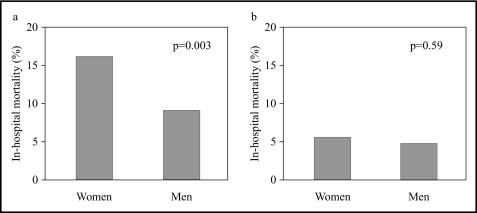
The aim of the present study was to investigate the gender-specific mortality after acute myocardial infarction in those aged <70 years versus ≥70 years. The present study consisted of 2,677 consecutive patients with acute myocardial infarction who had undergone coronary angiography within 24 hours after the onset of symptoms. The patients were divided into 2 groups: 1,810 patients <70 years old and 867 patients ≥70 years old. Women were older and had a greater incidence of hypertension and diabetes mellitus and a lower incidence of current smoking and previous myocardial infarction in both groups. The in-hospital mortality rate was significantly greater in women ≥70 years old age than in men ≥70 years old (16.2% vs 9.3%, respectively; p = 0.003) but was comparable between women and men in patients <70 years old (5.7% vs 4.9%, respectively; p = 0.59). On multivariate analysis, the association between female gender and in-hospital mortality in patients ≥70 years old remained significant (odds ratio 1.78, 95% confidential interval 1.05 to 3.00), but the gender difference was not observed in patients <70 years old (odds ratio 1.09, 95% confidence interval 0.53 to 2.24). In conclusion, female gender was associated with in-hospital mortality after acute myocardial infarction in patients ≥70 years old but not in patients <70 years old.
Acute myocardial infarction (AMI) is a leading cause of mortality in women and men in the developed countries. It has been well demonstrated that the mortality after AMI is greater in women than in men. Age is another important risk factor for both women and men ; however, female patients with AMI are an average of 10 years older than male patients. It has been reported that older age accounts for a greater part of the excess deaths among female patients with AMI. However, it remains unknown whether the gender-specific mortality after AMI is different between older and younger patients. In the present study, we assessed the in-hospital mortality of women and men with AMI aged <70 and ≥70 years.
Methods
The present study consisted of 2,677 consecutive patients with AMI who had undergone coronary angiography within 24 hours after the onset of symptoms at Hiroshima City Hospital, a tertiary referral institution of Hiroshima City. AMI was diagnosed by chest pain consistent with ongoing myocardial ischemia persisting >30 minutes and concomitant electrocardiographic changes. The serum creatine kinase was measured every 3 hours for ≥24 hours, and the peak creatine kinase value was required to be more than twice the normal upper limit. The patients were divided into 2 groups: 1,810 patients <70 years old and 867 patients ≥70 years old. All patients provided written informed consent, and the ethical committee of human research of Hiroshima City Hospital approved the study.
Emergency coronary angiography was performed as previously reported. Selective coronary angiography was performed in multiple projections before the initiation of reperfusion therapy. Immediately after diagnostic angiography, reperfusion therapy was performed. The allocation of reperfusion therapy was the physician’s decision.
All coronary angiograms were reviewed by 2 angiographers without knowledge of the clinical variables. The perfusion status of the infarct-related artery was determined in accordance with the Thrombolysis In Myocardial Infarction (TIMI) study classification. An initially occluded artery was defined as TIMI 0 or TIMI 1 flow before the initiation of reperfusion therapy. Successful reperfusion was defined as TIMI 3 flow on the final shot of the angiogram. Multivessel coronary disease was defined as ≥75% stenosis in ≥1 vessels remote from the infarct artery. Collateral circulation was considered present if partial or complete filling of the infarct artery distal to the infarct lesion was present.
Categorical data are reported as the proportions and continuous data as the mean ± SD. Statistical analysis was performed using the chi-square test for categorical variables. The t test was used for continuous variables. Logistic regression analysis was used to obtain the odds ratio (OR) and 95% confidence interval (CI) for in-hospital mortality. Multivariate analysis was performed, adjusting for age (model 1) or for age, hypertension, diabetes mellitus, current smoking, Killip class, interval to angiography, infarct location, initial occlusion of the infarct artery, collateral circulation, multivessel disease, use of primary percutaneous coronary angioplasty (PCI) and final reperfusion (model 2). We used the JMP statistical package, version 5.1 J (SAS Institute, Cary, North Carolina), for statistical analysis. A significance level of p = 0.05 was used and 2-tailed tests were applied.
Results
Of the 2,677 patients, 559 were women (20.9%) and 2,118 were men (79.1%). The women were significantly older than the men (69.2 ± 10.8 vs 61.5 ± 11.4 years, respectively; p <0.001). The proportion of women was significantly larger in the ≥70-year-old group than in the <70-year-old group (34.1% vs 14.5%, respectively; p <0.001). The baseline clinical and angiographic characteristics of the women and men aged ≥70 years are listed in Table 1 . These variables for the patients aged <70 years are listed in Table 2 .
| Variable | Women (n = 290) | Men (n = 571) | p Value |
|---|---|---|---|
| Age (y) | 77.1 ± 5.5 | 75.4 ± 4.6 | <0.001 |
| Hypertension | 176 (60%) | 288 (45%) | <0.001 |
| Diabetes mellitus | 88 (30%) | 135 (24%) | 0.05 |
| Current smoker | 34 (12%) | 242 (42%) | <0.001 |
| Previous myocardial infarction | 28 (10%) | 89 (16%) | 0.01 |
| Killip class 2–4 | 54 (18%) | 81 (14%) | 0.12 |
| Interval to admission (hr) | 5.9 ± 5.5 | 5.3 ± 4.9 | 0.12 |
| Anterior wall location | 143 (48%) | 253 (44%) | 0.26 |
| Initial Thrombolysis In Myocardial Infarction 0-1 | 217 (73%) | 412 (72%) | 0.72 |
| Collaterals | 64 (22%) | 144 (25%) | 0.24 |
| Multivessel coronary disease | 120 (41%) | 242 (42%) | 0.60 |
| Reperfusion therapy | |||
| Primary coronary angioplasty | 233 (79%) | 447 (78%) | 0.88 |
| Use of stents | 150 (51%) | 291 (51%) | 0.94 |
| Thrombolysis | 40 (14%) | 72 (13%) | 0.71 |
| Coronary bypass surgery | 7 (2%) | 27 (5%) | 0.08 |
| Final Thrombolysis In Myocardial Infarction 3 (n = 837) ⁎ | 214 (74%) | 421 (77%) | 0.28 |
| Variable | Women (n = 263) | Men (n = 1,547) | p Value |
|---|---|---|---|
| Age (y) | 60.4 ± 8.2 | 56.4 ± 8.5 | <0.001 |
| Hypertension | 136 (51%) | 612 (40%) | <0.001 |
| Diabetes mellitus | 80 (30%) | 370 (24%) | 0.03 |
| Current smoker | 92 (35%) | 984 (64%) | <0.001 |
| Previous myocardial infarction | 10 (4%) | 187 (12%) | <0.001 |
| Killip class 2–4 | 33 (13%) | 181 (12%) | 0.67 |
| Interval to admission (hr) | 5.1 ± 4.9 | 5.0 ± 4.9 | 0.81 |
| Anterior wall location | 135 (51%) | 815 (53%) | 0.88 |
| Initial Thrombolysis In Myocardial Infarction 0-1 | 202 (77%) | 1,194 (77%) | 0.89 |
| Collaterals | 73 (28%) | 467 (30%) | 0.42 |
| Multivessel coronary disease | 96 (37%) | 537 (35%) | 0.57 |
| Reperfusion therapy | |||
| Primary coronary angioplasty | 186 (71%) | 1,152 (75%) | 0.21 |
| Use of stents | 103 (39%) | 671 (43%) | 0.20 |
| Thrombolysis | 50 (19%) | 255 (17%) | 0.32 |
| Coronary bypass surgery | 7 (3%) | 72 (5%) | 0.12 |
| Final Thrombolysis In Myocardial Infarction 3 (n = 1,731) ⁎ | 195 (76%) | 1,188 (81%) | 0.11 |
Of the 2,677 patients, 192 (7.2%) died before hospital discharge. The in-hospital mortality rate was significantly greater in the women than in the men (11.3% vs 6.1%, respectively; p <0.001) and in those aged ≥70 years than aged <70 years (11.7% vs 5.0%, respectively; p <0.001). Of the patients ≥70 years old, in-hospital mortality was significantly greater in women than in men (16.2% vs 9.3%, respectively; p = 0.003; Figure 1 ). However, no significant gender difference in mortality was found among patients <70 years old (5.7% vs 4.9%, p = 0.59).
Female gender was associated with in-hospital mortality in patients ≥70 years old but not those aged <70 years ( Table 3 ). Multivariate analysis (model 2) found that age, Killip class, infarct location, multivessel disease, and final reperfusion were independently associated with in-hospital mortality in patients ≥70 years old. All these variables and previous myocardial infarction were significant in patients <70 years old. On multivariate analysis, the association of female gender and in-hospital mortality remained significant in patients ≥70 years old. However, gender was not a predictor of in-hospital mortality in patients <70 years old.



