Diabetes mellitus confers the highest mortality risk in primary and secondary cardiovascular prevention, but long-term prognosis differences between different forms of cardiovascular disease have not been assessed. We hypothesized that acute heart failure (HF) could have poorer outcomes than acute coronary heart disease (CHD) in patients with diabetes. We performed a prospective study of all consecutive patients admitted in a single year. Patients were categorized according to main cardiologic diagnosis: acute HF, acute CHD, rhythm disorders, or noncardiac disease. A total of 1,293 patients were included, 31.8% had diabetes and had higher mean age, more risk factors, previous cardiovascular disease, and co-morbidities. Hospital mortality (5.6% vs 1.7%; p <0.01) was higher in patients with diabetes. During follow-up (median 58.0 months; interquartile range 31.0 to 60.0), diabetic patients had higher cardiovascular mortality (27.2% vs 9.6%; p <0.01) and all-cause mortality (35.8% vs 14.5%; p <0.01); cardiovascular disease accounted for 75% of deaths. According to discharge diagnosis, patients with diabetes only had higher mortality rates in the subgroup of acute CHD. Acute HF was the diagnosis with higher cardiovascular (36.9%) and all-cause mortality (44.1%), followed by acute CHD (16.8% and 24.4%) and rhythm disorders (5.8% and 8.8%). Multivariate analysis identified an independent association with higher long-term mortality of acute HF and acute CHD in patients with and without diabetes. In conclusion, 1/3 of cardiology-admitted patients have diabetes and have poorer long-term prognosis, especially when discharged with the diagnosis of acute HF or acute CHD.
Diabetes mellitus (DM) is the risk factor that, individually, confers the highest risk for cardiovascular disease being coronary heart disease (CHD) the leading cause of mortality in patients with DM. All clinical guidelines classify DM in high-risk categories although most evidence has focused on CHD incidence and mortality. The prevalence of DM is around 30% to 35% in patients with acute coronary syndromes, and most studies have identified poorer outcomes in diabetic patients. In contrast, the incidence and prevalence of heart failure (HF) have increased in last decades, and the presence of DM is similar to acute coronary syndrome patients, which has lead to an increasing interest in the role of DM in HF prognosis. The prevalence of DM has increased exponentially in last decades and is estimated that it will increase twofold by 2030, especially in subjects >65 years. These estimations preclude an increase in hospital admissions and economic burden because most of threefold higher economic costs of diabetic patients is driven by hospital admissions. According to such data, it is crucial to uptake preventive measures directed to decrease DM incidence but, also, a wide analysis of which forms of cardiovascular disease confer the higher risk of mortality in current diabetic patients. The aim of our study was assessing the long-term prognosis of patients with DM after a hospital admission and describing their leading causes of mortality.
Methods
This was an observational and prospective study performed in a single center. Since December 2008, we initiated an on-going registry of all nonscheduled admissions in the Cardiology division. In 2009, we recorded 1,496 admissions and after excluding 165 patients for being re-admissions and 38 patients with severe aortic stenosis or severe mitral regurgitation with indications for percutaneous or surgical intervention, the final sample size was 1,293 patients. The registry and the informed consent have been approved by the ethics committee of the institution. Investigators and patients participated under the ethics, consent, and permissions heading.
Patients were codified in the DM group if they had been previously diagnosed, either by such diagnosis in a medical report or by patients’ interview or if they were under specific antidiabetic treatments. Local protocol includes routine screening for unknown DM only in patients admitted for acute CHD. Newly diagnosed DM was established for patients without previous diagnosis in whom glycated hemoglobin (HbA1c) >6.5% was detected. We decided to exclude these patients for the long-term analyses to have 2 well-defined groups (DM vs non-DM) ; newly diagnosed patients were a small group (only 51 patients, 3.4% of the cohort), and recommendations in lifestyle changes at discharge could have improved glycemic metabolism in many of these patients that would no longer fulfill criteria for diabetes. All clinical antecedents, risk factors, treatments, test, and complications were recorded during hospital stay. Admission diagnosis were grouped in 4 groups: (1) no cardiac disease (nonischemic chest pain, vagal syncope, and premature beats), (2) acute CHD (acute coronary syndromes and unstable angina); (3) acute HF (with and without depressed left ventricular ejection fraction), and (4) rhythm disorders (atrial fibrillation, auricular-ventricular block, and pacemaker dysfunction). Glomerular filtration rate was assessed from serum creatinine values with the Modification of Diet in Renal Disease Study equation. The overall analysis of co-morbidities was performed by the Charlson index adapted for patients with cardiovascular disease. All diagnosis and medical antecedents are collected by cardiologist that make the database very reliable. Clinical follow-up was performed by reviewing the electronic medical reports and by telephone. Primary end point during follow-up was cardiovascular mortality, and secondary end point was all-cause mortality.
Data were processed with SPSS 22.0 software for MAC. Quantitative variables are presented as mean (SD), and differences were assessed by the Student’s t test and chi-square tests. Qualitative variables are presented as percentages, and differences were analyzed by ANOVA test. Event rates through follow are presented by Kaplan-Meier curves, and survival analyses were performed by the log-rank tests; Cox regression models were performed for multivariate analyses. All multivariate analysis were adjusted by all variables that obtained p values <0.1 in the univariate analysis or could have plausible clinical implication. Statistical difference was accepted at p <0.05.
Results
The prevalence of DM in nonscheduled cardiology admissions was 31.8%. As listed in Table 1 , patients with DM had higher mean age, more cardiovascular risk factors, previous cardiovascular disease, and higher Charlson index. Acute CHD was the most frequent diagnosis and was significantly higher in patients with DM; acute HF diagnosis was also higher in diabetic patients; meanwhile, rhythm disorders or noncardiac disease were less frequent. Hospital mortality was 2.9% (38 patients), and it was higher in patients with DM (5.6% vs 1.7%; p <0.01). Mean hospital stay was 4.9 days (3.8) and was higher in diabetic patients (5.4 ± 4.0 vs 4.6 ± 3.7; p <0.01). In 51 nondiabetic patients (3.4% of the cohort), HbA1c >6.5% was detected and in 29 (51.8%) of them, an antidiabetic treatment was started (82.7% with metformin); the 51 patients were excluded from the follow-up analyses.
| Variable | Diabetes Mellitus | |||
|---|---|---|---|---|
| Total (n=1293) | No (n=882 (68.2%)) | Yes (n=411 (31.8%)) | p | |
| Age (years) | 71.0 (13.2) | 70.2 (14.2) | 72.6 (10.7) | <0.01 |
| Men | 57.3% | 57.5% | 56.9% | 0.83 |
| Body Mass Index (kg/m 2 ) | 28.3 (4.2) | 28.0 (4.2) | 28.7 (4.2) | 0.20 |
| Systolic blood pressure (mmHg) | 130.5 (24.2) | 130.4 (24.0) | 130.5 (24.6) | 0.94 |
| Diastolic blood pressure (mmHg) | 72.4 (13.4) | 72.6 (12.8) | 71.9 (14.5) | 0.48 |
| Hypertension | 70.7% | 65.2% | 82.7% | <0.01 |
| Current smokers | 18.2% | 19.5% | 15.4% | 0.08 |
| Dyslipidemia | 44.0% | 35.9% | 61.5% | <0.01 |
| Previous coronary heart disease | 28.9% | 22.3% | 43.0% | <0.01 |
| Previous heart failure | 9.2% | 7.8% | 12.1% | 0.01 |
| Previous stroke | 6.6% | 5.3% | 9.5% | <0.01 |
| Peripheral arterial disease | 4.2% | 2.3% | 8.3% | <0.01 |
| Left ventricle ejection fraction | 56.7 (11.4) | 58.0 (10.4) | 54.5 (12.8) | <0.01 |
| Glomerular filtration rate (<60 ml/min/1.72m 2 ) | 29.7% | 24.3% | 39.1% | <0.01 |
| Charlson Index | 2.0 (1.7) | 1.2 (1.1) | 3.7 (1.5) | <0.01 |
| Charlson index ≥4 | 13.8% | 4.0% | 35.2% | <0.01 |
| Hemoglobin (g/dl) | 12.9 (2.0) | 13.2 (1.9) | 12.4 (2.0) | <0.01 |
| Glomerular filtration rate (ml/min/1.72m 2 ) | 73.6 (28.5) | 76.8 (28.8) | 68.1 (27.0) | 0.01 |
| Total cholesterol total (mg/dl) | 164.3 (46.3) | 170.3 (45.9) | 154.0 (45.1) | <0.01 |
| High-density lipoprotein cholesterol (mg/dl) | 41.3 (13.4) | 42.7 (13.7) | 38.9 (12.4) | <0.01 |
| Triglycerides (mg/dl) | 138.9 (87.4) | 130.2 (65.1) | 153.9 (114.9) | <0.01 |
| Low-density lipoprotein cholesterol (mg/dl) | 96.8 (45.8) | 103.0 (50.6) | 85.7 (32.8) | <0.01 |
| Glycated hemoglobin (%) | 6.7 (1.3) | 6.0 (0.6) | 7.7 (1.4) | <0.01 |
| Main diagnosis | ||||
| No cardiac disease | 31.4% | 35.8% | 21.9% | <0.01 |
| Acute coronary heart disease | 31.9% | 26.8% | 42.8% | <0.01 |
| Acute heart failure | 20.1% | 17.3% | 26.4% | <0.01 |
| Rhythm disorders | 11.8% | 14.2% | 6.7% | <0.01 |
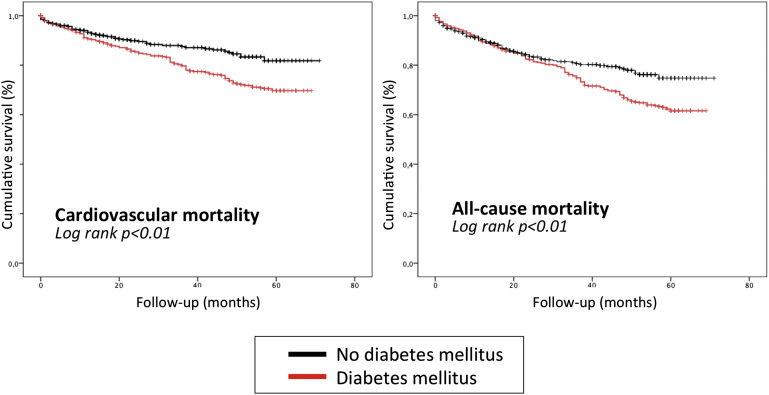
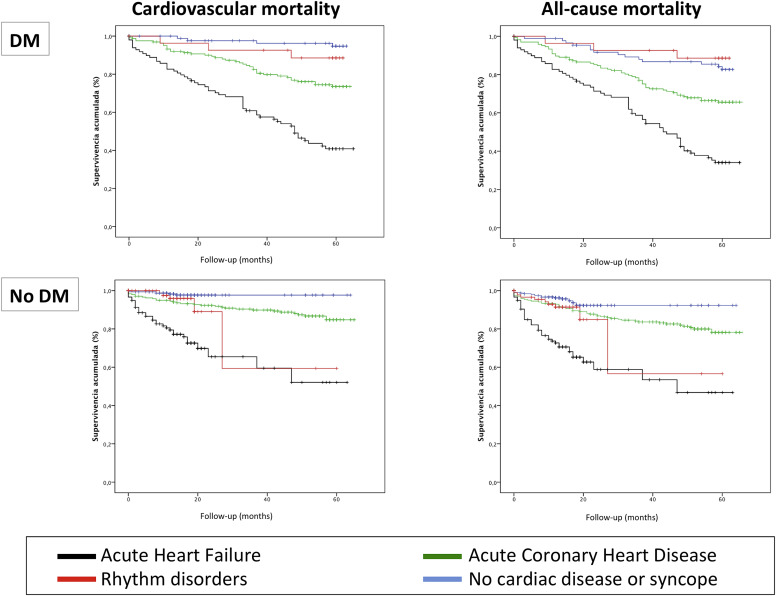
From the 1,202 discharged patients, 397 (33.0%) had DM. A complete follow-up was achieved in 92.4%, median time 58.0 months (interquartile range 31.0 to 60.0). During follow-up, 264 patients (20.4%) died, 189 (14.6%) from cardiovascular disease. As shown in Figure 1 , patients with DM had higher cardiovascular (27.2% vs 9.6%; log-rank p <0.01) and all-cause (35.8% vs 14.5%; log-rank p <0.01) mortality rates. Acute HF had the highest cardiovascular (36.9%) or all-cause (44.1%) mortality, followed by acute CHD (16.8% and 24.4%). No differences in mortality rates were observed in acute HF regardless of ejection fraction as happened in non-ST or ST-elevation acute coronary syndromes. When each clinical diagnosis was analyzed separately, patients with DM had higher mortality rates only in the subgroup of acute CHD ( Figure 2 ).
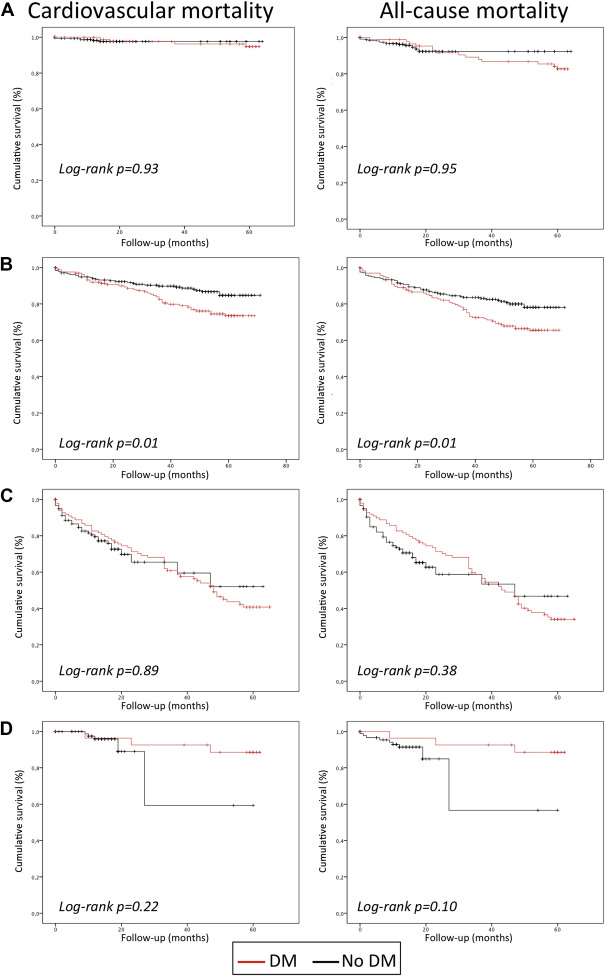
We finally conducted the same analysis in patients with and without DM and observed that acute HF was the cardiac disease with higher mortality in both groups ( Figure 3 ). The multivariate analysis, performed by Cox regression adjusted by age, gender, risk factor, glomerular filtration rate, medical antecedents, and pharmacologic treatments, identified acute HF and acute CHD as the diagnosis with higher cardiovascular and all-cause mortality in patients with and without DM ( Table 2 ).
| Variables | Cardiovascular mortality | All-cause mortality |
|---|---|---|
| Age | 1.10 (95% CI 1.05-1.10); p<0.01 | 1.10 (95% CI 1.05-1.10); p<0.01 |
| Previous HF | 1.51 (95% CI 1.00-2.33); p=0.05 | 1.53 (95% CI 1.05-2.23); p=0.03 |
| Acute CHD | 4.21 (95% CI 2.01-8.80); p<0.01 | 1.87 (95% CI 1.12-2.93); p<0.01 |
| Acute HF | 7.70 (95% CI 3.58-16.59); p<0.01 | 3.00 (95% CI 1.84-4.88); p<0.01 |
| No diabetes | ||
| Age | 1.10 (95% CI 1.05-1.11); p<0.01 | 1.10 (95% CI 1.05-1.10); p<0.01 |
| Previous CHD | – | 1.55 (95% CI 0.99-2.45); p=0.05 |
| Rhythm disorders | 4.12 (95% CI 1.15-15.2); p=0.03 | – |
| Acute CHD | 4.40 (95% CI 1.51-12.81); p<0.01 | 2.32 (95% CI 1.12-4.72); p=0.02 |
| Acute HF | 10.6 (95% CI 3.37-25.72); p<0.01 | 4.21 (95% CI 1.19-9.27); p<0.01 |
| Diabetes | ||
| Age | 1.10 (95% CI 1.01-1.15); p<0.01 | 1.10 (95% CI 1.05-1.10); p<0.01 |
| Acute CHD | 5.26 (95% CI 1.86-14.91); p<0.01 | 2.21 (95% CI 1.16-3.89); p<0.01 |
| Acute HF | 7.21 (95% CI 2.53-20.53); p<0.01 | 2.93 (95% CI 1.57-5.48); p=0.02 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


