Disparities in the risk of coronary artery disease (CAD) between races may be influenced by differences in the thoracic adipose tissue. We compared computed tomography (CT)–derived volumes of epicardial adipose tissue (EAT), mediastinal adipose tissue (MAT), and pericoronary fat thickness (PFT) and correlations with CAD between black and white patients. This institutional review board–approved Health Insurance Portability and Accountability Act–compliant study included 372 age- and gender-matched black versus white patients (186 black, 54 ± 11 years, 50% men; 186 white, 54 ± 11 years, 50% men) who underwent CT for chest pain evaluation. EAT, MAT, and PFT were measured. The amount of coronary calcium was quantified as calcium score. CAD was defined as ≥50% coronary artery narrowing. EAT and MAT volumes were significantly lower in black than white patients (59 [twenty-fifth to seventy-fifth percentile 39 to 84] vs 97 [67 to 132] cm 3 and 44 [27 to 77] vs 87 [52 to 157] cm 3 , for both p <0.001). Mean PFT in black patients was slightly lower than white patients (17.2 ± 3.2 vs 18.1 ± 3.4 mm, p <0.01). The relation between race and extent of adipose tissue remained significant after adjustment for cardiovascular risk factors. Significant correlations were observed between EAT and MAT volumes and calcium score in black and white patients (r = 0.19 to 0.26, p <0.01). For both races, the level of thoracic fat measurements was higher in present versus absent coronary calcification. A greater amount of thoracic fat was found with obstructive CAD only in white patients. In conclusion, CT-derived measurements of thoracic fat differ between symptomatic black and white patients, suggesting a differential relation between thoracic adipose tissue and CAD pathophysiology by race.
Previous studies have shown a greater prevalence of coronary artery disease (CAD) and disease-specific mortality rates in black than white patients. Recently, atherosclerotic plaque burden and composition, as derived from coronary computed tomography angiography (cCTA), was found to differ between black and white patients, with relatively more noncalcified disease in black patients and more calcified disease in white patients. The pathophysiological explanation for the racial difference in CAD risk needs further elucidation. Differences in thoracic adipose tissue between races may be one of the contributing factors. Thus, the purpose of this study was to compare computed tomography (CT)–derived volumes of epicardial adipose tissue (EAT), mediastinal adipose tissue (MAT), and pericoronary fat thickness (PFT) and correlations with CAD between black and white patients.
Methods
Our institutional review board waived the need for informed consent for this retrospective, Health Insurance Portability and Accountability Act–compliant, matched-cohort study. A total of 372 patients who had undergone cCTA for acute chest pain from October 2006 to April 2010, who had a cCTA study with diagnostic image quality and no previous revascularization (i.e., coronary artery bypass graft or stent), were retrospectively included, with the intent to include equal numbers of black and white patients as well as men and women. One hundred eighty-six were self-identified black with complete clinical and demographic data available. These patients were matched one-on-one with a total of 186 self-identified non-Hispanic white patients with age and gender distributions similar to those of the black patient group and complete data available.
Hypertension was defined as a systolic blood pressure of ≥140 mm Hg, a diastolic blood pressure of >90 mm Hg, or the use of antihypertensive medication. Hypercholesterolemia was defined as a total cholesterol level >200 mg/dl or the use of lipid-lowering medication. Diabetes was defined as a fasting blood glucose level of ≥126 mg/dl or a requirement for insulin or oral hypoglycemic agents. Body mass index (BMI) was calculated from self-reported height and weight, and if either height or weight was missing, BMI was derived from the hospital information system.
All subjects first underwent unenhanced, prospectively electrocardiographically triggered cardiac CT with 120 kV, 145 mA, and 1.2-mm collimation. Images were obtained at 40% or 70% of the RR interval depending on heart rate and were reconstructed with a medium-sharp convolution kernel, 3-mm section width, and 50% reconstruction increment.
Subsequently, retrospectively electrocardiographically gated, contrast material–enhanced cCTA was performed using a dual-source CT system (Somatom Definition; Siemens Medical Solutions, Forchheim, Germany) during end-inspiration. Electrocardiogram-dependent tube current modulation was used in all patients. Detector collimation was 64 × 2 × 0.6 mm and gantry rotation time was 330 ms (temporal resolution, 83 ms). No pharmacologic heart rate control was used. For the cCTA examinations, 60 to 80 ml of iopromide (370 mgI/ml Ultravist; Bayer, Wayne, New Jersey) was followed by 30 ml of saline solution, injected intravenously at 6 ml/s by way of a dual-syringe injector (Stellant D; Medrad, Indianola, Pennsylvania).
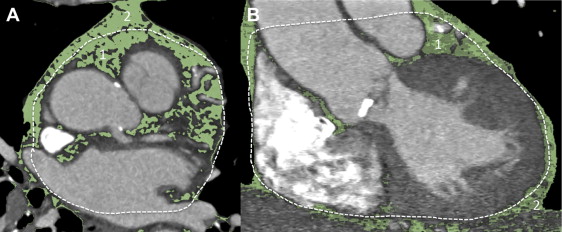
EAT volume, MAT volume, and PFT were assessed by a single observer (PA, with 5 years of experience in cardiac CT). The observer was blinded to clinical history, coronary artery calcium (CAC) score, and cCTA result. The superior extent for the thoracic fat measurements was defined as the center of the right pulmonary artery and the inferior extent as the end of the pericardial sac. EAT, defined as the adipose tissue within the visceral layer of the pericardium, was quantified by manually tracing the pericardium on 3 to 4 axial cCTA sections. Automated software (Volume; Siemens Medical Solutions) interpolated between the traced sections; if needed, the pericardial tracings were manually adjusted. A predefined threshold of −195 to −45 H was applied to identify voxels consisting of fat. These voxels were summed to obtain EAT volume in milliliters. MAT was determined using the same superior and inferior borders. However, the anterior border of the MAT volume was defined by the chest wall (sternum) and the posterior border by the ribs and vertebral column. After manually tracing the chest wall on 3 to 4 axial cCTA sections, the software automatically interpolated between the traced sections using the same predefined thresholds described previously. This resulted in total intrathoracic fat volume. Subsequently, EAT volume was subtracted from intrathoracic fat volume to obtain MAT volume. Figures 1 and 2 show examples of EAT and MAT volume quantification.
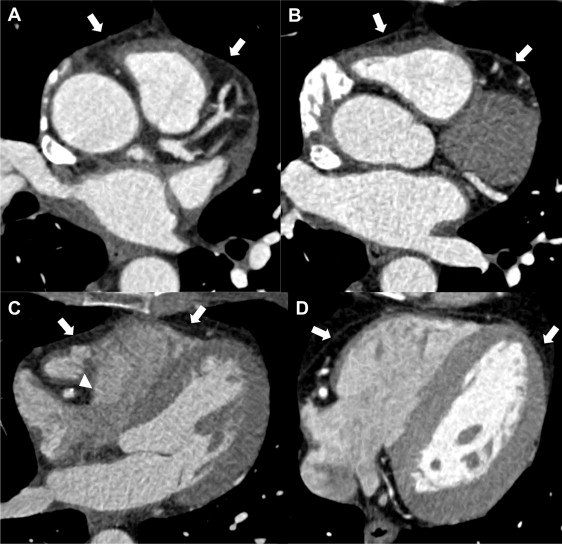
Pericoronary fat was defined as the adipose tissue between the surface of the heart and the visceral epicardium directly surrounding the right coronary artery. PFT of the right coronary artery was defined as the largest distance from myocardium to visceral epicardium and measured on reconstructed sections orthogonal to the vessel centerline at the proximal, mid, and distal segments of the right coronary artery. The mean of the 3 measurements (referred to as PFT) was used for analyses.
Quantification of CAC was performed by 1 experienced reader, unaware of cCTA results and fat measurements, on an off-line workstation using a dedicated software for calcium scoring (CaScore; Siemens Medical Solutions). Calcified lesions were identified as areas in the coronary arteries with attenuation of ≥130 H on noncontrast CT studies. The CAC score was computed by multiplying the area of each lesion by a weighing factor depending on the peak attenuation in the lesion. The scores of individual lesions were summed to obtain a global CAC score of all coronary vessels.
The reconstructed data sets were transferred to an off-line workstation (MultiModality Workplace; Siemens Healthcare, Forchheim, Germany) and analyzed by 2 experienced investigators (PA and UJS with 5 and 15 years of experience reading cCTA, respectively), blinded to the clinical and racial information. Stenosis was defined as any lesion that obstructed ≥50% of the vessel diameter. The presence of plaque, whether obstructive, was also noted. These findings were analyzed on a per-patient basis.
Analyses were performed for all patients and then by race (black and white). The Kolmogorov-Smirnov test was used to evaluate whether continuous variables had a normal distribution. Continuous variables are expressed as mean ± SD, except for nonnormally distributed variables, which are expressed as median (twenty-fifth to seventy-fifth percentile). Categorical variables are expressed as frequencies or percentages. Differences in continuous variables were tested by the independent-samples t test (normal distribution) or by the Mann-Whitney U test (nonnormal distribution). For categorical variables, the chi-square test was used. Correlations between age and thoracic fat measurements, between BMI and thoracic fat measurements, and between thoracic fat measurements and CAC score were assessed by Spearman’s correlation coefficient. In a generalized linear model, we evaluated the association between race and level of thoracic fat measurements, adjusted for age, gender, and BMI (model 1) and additionally adjusted for cardiovascular risk factors (model 2). BMI was categorized into <25, ≥25 to <30, ≥30 to <35, and ≥35 kg/m 2 . Differences in the level of thoracic fat measurements by BMI categories were tested by the Kruskal-Wallis test. Logistic regression analysis adjusted for age, gender, and BMI, and then additionally adjusted for cardiovascular risk factors, was performed to evaluate the relation between thoracic fat measurements and positive CAC score, obstructive CAD, and the presence of plaque as outcomes. Statistical analyses were performed using commercially available software (SPSS 20; SPSS, Chicago, Illinois). All p values were 2-sided. A p value of <0.05 was considered statistically significant.
Results
Table 1 lists the characteristics of the study population. The patient cohort consisted of 372 patients with acute chest pain (equal numbers of black and white as well as male and female patients). Mean age of the black and white patient group was equal, 54 ± 11 years. The mean BMI was 31 ± 7 kg/m 2 for black patients and 30 ± 6 kg/m 2 for white patients (p = NS). Risk factor levels by race were similar, except for diabetes mellitus and hypertension, which were more common in black patients.
| Variable | All Patients (n = 372) | Black Patients (n = 186) | White Patients (n = 186) | p Value ∗ |
|---|---|---|---|---|
| Age (yrs) | 54.1 ± 10.9 | 53.9 ± 11.2 | 54.4 ± 10.7 | NS |
| Men | 186 (50.0) | 93 (50.0) | 93 (50.0) | NS |
| Diabetes mellitus | 87 (23.4) | 55 (29.6) | 32 (17.2) | <0.01 |
| Smoker | 129 (34.7) | 70 (37.6) | 59 (31.7) | NS |
| Hypertension † | 261 (70.2) | 140 (75.3) | 121 (65.1) | <0.05 |
| Hypercholesterolemia ‡ | 178 (47.8) | 81 (43.8) | 97 (52.2) | NS |
| BMI (kg/m 2 ) | 30.2 ± 6.9 | 30.7 ± 7.3 | 29.6 ± 6.4 | NS |
| DF-CASS pretest probability | 27 (14–51) | 22 (12–51) | 31 (14–51) | NS |
∗ p Value for test of difference between black and white patients.
† Hypertension: systolic blood pressure ≥140 mm Hg, diastolic blood pressure >90 mm Hg, or the use of antihypertensive medication.
‡ Hypercholesterolemia: total cholesterol level >200 mg/dl or the use of lipid-lowering medication.
EAT and MAT volumes and PFT were significantly lower in black patients than white patients ( Table 2 ). EAT and MAT volumes were significantly correlated in both races, with r = 0.56 for black and 0.42 for white patients (p <0.001). Only in black patients, thoracic fat volumes were correlated with age (EAT: r = 0.24, p <0.01, MAT: r = 0.23, p <0.01). In both races, levels of thoracic fat measurements were significantly higher in men and patients with diabetes mellitus (except for MAT in white patients) and hypertension. No association was found with current smoking. The relation between race and extent of thoracic adipose tissue remained significant after adjustment for age, gender, and BMI and after additional adjustment for cardiovascular risk factors (data not shown).
| Variable | All Patients (n = 372) | Black Patients (n = 186) | White Patients (n = 186) | p Value |
|---|---|---|---|---|
| EAT ∗ | 77 (47–108) | 59 (39–84) | 97 (67–132) | <0.001 |
| MAT ∗ | 65 (32–115) | 44 (27–77) | 87 (52–157) | <0.001 |
| PFT † | 17.6 ± 3.4 | 17.2 ± 3.2 | 18.1 ± 3.4 | <0.01 |
∗ Median values (twenty-fifth to seventy-fifth percentile) in cm 3 .
BMI correlated with thoracic fat measurements in both races. Correlation coefficients were higher in white patients (for EAT and MAT: r = 0.35, p <0.001 and r = 0.42, p <0.001, respectively) than black patients (r = 0.23, p <0.01 and r = 0.26, p <0.001, respectively). Thoracic fat measurements differed by BMI category ( Figure 3 , p <0.05), except for EAT in black patients. Correlations between BMI and thoracic fat measurements were stronger in white patients. For each BMI category, median values of thoracic fat measurements were significantly lower for black than white patients (p <0.05).
Table 3 lists the presence and extent of coronary atherosclerosis. The percentage of black patients with coronary calcification was slightly, but nonsignificantly, lower than that of white patients (43.2% vs 51.7%), whereas the overall median CAC score was similar. Nearly 18% of black patients had significant stenosis at cCTA versus 23.7% of the white patients (p >0.05).
| Variable | All Patients (n = 372) | Black Patients (n = 186) | White Patients (n = 186) | p Value |
|---|---|---|---|---|
| Calcium score >0 (%) | 168 (47.5) | 76 (43.2) | 92 (51.7) | NS |
| Calcium score (Agatston units) | 0 (0–100) | 0 (0–76) | 2.5 (0–117) | NS |
| Significant stenosis (%) | 77 (20.7) | 33 (17.7) | 44 (23.7) | NS |
| Presence of plaque at cCTA (%) | 234 (62.9) | 119 (64.0) | 115 (61.8) | NS |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


