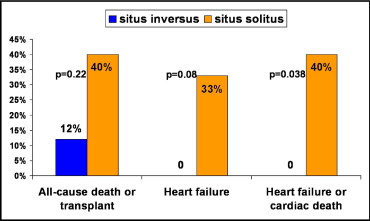
The long-term outcome of patients with congenitally corrected transposition of the great arteries is mainly determined by progressive morphologically tricuspid valve regurgitation, heart block, atrial arrhythmias, and/or systemic ventricular dysfunction. Situs abnormalities have been reported in ≤34% of cases, but whether clinical differences exist between a situs inversus and situs solitus arrangement has not yet been studied. The clinical records of 38 adults with congenitally corrected transposition of the great arteries (mean age 40 ± 15 years) followed for a mean period of 7.4 years were reviewed. Of these 38 patients, 8 presented with situs inversus and 30 with situs solitus. No significant differences were found between the 2 groups in age, gender, ventricular septal defect, pulmonary tract stenosis, previous surgical repair, or duration of follow-up. However, none of the patients with situs inversus presented with an Ebstein-like anomaly of the morphologically tricuspid valve and none developed nonoperative-related complete atrioventricular block compared to 15 (50%; p = 0.013) and 11 (42%; p = 0.032) of the patients with situs solitus, respectively. At follow-up, 2 patients with situs inversus (25%) presented with sustained atrial arrhythmia, severe tricuspid regurgitation, or severe systemic right ventricular systolic dysfunction compared to 22 (73%) of 30 those with situs solitus (p = 0.034). No patient with situs inversus presented with cardiac death or severe heart failure compared to 12 (40%) of 30 with situs solitus (p = 0.038). In conclusion, Ebstein-like anomaly or spontaneous complete atrioventricular block are rare in patients with congenitally corrected transposition of the great arteries with situs inversus, and late complications are uncommon. The long-term outcome of patients with situs inversus was significantly better than that for patients with situs solitus.
Congenitally corrected transposition of the great arteries (ccTGA) is a rare form of congenital heart disease that can present clinically at any age from fetus to elderly. Recognizable associated abnormalities include ventricular septal defect (VSD), pulmonary stenosis or atresia, abnormalities of the morphologically tricuspid valve, and complete atrioventricular (AV) block. The long-term outcome of patients with ccTGA varies depending on the severity of the associated malformations and the timing and approach to surgical palliative repair. Adult patients with ccTGA are prone to the development of morphologically tricuspid valve regurgitation, systemic ventricular dysfunction, heart block, and atrial arrhythmias. Most cases of ccTGA occur in those with situs solitus, but situs abnormalities were reported in 34% of patients in a pediatric series. In general, situs inversus is regarded as a mirror image of the normal arrangement; however, whether clinical differences between those with ccTGA and situs inversus versus situs solitus exist has not yet been studied. The aim of the present study was to compare the clinical characteristics and outcomes of patients with situs solitus and situs inversus in an adult population diagnosed with ccTGA.
Methods
The clinical records of all adult patients aged >18 years, diagnosed with ccTGA, and referred to the Adult Congenital Heart Disease unit at La Paz University Hospital (Madrid, Spain) from January 1990 to January 2012 were reviewed. The diagnosis of ccTGA, regardless of the situs visceroatrial or ventricular looping, was determined by demonstrating discordance of both the AV and the ventriculoarterial connections using 2-dimensional echocardiography (2DE) or cardiac magnetic resonance imaging (MRI), or both. Using the inclusion and exclusion criteria outlined by Graham et al, patients with heterotaxy syndrome, double-inlet AV connection, hypoplastic right or left heart syndrome, single ventricle, superior-inferior ventricles, and crisscross heart were excluded from the present analysis. Patients with associated cardiac lesions such as VSD, pulmonary stenosis or atresia, abnormalities of the tricuspid valve with or without Ebstein-like malformation, and double-outlet right ventricle were considered for the analysis. The local research ethics committee approved the study.
The visceroatrial situs arrangement was established by 2DE and/or MRI. The patients were classified into situs inversus or situs solitus groups. The clinical and complementary examination data from 2DE, MRI, electrophysiologic study, and/or cardiac catheterization were compared between the 2 groups. The incidence of symptomatic supraventricular arrhythmias was investigated. Nonsustained arrhythmias captured from Holter monitoring or data on ambient ectopy were not considered for the analysis. The severity of the morphologically tricuspid valve regurgitation was assessed by 2DE-Doppler according to previously established methods. Severe regurgitation was diagnosed when a large regurgitating jet with a vena contracta width >7 mm or a wall-impinging jet of any size, swirling in the left atrium, was detected. Evaluation of ventricular function was determined using 2DE and/or MRI. Severe systemic right ventricular systolic dysfunction was diagnosed when estimated or measured ejection fraction was <35%. For outcome analysis, a composite end point included all-cause mortality, heart transplantation, or hospital admission because of severe heart failure. Cardiac death was considered when death was sudden or from progressive heart failure or when cardiac transplantation was performed.
SPSS, version 15.0, for Windows (SPSS, Chicago, Illinois) was used for the statistical analyses. Quantitative values are summarized as the mean ± SD and categorical variables as percentages. Long-term follow-up was computed from the first visit at the adult congenital heart disease unit to the last clinical visit, or until an end point was reached. For the purposes of the analyses, age and follow-up time were considered continuous variables, and all other variables were considered categorical. The comparison of variables between groups was performed with Fisher’s exact test or Student’s t test, as appropriate. Kaplan-Meier curves of actuarial survival free from heart transplantation and cumulative freedom from cardiac death, transplantation, or hospital admission because of heart failure in both groups were performed, using the log-rank test for comparison. Two-tailed p values <0.05 were considered statistically significant.
Results
A total of 38 patients diagnosed with ccTGA and with potentially suitable anatomy for biventricular repair in the presence of balanced ventricles constituted the study population ( Table 1 ). The mean age at the last examination was 40 ± 15 years and 21 were men (55%). Associated anomalies, including VSD, pulmonary stenosis or atresia, complete AV block, or Ebstein-like anomaly, were present in 33 patients (87%). Surgical repair of associated intracardiac lesions had been performed in 13 patients.
| Variable | Overall (n = 38) | Situs Inversus (n = 8) | Situs Solitus (n = 30) | p Value |
|---|---|---|---|---|
| Men | 21 (55%) | 3 (38%) | 18 (60%) | 0.43 |
| Age at last examination (years) | 40 ± 15 | 40 ± 17 | 40 ± 14 | 0.99 |
| Follow-up time (years) | 7 ± 7 | 8 ± 8 | 7 ± 7 | 0.93 |
| Surgical palliative repair | 13 (34%) | 2 (25%) | 11 (37%) | 0.67 |
| Ventricular septal defect | 22 (58%) | 4 (50%) | 18 (60%) | 0.70 |
| Pulmonary stenosis or atresia ⁎ | 21 (55%) | 5 (63%) | 16 (53%) | 0.71 |
| Ebstein-like anomaly | 15 (40%) | 0 | 15 (50%) | 0.013 |
| Complete atrioventricular block | 18 (47%) | 1 (12%) | 17 (57%) | 0.045 |
⁎ Nineteen patients presented with nonrestrictive ventricular septal defect.
The visceroatrial arrangement was situs inversus in 8 patients (21%) and solitus inversus in 30. No significant differences were found in age, gender, frequency of associated VSD, previous surgical repair, or follow-up duration between the 2 groups ( Table 1 ). Two patients with pulmonary valve atresia had situs inversus but none had situs solitus, and no significant difference was seen in the prevalence of pulmonary stenosis between the 2 groups. Three patients in situs solitus group, but none in the situs inversus group, had a double-outflow right ventricle. None of the patients with situs inversus had an Ebstein-like anomaly of the tricuspid valve but 15 patients (50%) with situs solitus did so (p = 0.013). Also, only 1 patient (12%) with situs inversus developed complete AV block compared to 17 (57%) with situs solitus (p = 0.045). Moreover, none of the patients with situs inversus had nonsurgically related complete AV block compared to 11 (42%) with situs solitus (p = 0.032).
We observed differences in the clinical outcomes between the 2 groups during the adult follow-up ( Figure 1 ), but these differences were not statistically significant: 1 patient with situs inversus experienced clinically sustained atrial arrhythmias versus 15 with situs solitus; no patient with situs inversus developed severe tricuspid regurgitation versus 10 with situs solitus; and 1 patient with situs inversus presented with severe systemic right ventricular systolic dysfunction compared to 11 with situs solitus. Despite this, the overall frequency of complications was significantly greater in the group with situs solitus (22 of 30 patients vs 2 of 8 patients; p = 0.034).

After a mean follow-up of 7.4 years, 9 patients had died, 4 had undergone heart transplantation, and 10 patients had been admitted because of severe heart failure. Long-term mortality was lower in the situs inversus group (12% vs 40%), but this difference was not statistically significant ( Figure 2 ). One patient in the situs inversus group with pulmonary atresia and severe pulmonary ischemia died after palliative cardiac surgery, but no patient in that group presented with severe heart failure or cardiac death. In contrast, in the group with situs solitus, 10 patients were admitted to the hospital or died from heart failure, 2 patients experienced sudden cardiac death, and 1 patient died after pacemaker replacement. In summary, heart failure or cardiac death occurred in 12 patients with situs solitus versus none with situs inversus (p = 0.038; Figure 2 ). The Kaplan-Meier actuarial curve for survival free from heart transplantation and the cumulative survival curve for freedom from cardiac death or hospital admission for heart failure are shown in Figure 3 .

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


