The transradial approach is increasingly used for percutaneous coronary intervention (PCI), and we therefore aimed to compare the clinical outcomes after transradial intervention (TRI) and transfemoral intervention (TFI) in all patients undergoing PCI. Among 6,973 patients enrolled in a nationwide, prospective, multicenter registry (February 2013 to September 2013), 1,860 underwent TRI (n = 1,445, 77.7%) and TFI (n = 415, 22.3%). Bleeding and major adverse cardiac events (MACE; death, myocardial infarction, revascularization, or stent thrombosis) were compared. Bleeding occurred in 42 patients (2.3%) and was significantly less likely in the TRI versus TFI group (overall cohort: 1.5% vs 4.8%, p = 0.001; propensity score–matched: n = 728, 2.7% vs 5.2%, p = 0.048). Multivariate regression revealed that TRI was negatively associated with bleeding (odds ratio 0.42, 95% CI 0.21 to 0.83, p = 0.013). MACE occurred in 152 patients (8.2%). Kaplan–Meier estimates showed higher MACE-free survival rates in the TRI versus TFI group (overall cohort: 93.3% vs 86.7%, log-rank p = 0.026; propensity score–matched: 91.8% vs 86.5%, log-rank p = 0.04). Cox proportional analysis demonstrated that TRI independently predicted improved MACE (hazard ratio 0.64, 95% CI 0.43 to 0.91, p = 0.024). In conclusion, TRI is associated with reduced bleeding rates and better clinical outcomes than TFI in all patients undergoing PCI.
The transradial approach has been increasingly adopted for percutaneous coronary intervention (PCI). Recent studies comparing transradial intervention (TRI) with transfemoral intervention (TFI) in patients with acute coronary syndrome (ACS) noted that TRI was associated with significantly lower risks of bleeding, access-site complications, death, and adverse clinical events relative to TFI. Furthermore, the Minimizing Adverse Haemorrhagic Events by TRansradial Access Site and Systemic Implementation of angioX (MATRIX) trial of 8,404 patients with ACS undergoing invasive cardiac procedures through a transradial or transfemoral approach showed that the risks of bleeding, mortality, and net adverse clinical events were reduced significantly in the TRI group. Although almost all precedent studies investigated the prognosis after TRI versus TFI in patients with ACS, data on the clinical outcomes in all patients who underwent PCI are scarce. Therefore, based on the observed clinical benefits of TRI, particularly in patients with ACS undergoing PCI, we evaluated contemporary practice patterns and clinical outcomes after TRI and TFI in the recent antiplatelet era in all eligible patients, including patients with non-ACS, who underwent PCI in a certain prespecified period.
Methods
The study population was selected from the Korea Transradial Coronary Intervention Prospective Registry, a nationwide, prospective, multicenter online registry of patients who have undergone coronary angiography or PCI at 22 university or community hospitals in South Korea since February 2013. This registry is sponsored by the Korean Society of Cardiology, managed by the Transradial Intervention Working Group, and registered with ClinicalTrials.gov ( NCT01803841 ). The participating centers have high volumes of patients and facilities for primary PCI and onsite cardiac surgery. From February 2013 to September 2013, 6,973 consecutive patients who underwent coronary angiography or PCI were prospectively enrolled. All medical data were collected by trained study coordinators using a standardized case report form and protocol. The protocol conformed to the Declaration of Helsinki and was approved by the Human Research Committee of each participating institution. Informed consent was obtained from each patient for using data.
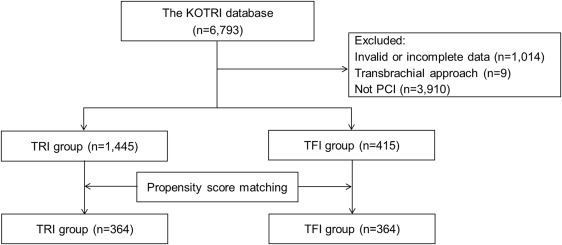
Consecutively hospitalized patients aged ≥19 years who had undergone PCI were included. Patients with invalid or incomplete data (patients aged <19 years, without follow-up, with inaccurate data of the coronary procedure, with dating error, and with a missing value rate >30%), those subjected to a transbrachial approach, and those who did not undergo PCI were excluded. Among all registered patients, 1,860 were included in the analysis. Subjects were divided into 2 groups based on the final successful access site: TRI (n = 1,445; 77.7%) and TFI (n = 415; 22.3%). After propensity score (PS)–matching, 364 patients were included in each group ( Figure 1 ).
Before coronary angiography, an operator, who had experience of at least 100 PCIs and 50 TRIs per year, determined the access site. All patients underwent coronary angiography, if needed, followed by PCI for target lesions under unfractionated heparin or low molecular weight heparin according to the current standard guidelines. During the procedure, patients received unfractionated heparin to maintain an activated clotting time of >250 seconds. Stents were deployed after balloon predilation, and the decision of glycoprotein IIb/IIIa inhibitor use was made at the operators’ discretion. For patients with TRI, hemostasis was achieved with manual compression band mostly or with dedicated devices (RadiStop, TR band, and so on) after radial sheath removal. For patients with TFI, hemostasis was achieved with either manual compression or mostly closure devices (angioseal, percloser, and so on).
Patients were given standard care and medications to prevent secondary events. Each patient received aspirin and clopidogrel or prasugrel or ticagrelor, and cilostazol could be added to clopidogrel by the operator’s discretion in patients at high thrombotic risk. After discharge, all patients were prescribed medications according to current guidelines and followed up at 1 to 3–month intervals. Patients who developed angina-like symptoms underwent complete clinical evaluation. If deemed necessary, the patients received hospital care and revascularization. We collected information about the study end points and the use of the prescribed medications at the follow-up of each patient or by contacting the patients or their relatives by telephone.
The primary end point was cumulative bleeding complications that were unrelated to coronary artery bypass graft (CABG) surgery (types 1 to 3 or 5, as defined by the Bleeding Academic Research Consortium [BARC]), including various types of bleeding (oozing, subcutaneous, retroperitoneal, gastrointestinal, and so on). Secondary end points were major adverse cardiac events (MACE) during follow-up (all-cause death, myocardial infarction [MI], any revascularization [including repeat PCI and CABG], or stent thrombosis). All events were identified by the patient’s physician and confirmed by the principal investigator of each hospital. All-cause death was defined as any death during or after the procedure, and death was considered to be of cardiac origin unless a definite noncardiac cause could be established. MI was defined as symptoms with new electrocardiographic changes compatible with MI or elevated cardiac markers at least 2 times the normal upper limit during the follow-up. Any revascularization was defined as revascularization involving either target or nontarget vessels. Stent thrombosis was defined as evidence of acute myocardial ischemia and documented arterial occlusion at the stent implantation site. Procedural success was defined as a Thrombolysis In Myocardial Infarction flow grade of 2 or 3 in the infarct-related artery and a residual stenosis of <20% in the treated segment at the end of the procedure.
For the statistical analyses, continuous variables are presented as medians with 25th and 75th percentiles, and they were compared using the Mann–Whitney U test. Categorical variables are presented as numbers and percentages, and they were compared using the chi-square or Fisher’s exact test, as appropriate. Multivariate logistic regression was performed to identify independent predictors both for any bleeding including BARC 1 and for BARC 2 or higher bleeding after adjusting for baseline, angiographic, and antithrombotic variables. Age, diabetes mellitus, previous MI, systolic blood pressure, baseline hematocrit, baseline creatine clearance, ST-elevation MI (STEMI), TRI, and aspirin administration were initially chosen both from significant variables after univariate analysis and from other variables which were proved as significant in previous studies. With the rule of thumb with 10 events per variable, important 4 variables according to a total of 42 events in our study were finally selected for multivariate analysis. Kaplan–Meier analyses were used to identify the survival and MACE-free survival between groups in the entire and PS-matched cohorts. Cox proportional hazard models were used to identify the associations of TRI with all-cause death and 1-year MACE. PS was estimated using multivariate logistic regression, with the access-site as the dependent variable and all characteristics in Table 1 as covariates. We matched patients undergoing TRI and TFI in a 1:1 nearest neighbor matching, without replacement and with a caliper width of 0.1. To assess differences in the PS-matched cohort, paired t and McNemar’s tests were used for continuous and categorical variables, respectively. A p value <0.05 was considered significant. Statistical analyses were performed using SPSS 22.0 (SPSS Inc., Chicago, Illinois), and R 3.1.0 (R Development Core Team, Vienna, Austria).
| Variable | Entire cohort (n=1,860) | Propensity score-matched cohort (n=728) | ||||
|---|---|---|---|---|---|---|
| TRI group (n=1,445) | TFI group (n=415) | p | TRI group (n=364) | TFI group (n=364) | p | |
| Age (years) | 67.0 (58.0–74.0) | 68.0 (58.0–75.0) | 0.273 | 68.0 (59.0–75.0) | 69.0 (58.0–76.0) | 0.898 |
| Age >65 years | 821 (56.8%) | 242 (58.3%) | 0.587 | 221 (60.7%) | 217 (59.6%) | 0.832 |
| Men | 1,001 (69.3%) | 273 (65.8%) | 0.177 | 254 (69.8%) | 233 (64.0%) | 0.121 |
| Hypertension | 711 (49.2%) | 218 (52.5%) | 0.118 | 227 (62.4%) | 210 (57.7%) | 0.736 |
| Diabetes mellitus | 349 (24.2%) | 148 (35.7%) | <0.001 | 137 (37.6%) | 130 (35.7%) | 0.630 |
| Dyslipidemia | 221 (15.3%) | 58 (14.0%) | 0.058 | 71 (19.5%) | 52 (14.3%) | 0.203 |
| Current smoker | 660 (45.7%) | 162 (39.0%) | 0.041 | 143 (39.3%) | 145 (39.8%) | 0.832 |
| Prior myocardial infarction | 128 (8.9%) | 48 (11.6%) | 0.071 | 38 (10.4%) | 44 (12.1%) | 0.466 |
| Prior percutaneous coronary intervention | 250 (17.3%) | 109 (26.3%) | <0.001 | 98 (26.9%) | 100 (27.5%) | 0.832 |
| Systolic blood pressure (mmHg) | 130 (117–141) | 130 (110–147) | 0.497 | 130 (116–149) | 130 (112–140) | 0.139 |
| Killip class III/IV | 44 (3.0%) | 23 (5.5%) | 0.016 | 15 (4.1%) | 18 (4.9%) | 0.582 |
| Baseline hematocrit (%) | 41 (37–44) | 39 (34–43) | <0.001 | 38 (34–43) | 41 (36–45) | 0.057 |
| Maximum creatine kinase-MB (μg/l) | 3.3 (1.5–21.3) | 5.6 (1.7–77.6) | 0.004 | 4.49 (1.75–47.50) | 3.92 (1.60–42.14) | 0.854 |
| LDL-cholesterol (mg/dl) | 98.8 (75.0–126.0) | 93.7 (70.6–124.6) | 0.227 | 93.4 (66.6–121.4) | 93.2 (70.6–122.9) | 0.922 |
| Baseline creatinine (mg/dl) | 0.9 (0.8–1.1) | 0.95 (0.8–1.28) | <0.001 | 0.93 (0.81–1.10) | 0.95 (0.80–1.29) | 0.218 |
| Baseline eGFR (mL/min/1.73 m 2 ) | 81.0 (62.3–96.9) | 67.4 (43.8–91.7) | 0.118 | 66.1 (44.7–94.5) | 69.2 (51.7–93.9) | 1.000 |
| Left ventricular ejection fraction (%) | 60.0 (52.0–65.0) | 56.0 (48.3–62.8) | <0.001 | 58.5 (49.8–64.0) | 57.0 (49.0–63.0) | 0.207 |
| Clinical diagnosis | ||||||
| Atypical chest pain | 99 (6.9%) | 30 (7.2%) | 0.101 | 25 (6.9%) | 26 (7.1%) | 0.218 |
| Stable IHD | 453 (31.3%) | 111 (26.7%) | 0.009 | 112 (30.8%) | 105 (28.8%) | 0.549 |
| Acute coronary syndrome | 893 (61.8%) | 274 (66.0%) | 0.002 | 227 (62.4%) | 233 (64.0%) | 0.967 |
| Unstable angina | 561 (38.8%) | 132 (31.8%) | 0.028 | 123 (33.8%) | 125 (34.3%) | 0.812 |
| Non-STEMI | 201 (13.9%) | 67 (16.1%) | 0.203 | 54 (14.8%) | 57 (15.7%) | 0.670 |
| STEMI | 131 (9.1%) | 75 (18.1%) | <0.001 | 50 (13.7%) | 51 (14.0%) | 0.944 |
| Number of coronary artery narrowed | ||||||
| 1 | 593 (41.0%) | 152 (36.6%) | 0.111 | 137 (37.6%) | 143 (39.3%) | 0.606 |
| 2 | 485 (33.6%) | 125 (30.1%) | 0.195 | 118 (32.4%) | 111 (30.5%) | 0.611 |
| 3 | 340 (23.5%) | 135 (32.5%) | <0.001 | 107 (29.4%) | 108 (29.7%) | 0.897 |
| Multiple treated arteries (≥2) | 231 (16.0%) | 100 (24.1%) | 0.399 | 78 (21.4%) | 84 (23.1%) | 0.542 |
| Multiple stents (≥2) | 223 (15.4%) | 109 (26.3%) | 0.025 | 72 (19.8%) | 90 (24.7%) | 0.482 |
| Number of DES | 1,429 (98.9%) | 403 (97.1%) | 0.462 | 358 (98.4%) | 359 (98.6%) | 0.351 |
| Procedural success rate | 1,439 (99.6%) | 409 (98.6%) | 0.110 | 361 (99.2%) | 362 (99.5%) | 0.214 |
| Antithrombotics | ||||||
| Aspirin | 1,443 (99.9%) | 414 (99.8%) | 0.483 | 364 (100%) | 364 (100%) | 0.500 |
| Clopidogrel | 1,358 (94.0%) | 345 (83.1%) | 0.467 | 328 (90.1%) | 325 (89.3%) | 0.399 |
| Prasugrel | 53 (3.7%) | 52 (12.5%) | <0.001 | 24 (6.6%) | 28 (7.7%) | 0.575 |
| Ticagrelor | 33 (2.3%) | 18 (4.3%) | 0.021 | 12 (3.3%) | 11 (3.0%) | 0.875 |
| Cilostazol | 109 (7.5%) | 36 (8.7%) | 0.390 | 41 (11.3%) | 33 (9.1%) | 0.385 |
| Unfractionated heparin | 1,130 (78.2%) | 345 (83.1%) | <0.001 | 303 (83.2%) | 302 (83.0%) | 0.578 |
| Low molecular weight heparin | 315 (21.8%) | 70 (16.9%) | 0.096 | 61 (16.8%) | 62 (17.0%) | 0.659 |
| Glycoprotein IIb/IIIa inhibitor | 41 (2.8%) | 44 (10.6%) | <0.001 | 23 (6.3%) | 25 (6.9%) | 0.750 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


