Conventional coronary angiography (CA) with static imaging is limited by the ability to properly select the optimal acquisition angle, vessel foreshortening, and significant radiation exposure. Rotational coronary angiography (RA) acquires coronary images in a multitude of viewing angles during a single injection by means of a moving gantry that rapidly completes a predefined arc. This study compares procedural characteristics of CA and RA. Electronic search of databases such as OVID, Medline, and PubMed was conducted to identify studies comparing procedural characteristics of CA and RA. End points for analysis included contrast volume, radiation dose by dose area product, radiation dose by air kerma, fluoroscopy time, and procedure time. Studies were assessed for quality and bias and were included if they compared coronary imaging of both the right and left coronary systems with CA and RA, included one of the end points of interest, and were in English. A total of 11 studies consisting of 940 patients who underwent RA and 976 who underwent CA were included in the final analysis. Contrast volume, radiation dose by dose area product, and radiation dose by air kerma were all found to be significantly lower with RA compared with CA. There was a statistically significant increase in fluoroscopy time, although this was not clinically significant, and there was no difference in procedure time. RA angiography is a feasible alternative to CA and offers reductions in contrast used and radiation exposure.
Angiography remains the gold standard in imaging the coronary arteries for evaluation of stenosis and obstruction. Conventional coronary angiography (CA), consisting of static imaging of the coronary arteries, lacks standardized acquisition protocols and instead relies on operator-dependent decisions in real time to determine optimal imaging angles. Contrast agents used for angiography may also be harmful. In general, 3 to 4 images of the left coronary artery and 2 to 3 images of the right coronary artery are obtained; these multiple images, however, still may not contain the optimal angle. Rotational coronary angiography (RA), both single and dual axis, may help overcome the limitations of CA. RA acquires a cine of the coronary artery injection as the gantry rapidly moves through a predefined arc. With single-axis RA, the arc is repeated twice, once with cranial angulation and once with caudal angulation, whereas with dual-axis RA does this in 1 motion. This analysis pools data from previous studies to compare the procedural characteristics of CA and RA.
Methods
A systematic review of the literature was performed to identify reports describing comparisons between RA and CA. This was a newly conducted review with no previous review protocol having been established for it. The aim of the study was to compare procedural characteristics of RA and CA using the following outcomes: contrast volume, total radiation as dose area product (DAP), total radiation as air kerma, total fluoroscopy time, and total procedure time. Contrast volume was defined as volume of contrast used for the entire case, including any contrast used in additional to the CA. Total procedure time was defined as the time between administration of local anesthesia for vascular access until all catheters were removed. Procedure time was analyzed in seconds as was fluoroscopy time. Contrast volume is presented in milliliters, DAP in gray per square centimeter, kerma in milligray, total fluoroscopy time in seconds, and total procedure time in seconds.
Reports were identified using electronic databases including PubMed, EMBASE, and Ovid, which were queried using one of the following terms “rotational,” “single axis,” “dual axis,” and “swing” in combination with one of the following terms “coronary angiography,” “angiography,” and “angioplasty.” No specific restriction on year of publication was used. Reports were initially screened by title and abstract with full text being retrieved for only selected reports.
These full-text reports were then reviewed by 2 of the investigators and assessed for quality and bias (RSL and ME). Any disparities in scoring of reports were then independently reviewed by another author (SA). The Cochrane Handbook for Systematic Review was used for quality evaluation.
Criteria for inclusion consisted of studies published in English comparing RA and CA. The study must have included at least one of the aforementioned end points of interest for both RA and CA. Data for the end points had to have included either a mean or median, SD or range, and number of patients in each group. Studies not meeting these criteria were excluded.
Next, data regarding baseline patient characteristics and identified outcomes were extracted from the reports identified for inclusion. Trial level data were extracted independently using a data collection form by the following 2 investigators, MB and RSL. The data extraction was then independently reviewed by another author (SA) to ensure integrity of the resulting data. If no information was available about particular outcomes, this was designated separately. Authors of included studies were not contacted for additional data.
Bias was assessed using the Cochrane Risk of Bias assessment tool. Specifically, patient eligibility, randomization and concealment of allocation, blinding, completeness of outcome data, and statistical integrity were assessed using this scale. Publication analysis was assessed for end points for which data from ≥10 studies was pooled using funnel plots.
Sensitivity analyses were conducted for each end point based on study size, publication date, single- versus dual-axis RA.
Numeric data are presented as means with SDs or medians with ranges. Categorical data are presented as frequencies with absolute numbers and percentages. p Values ≤0.05 were considered statistically significant. This analysis was done using SPSS Statistical Software, version 20.0 (Chicago, Illinois). Meta-analysis and forest plot creation were done using RevMan 5.0 (Cochrane Collaboration, Oxford, United Kingdom). Results are presented as pooled odds ratios with 95% confidence intervals (CIs) or as standard mean difference where appropriate. Heterogeneity between studies was identified using the chi-square and I 2 tests. For outcomes with no significant heterogeneity present, a fixed-effects model was used. Otherwise a random-effects model was used if either the p value was significant or the I 2 statistics was >50%.
The studies included both randomized studies in which patients were randomly assigned to undergo coronary angiography using a rotational or conventional protocol and studies in which all included patients underwent both RA and CA with subsequent comparison of the 2 methods. Analysis was initially run with all studies for each respective end point and then repeated with only data from randomized controlled trials if that was not the case for the initial analysis.
Results
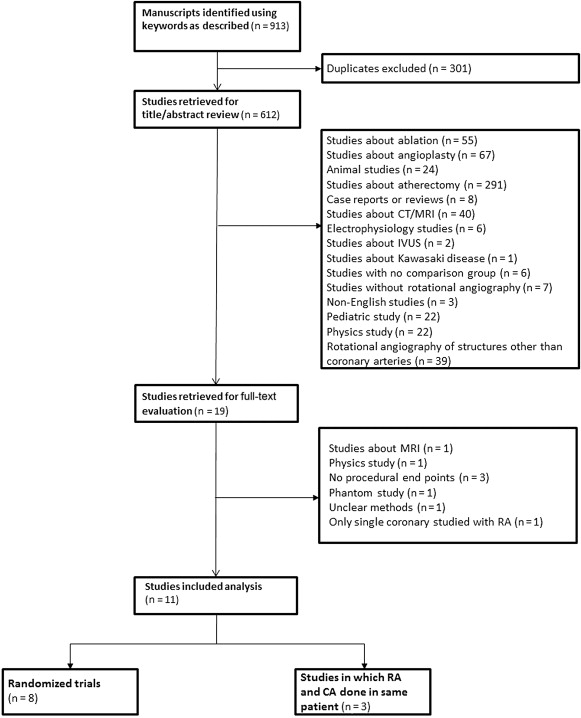
A total of 913 reports were initially identified with 612 remaining after removal of duplicates. Abstracts for these 612 reports were reviewed, and after elimination of animal studies, case reports, reviews, non-English studies, and studies not pertaining to RA, a total of 19 reports were identified for full-text evaluation. No direct contact with the authors was required to obtain full-text reports. Studies without procedural end points, with only a single rotational coronary artery injection done, based on magnetic resonance imaging, presenting phantom data, and with unclear methods were eliminated leaving a total of 11 studies. Of these 11 studies, 8 were randomized trials in which patients underwent either RA or CA and 3 were studies in which all patients underwent both RA and CA ( Figure 1 ).
A total of 1,916 patients were included in this analysis from the 11 included studies with 940 patients having undergone RA and 976 having undergone CA. It should be noted that not all patients from the study by Klein et al were included, with only 21 patients who underwent RA of both the right and left coronary circulations being included in the pooled analysis ( Table 1 ).
| First author | Year | Study Design | Rotational angiography (n) | Conventional angiography (n) | Rotational angiography age (Years) | Conventional angiography age (Years) |
|---|---|---|---|---|---|---|
| Maddux | 2004 | Randomized | 28 | 28 | 57.9 | 59.5 |
| Akhtar | 2005 | Randomized | 25 | 25 | 63.3 ± 9.7 | 62.0 ± 13.2 |
| Garcia | 2009 | Patients underwent both | 100 | 100 | 62.0 ±12.0 | 62.0 ± 12.0 |
| Empen | 2010 | Patients underwent both | 207 | 207 | — | — |
| Klein | 2011 | Patients underwent both | 30 | 30 | — | — |
| Gomez-Menchero | 2012 | Randomized | 52 | 52 | 64.0 ± 11.0 | 67.0 ± 11.0 |
| Liu | 2012 | Randomized | 100 | 100 | 58.21 ± 9.92 | 56.95 ± 9.37 |
| Grech | 2012 | Randomized | 216 | 247 | — | — |
| Eloot | 2013 | Randomized | 40 | 40 | 65.8 ± 15.9 | 63.3 ± 10.7 |
| Yasar | 2013 | Randomized | 56 | 61 | 60.9 ± 9.4 | 58.3 ± 11.9 |
| Giuberti | 2014 | Randomized | 101 | 100 | 54.8 ± 4.3 | 57.0 ± 3.5 |
Mean age across the studies ranged from 56.9 to 67.0 years in the CA group and 54.8 to 65.8 years in the RA group. There was no statistically significant difference in patient characteristics between studies ( Table 1 ).
Included studies were all found to have low overall levels of bias based on the Cochrane Risk of Bias Assessment Tool. The 3 studies in which all included patients underwent both conventional and RA were given a high level of risk in respect to selection bias but otherwise had low risk of other bias ( Table 2 ). Publication bias was assessed for contrast volume and total radiation dose expressed as DAP with no significant publication bias being appreciated for either end point. As <10 studies were pooled for the remainder of the end points, publication bias was not formally assessed using funnel plots.
| First author | Random Sequence generation (selection bias): Risk | Allocation concealment (selection bias): Risk | Blinding of participants and personnel (performance bias): Risk | Blinding of outcome assessment (detection bias): Risk | Incomplete outcome data (attrition data): Risk | Selective reporting (reporting bias): Risk | Other bias: Risk |
|---|---|---|---|---|---|---|---|
| Maddux | Low | Low | Low | Low | Low | Low | Low |
| Akhtar | Low | Low | Low | Low | Low | Low | Low |
| Garcia | High | Low | Unknown | Low | Low | Low | Low |
| Empen | High | Low | Unknown | Low | Low | Low | Low |
| Klein | High | Low | Unknown | Low | Low | Low | Low |
| Gomez-Menchero | Low | Low | Low | Low | Low | Low | Low |
| Liu | Low | Low | Low | Low | Low | Low | Low |
| Grech | Low | Low | Low | Low | Low | Low | Low |
| Eloot | Low | Low | Low | Low | Low | Low | Low |
| Yasar | Low | Low | Low | Low | Low | Low | Low |
| Giuberti | Low | Low | Low | Low | Low | Low | Low |
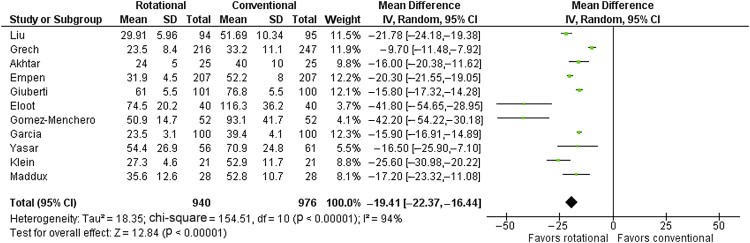
Data from a total of 11 studies were pooled for analysis of contrast volume with a total of 940 patients in the RA group and 976 patients in the CA group. There was a significant difference with respect to contrast volume between the 2 groups with a pooled mean difference of −19.4 ml (95% CI −22.37 to −16.44, p <0.001) favoring RA. A random-effect model was used as there was significant heterogeneity present. When the analysis was repeated with only the randomized trials, there were similar findings ( Figure 2 ).
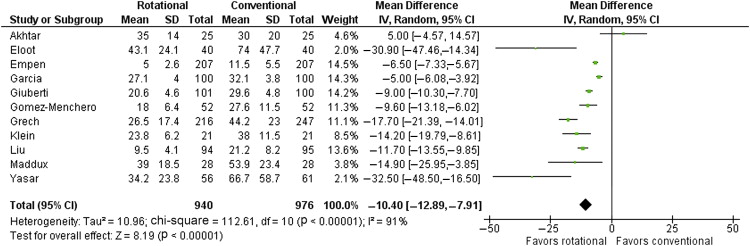
Data from a total of 11 studies were pooled for analysis of total radiation dose represented by DAP with a total of 940 patients in RA group and 976 patients in the CA group. There was a significant difference with respect to DAP between the 2 groups with a pooled mean difference of −10.40 Gycm −2 (95% CI −12.89 to −7.91, p <0.001) favoring RA. A random-effects model was used as there was significant heterogeneity present ( Figure 3 ). When the analysis was repeated with only the randomized trials, there were similar findings.