Although octogenarians are increasingly referred for percutaneous coronary intervention (PCI), data are lacking on long-term safety and efficacy of drug-eluting stents in this high-risk subpopulation. The aim of this study was to evaluate 5-year clinical outcome of octogenarians who underwent PCI using sirolimus-eluting stents (SESs) or paclitaxel-eluting stents (PESs) compared to bare-metal stents (BMSs). From January 2000 to December 2005, 319 consecutive octogenarian patients who underwent PCI with BMSs (n = 93, January 2000 to April 2002), SESs (n = 52, April 2002 to February 2003), or PESs (n = 174, February 2003 to December 2005) were included prospectively. Primary study end points were all-cause mortality and major adverse cardiac events (MACEs), defined as all-cause death, any myocardial infarction, or any revascularization. Mean age of the study population was 83 ± 2 years and 51% of patients were men. Median follow-up duration was 5.4 years (range 3 to 9). Five-year mortality rates in the BMS, SES, and PES cohorts were similar (41%, 42%, and 41%, respectively). Cumulative 5-year MACE-free survival in the BMS, SES, and PES cohorts were 44%, 52%, and 48%, respectively. Compared to the BMS cohort, adjusted hazard ratios for MACEs in the SES and PES cohorts were 0.5 (95% confidence interval [CI] 0.3 to 0.9, p <0.05) and 0.5 (95% CI 0.2 to 1.4, p = 0.2), respectively. Overall, use of drug-eluting stents was associated with fewer MACEs (adjusted hazard ratio 0.5, 95% CI 0.3 to 0.9, p <0.05) and a trend toward less target vessel revascularization (adjusted hazard ratio 0.5, 95% CI 0.2 to 1.2, p = 0.1). In conclusion, PCI with drug-eluting stents in octogenarians was found to be safe and more effective compared to PCI with BMSs.
Octogenarians constitute the fastest growing segment of the population in the Western world. Octogenarians are characterized by a high prevalence of coronary artery disease and a growing number of octogenarians are undergoing coronary revascularization. The initial American Heart Association/American College of Cardiology guidelines noted that the very elderly constituted a special patient population who are developing increased in-hospital complications and mortality. Nevertheless, octogenarians are increasingly referred for percutaneous coronary intervention (PCI) using bare-metal stents (BMSs) or drug-eluting stents. Although randomized trials have shown that drug-eluting stents have significantly decreased the incidence of in-stent restenosis and need for repeat revascularizations in the overall population with various clinical indications, very elderly patients were not adequately represented in these studies. There is a paucity of data on long-term safety and efficacy of drug-eluting stents pertaining specifically to octogenarians undergoing PCI. Therefore, the aim of this study was to evaluate 5-year clinical outcomes of octogenarians who underwent PCI with unrestricted use of sirolimus-eluting stents (SESs) or paclitaxel-eluting stents (PESs) compared to BMSs in a “real-world” experience.
Methods
From January 1, 2000 to December 31, 2005, 7,217 PCIs were performed in Erasmus University Medical Center (Rotterdam, The Netherlands) using BMSs, SESs, or PESs. From January 2000 to April 16, 2002, 2,681 PCIs were performed using exclusively BMSs, and from April 16, 2002 to February 23, 2003, 1,035 interventions were performed using SESs (Cypher, Cordis Corp., Johnson and Johnson, Warren, New Jersey), as part of the Rapamycin-Eluting Stent Evaluated At Rotterdam Cardiology Hospital (RESEARCH) registry, and from February 23, 2003 to December 31, 2005, 3,339 interventions using PESs (Taxus Express or Liberté, Boston Scientific, Natick, Massachusetts), as part of the Taxus-Stent Evaluated at Rotterdam Cardiology Hospital (T-SEARCH) registry. Procedures in which 2 different types of stents (BMS and SESs or PESs; SESs and BMSs or PESs; PESs and SESs or BMSs) were used were excluded (n = 162). Although 784 underwent multiple procedures, only patients initially enrolled in 1 of the sequential cohorts (BMS, SES, or PES group) were maintained for analytic purposes throughout the follow-up period in their original cohort, even if a repeat intervention was performed using a different type of stent. From the 6,129 patients who fulfilled these criteria, we identified 319 octogenarians who were included in this study.
Angina pectoris was categorized according to the Canadian Cardiovascular Society classification for stable angina and according to the Braunwald classification for unstable angina. Hypertension was defined as a systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg or based on current use of antihypertensive treatment. Dyslipidemia was classified as a total serum cholesterol level ≥6.2 mmol/L or use of lipid-lowering drugs. All procedures were performed according to previously defined current standard procedural guidelines. Patients were prescribed aspirin plus clopidogrel 75 mg/day (after a loading dose of 300 mg) before or during baseline coronary interventions. Patients treated with BMSs received ≥1 month of clopidogrel, patients treated with SESs received ≥3 months of clopidogrel, and patients treated with PESs received ≥6 months of clopidogrel. All patients were advised to remain on aspirin indefinitely. Baseline, clinical, and procedural characteristics were acquired prospectively by recording the data in a dedicated database.
Primary end points were all-cause mortality and the patient-oriented composite end point of major adverse cardiac events (MACEs) according to Academic Research Consortium definitions, which included all-cause mortality, any myocardial infarction, and any repeat revascularization. Secondary end points were the composite end point of all-cause mortality or any myocardial infarction (“death/myocardial infarction”), and target vessel revascularization. All-cause mortality and death/myocardial infarction were defined as safety end points, whereas MACEs and target vessel revascularization were defined as efficacy end points. Myocardial infarction was diagnosed by an increase in creatine kinase-MB fraction 3 times the upper limit of normal, together with electrocardiographic changes and symptoms suggestive of ischemia. Repeat revascularization was defined as any PCI or coronary artery bypass grafting during follow-up. Target vessel revascularization was defined as any repeat revascularization of any segment of the target vessel.
In August 2009, the vital status of all patients was acquired from municipal civil registries. Questionnaires were sent to all living patients focusing on the occurrence of MACEs. The referring physician and institutions and the general practitioners were directly approached whenever necessary. Study outcomes were evaluated at 5 years of follow-up.
All data were analyzed with SPSS 15.0 (SPSS, Inc., Chicago, Ilinois). Continuous variables were compared by Student’s t test and are presented as mean ± SD. Categorical variables were compared by chi-square test or Fisher’s exact test, when appropriate, and are presented in percentages. Patients lost to follow-up were considered at risk until the date of last contact, at which point they were censored. Cumulative (event-free) survival was estimated according to the Kaplan-Meier method. Kaplan-Meier survival curves were compared by log-rank test. Univariate and multivariate Cox regression analyses were performed to evaluate SES- and PES-associated outcomes. In multivariate analyses, the following variables were entered into the model: type of stent, age, gender, diabetes mellitus, hypercholesterolemia, previous myocardial infarction, previous coronary artery bypass grafting, previous PCI, clinical presentation, left main/3-vessel coronary disease, calcium antagonist use, statin use, treated coronary vessel, bifurcation, lesion type B2/C, and year of hospital admission. The final results are presented as unadjusted and adjusted hazard ratios (HRs) with associated 95% confidence intervals (CIs). All statistical tests were 2-tailed, where a p value <0.05 was considered statistically significant.
Results
Baseline characteristics of patients in the BMS (n = 93), SES (n = 52), and PES (n = 174) groups are presented in Table 1 . Mean age of the total study population was 83 ± 2 years and 51% were men. Most baseline characteristics were similar among the 3 groups. However, the SES and PES groups consisted of more patients with hypercholesterolemia (p <0.001) compared to the BMS group. Furthermore, more patients with SESs presented with unstable angina, whereas more patients with PESs presented with acute myocardial infarction (p <0.01). None of the included patients presented with cardiogenic shock. At baseline, aspirin use and use of anticoagulants were similar among the 3 groups (91% and 3%, respectively). Statins were more frequently prescribed in patients with SESs and PESs (p <0.001), whereas calcium antagonists were less frequently prescribed compared to patients with BMSs (p <0.001). Procedural characteristics of the BMS, SES, and PES groups are presented in Table 2 . Most procedural characteristics were similar among the 3 groups, although patients with SESs and PESs received stents with a smaller average diameter (p <0.001) and were prescribed clopidogrel for a longer period (p <0.001) than patients with BMSs. Angiographic success rate was similar among the 3 groups (96%).
| Variable | Total (n = 319) | BMS (n = 93) | SES (n = 52) | PES (n = 174) | p Value |
|---|---|---|---|---|---|
| Age (years), mean ± SD | 83 ± 2 | 83 ± 2 | 83 ± 3 | 83 ± 2 | 0.4 |
| Men | 51% | 45% | 58% | 51% | 0.3 |
| Diabetes mellitus | 15% | 17% | 8% | 16% | 0.3 |
| Hypertension ⁎ | 43% | 39% | 44% | 45% | 0.6 |
| Hypercholesterolemia † | 62% | 41% | 60% | 74% | <0.001 |
| Smoker | 9% | 9% | 6% | 10% | 0.7 |
| Family history | 12% | 10% | 10% | 13% | 0.6 |
| Previous myocardial infarction | 33% | 36% | 37% | 31% | 0.7 |
| Previous percutaneous coronary intervention | 25% | 31% | 23% | 21% | 0.2 |
| Previous coronary artery bypass grafting | 19% | 25% | 19% | 15% | 0.1 |
| Left main/3-vessel coronary disease | 40% | 47% | 33% | 38% | 0.2 |
| Presentation | <0.01 | ||||
| Stable angina pectoris | 37% | 39% | 25% | 39% | |
| Unstable angina pectoris | 45% | 50% | 63% | 37% | |
| Acute myocardial infarction | 18% | 11% | 12% | 23% | |
| Cardiogenic shock | 0% | 0% | 0% | 0% | 1.0 |
| Medication use at baseline | |||||
| Aspirin | 91% | 89% | 92% | 91% | 0.8 |
| Oral anticoagulant | 3% | 2% | 6% | 3% | 0.5 |
| Angiotensin converting enzyme inhibitor | 37% | 41% | 33% | 36% | 0.6 |
| β Blocker | 55% | 59% | 58% | 52% | 0.5 |
| Calcium antagonist | 21% | 36% | 21% | 13% | <0.001 |
| Diuretic | 19% | 22% | 21% | 17% | 0.6 |
| Oral nitrate | 11% | 15% | 14% | 8% | 0.1 |
| Statin | 46% | 28% | 42% | 58% | <0.001 |
⁎ Systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg, or based on current use of antihypertensive treatment.
† Dyslipidemia was defined as a total serum cholesterol level ≥6.2 mmol/L or use of lipid-lowering drugs.
| Variable | Total (n = 319) | BMS (n = 93) | SES (n = 52) | PES (n = 174) | p Value |
|---|---|---|---|---|---|
| Coronary vessel treated ⁎ | |||||
| Left main | 7% | 7% | 10% | 6% | 0.7 |
| Left anterior descending | 53% | 56% | 62% | 49% | 0.2 |
| Left circumflex | 34% | 39% | 33% | 32% | 0.5 |
| Right | 35% | 39% | 29% | 35% | 0.5 |
| Saphenous vein graft | 9% | 13% | 8% | 8% | 0.3 |
| American College of Cardiology/American Heart Association lesion type B2/C | 73% | 73% | 73% | 73% | 1.0 |
| Bifurcation | 9% | 7% | 6% | 10% | 0.4 |
| Number of stents, mean ± SD | 2.2 ± 1.5 | 2.2 ± 1.6 | 2.1 ± 1.5 | 2.3 ± 1.5 | 0.7 |
| Total stent length (mm), mean ± SD | 40 ± 29 | 35 ± 27 | 38 ± 25 | 44 ± 31 | 0.1 |
| Stent diameter (mm), mean ± SD | 3.0 ± 0.6 | 3.3 ± 0.7 | 2.9 ± 0.3 | 2.9 ± 0.6 | <0.001 |
| Glycoprotein IIb/IIIa inhibitor | 12% | 16% | 17% | 8% | 0.1 |
| Angiographic success | 96% | 96% | 94% | 96% | 0.8 |
| Clopidogrel (months), mean ± SD | 5.1 ± 4.3 | 2.2 ± 1.6 | 4.6 ± 6.9 | 6.7 ± 3.3 | <0.001 |
Clinical follow-up was available for 99% of patients. Response rate of the questionnaires that were sent to all living patients was 87%. Median follow-up duration was 5.4 years (range 3 to 9). In the total study population, cumulative 30-day survival rate was 92%. Overall cumulative 1-, 3-, and 5-year cumulative survival rates were 83%, 71%, and 59%, respectively.
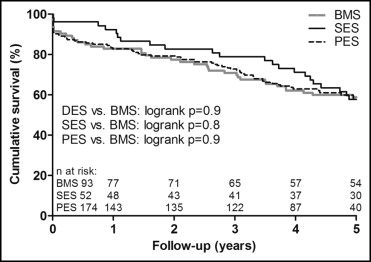
Kaplan-Meier cumulative 5-year survivals were 58% in patients with SESs (log-rank p = 0.8) and 59% in patients with PESs (log-rank p = 0.9) compared to 59% in patients with BMSs ( Figure 1 ). Unadjusted and adjusted HRs of study end points at 5 years are presented in Table 3 . After adjustment in multivariate analysis, all-cause mortality after implantation of SESs (adjusted HR 0.7, 95% CI 0.4 to 1.4) and PESs (adjusted HR 0.6, 95% CI 0.2 to 1.8) were not significantly different from that after BMS implantation. Kaplan-Meier cumulative 5-year death/myocardial infarction-free survivals were 54% in patients with SESs (log-rank p = 0.9) and 56% in those with PESs (log-rank p = 0.9) compared to 58% in those with BMSs ( Figure 2 ). In multivariate analysis, death/myocardial infarction after use of SESs (adjusted HR 0.8, 95% CI 0.4 to 1.6) and PESs (adjusted HR 0.7, 95% CI 0.2 to 2.0) were similar to that after use of BMSs.
| Variable | Univariate | Multivariate ⁎ | ||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Drug-eluting stent compared to bare-metal stent | ||||
| All-cause mortality | 1.0 (0.7–1.4) | 0.9 | 0.7 (0.4–1.4) | 0.3 |
| All-cause mortality or myocardial infarction | 1.0 (0.7–1.5) | 0.8 | 0.8 (0.4–1.6) | 0.6 |
| Major adverse cardiac event | 0.8 (0.6–1.1) | 0.2 | 0.5 (0.3–0.9) | <0.05 |
| Target vessel revascularization | 0.5 (0.3–1.1) | 0.1 | 0.5 (0.2–1.2) | 0.1 |
| Sirolimus-eluting stent compared to bare-metal stent | ||||
| All-cause mortality | 0.9 (0.6–1.6) | 0.8 | 0.7 (0.4–1.4) | 0.3 |
| All-cause mortality or myocardial infarction | 1.0 (0.6–1.7) | 0.9 | 0.8 (0.4–1.6) | 0.6 |
| Major adverse cardiac event | 0.7 (0.4–1.1) | 0.1 | 0.5 (0.3–0.9) | <0.05 |
| Target vessel revascularization | 0.4 (0.1–1.4) | 0.2 | 0.4 (0.1–1.3) | 0.1 |
| Paclitaxel-eluting stents compared to bare-metal stent | ||||
| All-cause mortality | 1.0 (0.7–1.5) | 1.0 | 0.6 (0.2–1.8) | 0.3 |
| All-cause mortality or myocardial infarction | 1.0 (0.7–1.5) | 0.8 | 0.7 (0.2–2.0) | 0.5 |
| Major adverse cardiac event | 0.9 (0.6–1.2) | 0.4 | 0.5 (0.2–1.4) | 0.2 |
| Target vessel revascularization | 0.6 (0.3–1.2) | 0.1 | 0.6 (0.3–1.5) | 0.2 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


