The evaluation of the aortic root in patients referred for transcatheter aortic valve implantation is crucial. The aim of the present study was to compare the accuracy of cardiac magnetic resonance (CMR) evaluation of the aortic annulus (AoA) with transthoracic and transesophageal echocardiography and multidetector computed tomography (MDCT) in patients referred for transcatheter aortic valve implantation. In 50 patients, maximum diameter, minimum diameter and AoA, length of the left coronary, right coronary, and noncoronary aortic leaflets, degree (grades 1 to 4) of aortic leaflet calcification, and distance between AoA and coronary artery ostia were assessed. AoA maximum diameter, minimum diameter, and area by CMR were 26.4 ± 2.8 mm, 20.6 ± 2.3 mm, 449.8 ± 86.2 mm 2 , respectively. The length of left coronary, right coronary, and noncoronary leaflets by CMR were 13.9 ± 2.2, 13.3 ± 2.1, and 13.4 ± 1.8 mm, respectively, whereas the score of aortic leaflet calcifications was 2.9 ± 0.8. Finally, the distances between AoA and left main and right coronary artery ostia were 16.1 ± 2.8 and 16.1 ± 4.4 mm, respectively. Regarding AoA area, transthoracic and transesophageal echocardiography showed an underestimation (p <0.01), with a moderate agreement (r: 0.5 and 0.6, respectively, p <0.01) compared with CMR. No differences and excellent correlation were observed between CMR and MDCT for all parameters (r: 0.9, p <0.01), except for aortic leaflet calcifications that were underestimated by CMR. In conclusion, aortic root assessment with CMR including AoA size, aortic leaflet length, and coronary artery ostia height is accurate compared with MDCT. CMR may be a valid imaging alternative in patients unsuitable for MDCT.
Accurate measurement of the aortic annulus (AoA) is essential for appropriate valve sizing in transcatheter aortic valve implantation (TAVI). Measurement of AoA before and during TAVI has been traditionally and most commonly performed using transthoracic (TTE) and transesophageal (TEE) echocardiography. However, multidetector computed tomography (MDCT) has distinct advantages such as exceptional spatial resolution and multiplanar reformatting capabilities over 2-dimensional echocardiography and has demonstrated to be a feasible and accurate imaging method for the evaluation of the aortic root morphology and dimensions that may influence or modify TAVI strategy in a considerable number of cases. Unfortunately, up to 20% of patients undergoing TAVI have clinical conditions that make them unsuitable candidates for MDCT. Moreover, MDCT requires contrast agent administration that may be a hazard issue in patients with reduced kidney function who are a substantial proportion of patients undergoing TAVI. Cardiac magnetic resonance (CMR) may provide similar 3-dimensional (3D) multislice images of the aortic root without the administration of contrast agents and may be a valid alternative to MDCT. However, only a few data are available regarding its accuracy compared with MDCT. Thus, the aim of this study was to assess feasibility and accuracy of CMR compared with MDCT for the evaluation of AoA, aortic leaflets length, and AoA-coronary artery ostia distance in patients referred for TAVI.
Methods
From January 2011 to June 2012, 80 consecutive patients with severe aortic stenosis were referred to our institute for TAVI. Exclusion criteria were severely impaired renal function (creatinine clearance <30 ml/min; 4 patients); inability to sustain a 10-second breath hold (2 patients), atrial fibrillation, or other cardiac arrhythmias (9 patients); presence of pacemaker or intracardiac defibrillator (10 patients); and claustrophobia (5 patients). According to the exclusion criteria, a total of 50 patients were included in the study (27 men, mean age 79.62 ± 7.52 years, logistic EuroSCORE 22.4 ± 8). Written informed consent was obtained from all patients, and the study protocol was approved by the local ethical committee.
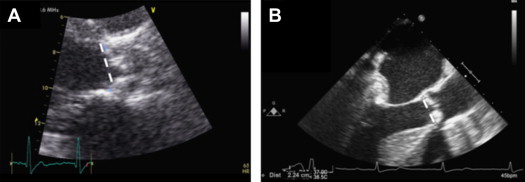
TTE was obtained with patients in the left lateral decubitus position using a commercially available system (IE33 system; Philips Medical System, Andover, Massachusetts) in the parasternal (long- and short-axis) and apical (2- and 4-chamber) views at baseline. For each patient, end-diastolic and end-systolic left ventricle volumes were measured. Left ventricular ejection fraction was calculated by echocardiography biplane Simpson’s rule. The severity of aortic stenosis was assessed with the peak and mean aortic gradients, whereas the aortic valve area was calculated with the continuity equation. The aortic stenoses were graded according to the American College of Cardiology/American Heart Association guidelines. Regurgitation of the mitral and aortic valves was graded as none (grade 0), mild (grade 1), mild to moderate (grade 2), moderate (grade 3), or severe (grade 4) according to published guidelines. Measurement of the AoA diameter with TTE was performed in systole in a parasternal long-axis view on the left ventricular outflow tract (LVOT) at the points of insertion of the right and noncoronary aortic leaflets ( Figure 1 ). The AoA area by TTE was estimated using the following equation: (AoA − diameter/2) 2 × Π with the assumption that the AoA had a circular configuration. All patients underwent TEE (IE33 system; Philips Medical System, Andover, Massachusetts) with a multiplane probe in the midesophageal position at 110° to 135° for full visualization of the AoA. TEE measurements of AoA diameter and area ( Figure 1 ) were obtained in the same way as described for TTE. TTE was repeated after TAVI before patient discharge and at 1 month.
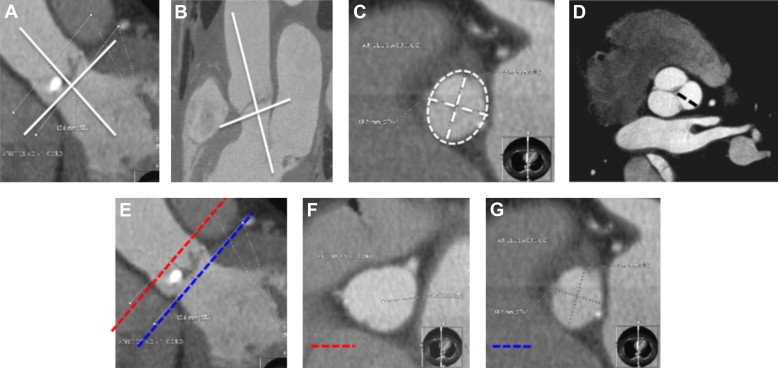
The MDCT examinations were performed with a Discovery HD750 scanner (GE Healthcare, Milwaukee, Wisconsin). All patients with a heart rate of ≥70 beats/min at rest received oral dose of ivabradine (10 mg/day) for 24 to 48 hours before MDCT to achieve a target heart rate of <70 beats/min. No patients were excluded because target heart rate was not reached. The MDCT parameters were slice configuration 64 × 0.625 mm, gantry rotation time 350 ms, tube voltage 120 kVp and effective tube current 650 mA. All patients received a double-injection protocol of an 80-ml bolus of contrast (Iomeron 400 mg/ml; Bracco, Milan, Italy) through an antecubital vein at an infusion rate of 5 ml/s, followed by 50 ml of saline solution. The scan was performed as follows: after contrast enhancement reached a predefined threshold of 200 HU in the right ventricle, patients were instructed to hold a deep breath and the scan was started when a predefined threshold of 200 HU was achieved in the left atrium using retrospective electrocardiographic (ECG) triggering. AoA by MDCT was defined as a virtual ring formed by joining the basal attachments of the aortic leaflets. For each AoA, maximum diameter, minimum diameter, and area were measured in systole in an orthogonal plane on the center line of the aorta ( Figure 2 ). Aortic leaflet calcifications were assessed on a short-axis view and graded visually (grade 1: no calcification, grade 2: mild calcifications, grade 3: moderate calcifications, and grade 4: heavy calcifications). Aortic leaflet length was defined as the distance from the basal attachment and the apex of the left coronary, right coronary, and noncoronary leaflets ( Figure 2 ). The coronary ostia height was defined as the distance between 2 orthogonal planes on the center line of the aorta centered at the level of AoA and the ostium of the left main coronary artery and right coronary artery ( Figure 2 ). For MDCT, the effective radiation dose was calculated as the dose-length product times a conversion coefficient for the chest (K = 0.017 mSv/mGy·cm). Each MDCT variable was measured by an expert reader blinded to the other imaging methods.
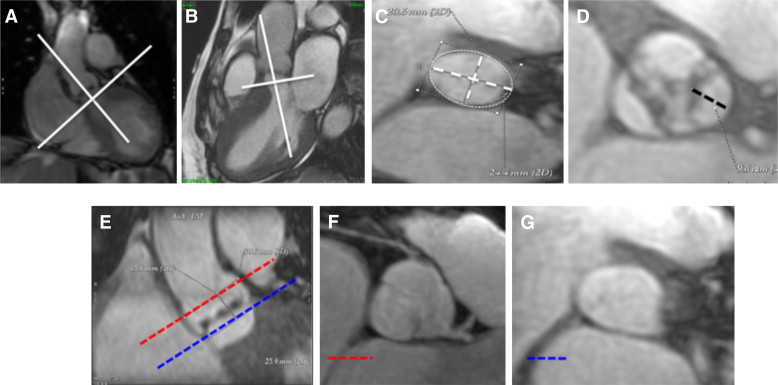
All patients were studied with a 1.5-T scanner (Discovery MR450; GE Healthcare, Milwaukee, Wisconsin) the same day of MDCT evaluation. Transaxial and coronal 1/2-Fourier acquisition single-shot turbo spin echo multislice pilot images were acquired during held expiration. Steady-state free precession cine acquisitions were then acquired, also during held expiration, without contrast agent injection because of the high contrast resolution between blood pool and cardiac chambers, using the following parameters: echo time 1.57 ms, 15 segments, repetition time 46 ms without view sharing, slice thickness 8 mm, field of view 350 mm × 263 mm, and pixel size 1.4 mm × 2.2 mm. To acquire cine planes, multiple short axis and 2-, 3-, and 4-chamber long axis of left ventricle were reached according to guidelines. Using the long-axis plane of the left ventricle, 2 long-axis views of the aortic root and ascending aorta were obtained ( Figure 3 ). Thus, serial short-axis cines orthogonal to the LVOT (3-mm thickness with 1.5-mm overlapping) were imaged including the entire aortic root ( Figure 3 ). AoA by CMR was defined as a virtual ring formed by joining the basal attachments of the aortic leaflets. For each AoA, maximum diameter, minimum diameter, and area were measured in systole in an orthogonal plane on the center line of the aorta ( Figure 3 ). Aortic leaflet length and coronary ostia height were measured as previously described for MDCT ( Figure 3 ). Each CMR variable was measured twice by 1 of the investigators (GP), while another blinded reader (DA) measured the same CMR variables once again to test intra- and interobserver variabilities. All CMR readers were blinded to the other imaging methods.
TAVIs were performed in a hybrid operating room with general anesthesia, endotracheal intubation, and fast-track anesthesia protocol by a combined team of cardiologists, cardiac surgeons, and anesthesiologists. The SAPIEN valve (Edwards Lifesciences Inc, Irvine, California) in 3 different sizes (23-, 26-, and 29-mm expanded diameter) was used in all patients. The final choice of the prosthesis size and approaching method was made according to guidelines.
Statistical analysis was performed with the SPSS, version 17.0 software (SPSS Inc., Chicago, Illinois). Continuous variables are expressed as mean ± SD and discrete variables as absolute numbers and percentages. The intra- and interobserver variabilities for the evaluation of CMR variables were defined by the coefficient of variation. Student t test was used to test differences of continuous variables between the baseline and post-TAVI parameters. The Spearman correlation and Bland-Altman analysis were used for comparing CMR to MDCT values. p Value <0.05 was considered statistically significant.
Results
Clinical characteristics of the 50 patients included in the study are summarized in Table 1 . All patients had severe aortic stenoses with normal left ventricular volumes and low-to-normal ejection fraction ( Table 1 ). The overall effective radiation dose of MDCT was 15.4 ± 5.3 mSv. The aortic root measurements with all imaging methods and the differences between CMR and other imaging methods are reported in Tables 2 and 3 , respectively. Both TTE and TEE showed an underestimation of the AoA area compared with CMR (p <0.01). In contrast, no differences were observed between CMR and MDCT except for aortic valve calcifications that were underestimated by CMR (p <0.05). The inter- and intraobserver variabilities of CMR measurements are listed in Table 4 . With regard to AoA maximum diameter, minimum diameter, and area, TTE ( Figure 4 ) and TEE ( Figure 5 ) showed only a moderate agreement versus CMR as shown by Pearson’s correlation and Bland-Altman analysis, respectively. In contrast, CMR showed an excellent agreement with MDCT regarding AoA root geometry ( Figure 6 ), heights of aortic leaflets ( Figure 7 ), and the distance between AoA and coronary artery ostia ( Figure 8 ). In 2 (4%) patients, a 23-mm prosthesis was implanted according to the AoA area measurements by MDCT , despite both TTE and TEE suggest to not perform TAVI for too small AoA size. In other 2 patients, TAVI was not performed because MDCT showed a too large AoA, whereas both TTE and TEE suggested a 29-mm valve. In the remaining patients, TTE and TEE suggested a smaller, equal, or larger prosthesis in 14 (28%), 31 (62%), and 1 patient (2%) and 8 (16%), 34 (68%), and 4 patients (8%) as compared to MDCT, respectively. CMR suggested a smaller, equal, or larger prosthesis in 1 (2%), 44 (88%), and 2 patients (4%) as compared to MDCT and agreed with MDCT to not perform TAVI for too large AoA size in 1 patient (2%). Moreover, in 1 patient (2%) a 29-mm prosthesis was implanted based on MDCT measurements without complications despite CMR suggested to not perform TAVI for too large AoA size. Finally, in 1 patient (2%), TAVI was not performed because MDCT showed a too large AoA, whereas CMR indicated a 29-mm valve. Therefore, the agreement to perform the procedure and the agreement for prosthesis size between TTE, TEE, and CMR versus MDCT were 92% and 62%, 92% versus 68%, and 96% and 88%, respectively.
| Variable | Baseline | After Implantation (1 mo) |
|---|---|---|
| Clinical characteristics | ||
| Number of patients, n | 50 | — |
| Gender (men/women), n | 27/23 | — |
| Age (yrs) | 79.6 ± 7.5 | — |
| Body mass index (kg/m 2 ) | 25.9 ± 5.6 | — |
| BSA (m 2 ) | 1.8 ± 0.2 | — |
| Logistic EuroSCORE | 22.4 ± 8 | — |
| TTE characteristics | ||
| Left ventricular end-diastolic volume/BSA (ml/m 2 ) | 58.4 ± 25.1 | 51.6 ± 21.7 |
| Left ventricular end-systolic volume/BSA (ml/m 2 ) | 26.3 ± 19.3 | 23.3 ± 15.1 |
| Left ventricular ejection fraction (%) | 57.8 ± 11.8 | 57.4 ± 12.2 |
| Mitral regurgitation (grade 0–4) | 1 ± 0.8 | 1.0 ± 0.7 |
| Peak aortic gradient (mm Hg) | 78 ± 18.5 ∗ | 19.3 ± 6.9 |
| Mean aortic gradient (mm Hg) | 47.8 ± 12.2 ∗ | 10.8 ± 5.0 |
| Aortic valve area/BSA (cm 2 /m 2 ) | 0.4 ± 0.1 ∗ | 1.4 ± 0.4 |
| Aortic regurgitation (grade 0–4) | 1.2 ± 0.9 ∗ | 0.5 ± 0.9 |
| Pulmonary pressure (mm Hg) | 39.3 ± 10.4 | 36.8 ± 8.6 |
| CMR characteristics | ||
| Left ventricular end-diastolic volume/BSA (ml/m 2 ) | 85.7 ± 29.3 | — |
| Left ventricular end-systolic volume/BSA (ml/m 2 ) | 46.1 ± 41.6 | — |
| Left ventricular ejection fraction (%) | 55.3 ± 13.9 | — |
| Right ventricular end-diastolic volume/BSA (ml/m 2 ) | 65.5 ± 15.9 | — |
| Right ventricular end-systolic volume/BSA (ml/m 2 ) | 24.6 ± 10.7 | — |
| Right ventricular ejection fraction (%) | 63 ± 10.3 | — |
| Mitral regurgitation (ml) | 3.4 ± 6.9 | — |
| Aortic valve area/BSA (cm 2 /m 2 ) | 0.4 ± 0.1 | — |
| Aortic regurgitation (ml) | 4.2 ± 8.0 | — |
| Variable | CMR | TTE | TEE | MDCT |
|---|---|---|---|---|
| AoA maximum diameter (mm) | 26.4 ± 2.8 | — | — | 26.5 ± 2.8 |
| AoA minimum diameter (mm) | 20.6 ± 2.3 | 21.9 ± 2.4 | 22.6 ± 2.6 | 20.2 ± 2.2 |
| AoA area (mm 2 ) | 449.8 ± 86.2 | 379.6 ± 82.2 | 404.2 ± 89.8 | 444.9 ± 84.6 |
| Aortic valve calcifications (grade 1–4) | 2.9 ± 0.8 | — | — | 3.4 ± 0.7 |
| Length of the left coronary leaflet (mm) | 13.9 ± 2.2 | — | — | 14 ± 2.3 |
| Length of the right coronary leaflet (mm) | 13.3 ± 2.1 | — | — | 13.3 ± 2.3 |
| Length of the noncoronary leaflet (mm) | 13.4 ± 1.8 | — | — | 13.4 ± 2.0 |
| AoA-to-left coronary ostium distance (mm) | 16.1 ± 2.8 | — | — | 16.2 ± 3.1 |
| AoA-to-right coronary ostium distance (mm) | 16.1 ± 4.4 | — | — | 16.0 ± 4.3 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


