treatment were significantly older than men (83.0 years, 81.0 to 86.0, vs 82.0 years, 81.0 to 85.0, p <0.001).
Most baseline patient and procedure characteristics ( Table 1 ) differed substantially among the 4 groups. As a population, elderly patients had a high prevalence of cardiovascular risk factors including smoking, diabetes, hypertension, and hypercholesterolemia and often had previous MI, PCI, and coronary artery bypass grafting. Prevalences of previous MI, PCI, and coronary artery bypass grafting were significantly lower in elderly patients with STEMI compared to elderly patients with SAP (p <0.001). The Charlson Co-morbidity Index also differed significantly among the 4 groups: the STEMI group had the highest frequency of no co-morbidity ( Table 1 ). Patients with STEMI were most likely to have the culprit lesions in the left anterior descending coronary artery, longer lesions, and implantation of longer stents. In contrast, they had shorter procedure and fluoroscopic times with less contrast used ( Table 1 ). Elderly patients with SAP had the longest procedure and fluoroscopic times and the most contrast used. Moreover, the highest balloon pressure was applied to coronary lesions in this indication group. Treated coronary arteries also differed substantially among the 4 groups (p <0.001). The left main coronary artery stem was treated significantly more often in the UAP/NSTEMI group (8.4%) compared to the SAP, STEMI, and ventricular arrhythmia/congestive heart failure indication groups (4.9%, 2.7%, and 4.0%, respectively, p <0.001). Use of drug-eluting stents increased from 0.0% in 2002 to 60.3% in 2008 (p <0.001).
One-year follow-up was complete for all patients (n = 3,792). Figure 2 shows cumulative mortality rates. Average all-cause 30-day mortality rate was 9.2%. Thirty-day mortality rate differed significantly among the 4 groups (p <0.001; Table 2 ) with the highest mortality rates observed in elderly patients treated with PCI because of STEMI (17.9%) and the indication ventricular arrhythmia/congestive heart failure (9.7%) and the lowest 30-day mortality rate was observed in PCI-treated patients with SAP (1.4%). Adjusting for age, gender, and co-morbidity showed that patients with SAP had the lowest 1-year mortality rate ( Table 3 ). Annual 30-day mortality rate did not change significantly during the observational period (8.1% in 2002 and 8.4% in 2008, p = 0.932). Average all-cause 1-year mortality rate was 18.1% with significant differences among the 4 groups ( Table 2 ). The highest 1-year mortality rate was observed in patients with STEMI (27.3%). A high 1-year mortality rate was also observed in the group with the indication ventricular arrhythmia/congestive heart failure (22.6%). The lowest 1-year mortality was observed in patients with SAP (8.5%). Adjusting for age, gender, and co-morbidity showed that patients with SAP had the lowest 1-year mortality rate ( Table 3 ). Annual 1-year mortality rate did not change significantly during the period of observation (14.9% in 2002 and 18.3% in 2008, p = 0.443).
| SAP | UAP/NSTEMI | STEMI | Other | p Value | |
|---|---|---|---|---|---|
| Death at 30 days | |||||
| All | 14 (1.5%) | 67 (6.9%) | 206 (18.1%) | 17 (10.0%) | <0.001 |
| 2002 | 0 (0.0%) | 5 (6.3%) | 12 (21.1%) | 1 (8.3%) | |
| 2003 | 2 (2.5%) | 7 (9.6%) | 23 (16.9%) | 0 (0.0%) | |
| 2004 | 0 (0.0%) | 7 (8.1%) | 27 (17.4%) | 2 (4.5%) | |
| 2005 | 4 (2.6%) | 10 (5.9%) | 39 (18.7%) | 6 (12.8%) | |
| 2006 | 3 (1.5%) | 9 (5.1%) | 44 (21.2%) | 3 (23.1%) | |
| 2007 | 2 (1.2%) | 17 (8.9%) | 35 (17.6%) | 0 (0.0%) | |
| 2008 | 3 (1.8%) | 12 (6.2%) | 27 (14.8%) | 5 (27.8%) | |
| p Value | 0.613 | 0.748 | 0.771 | 0.023 | |
| Death at 1 year | |||||
| All | 84 (9.1%) | 167 (17.2%) | 324 (28.4%) | 40 (23.5%) | <0.001 |
| 2002 | 4 (5.5%) | 9 (11.3%) | 17 (29.8%) | 3 (25.0%) | |
| 2003 | 9 (11.3%) | 16 (21.9%) | 44 (32.4%) | 1 (4.5%) | |
| 2004 | 2 (2.2%) | 20 (23.3%) | 41 (26.5%) | 6 (13.6%) | |
| 2005 | 19 (12.5%) | 26 (15.3%) | 52 (25.6%) | 13 (27.7%) | |
| 2006 | 18 (9.1%) | 30 (17.1%) | 63 (30.3%) | 4 (30.8%) | |
| 2007 | 12 (7.3%) | 38 (19.8%) | 60 (30.2%) | 6 (42.9%) | |
| 2008 | 20 (12.3%) | 28 (14.5%) | 47 (25.7%) | 7 (38.9%) | |
| p Value | 0.078 | 0.265 | 0.745 | 0.045 | |
| Target vessel revascularization at 1 year | |||||
| All | 69 (5.0%) | 61 (4.1%) | 62 (4.4%) | 8 (3.4%) | 0.587 |
| 2002 | 7 (7.1%) | 7 (5.3%) | 4 (6.2%) | 2 (11.1%) | |
| 2003 | 8 (7.0%) | 4 (3.7%) | 6 (3.6%) | 2 (6.1%) | |
| 2004 | 9 (6.2%) | 4 (2.8%) | 15 (7.2%) | 1 (1.6%) | |
| 2005 | 8 (3.3%) | 11 (4.2%) | 7 (2.8%) | 2 (3.1%) | |
| 2006 | 25 (8.1%) | 7 (2.5%) | 14 (5.6%) | 0 (0.0%) | |
| 2007 | 6 (2.5%) | 17 (5.9%) | 9 (3.5%) | 0 (0.0%) | |
| 2008 | 6 (2.5%) | 11 (4.0%) | 7 (3.1%) | 1 (4.0%) | |
| p Value | 0.012 | 0.479 | 0.215 | 0.469 | |
| Target lesion revascularization at 1 year | |||||
| All | 41 (3.0%) | 35 (2.3%) | 47 (3.3%) | 5 (2.1%) | 0.392 |
| 2002 | 5 (5.1%) | 4 (3.0%) | 2 (3.1%) | 1 (5.6%) | |
| 2003 | 6 (5.3%) | 4 (3.7%) | 4 (2.4%) | 1 (3.0%) | |
| 2004 | 3 (2.1%) | 4 (2.8%) | 13 (6.3%) | 1 (1.6%) | |
| 2005 | 5 (2.0%) | 8 (3.0%) | 7 (2.8%) | 1 (1.5%) | |
| 2006 | 17 (5.5%) | 4 (1.4%) | 11 (4.4%) | 0 (0.0%) | |
| 2007 | 2 (0.8%) | 7 (2.4%) | 6 (2.4%) | 0 (0.0%) | |
| 2008 | 6 (2.0%) | 4 (1.4%) | 4 (1.7%) | 1 (4.0%) | |
| p Value | 0.007 | 0.699 | 0.149 | 0.884 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


