Smoking is associated with high incidence of cardiovascular events including acute coronary syndrome. We sought to characterize coronary plaques in patients with ongoing smoking using optical coherence tomography (OCT) compared with former smokers and nonsmokers. We identified 465 coronary plaques from 182 subjects who underwent OCT imaging for all 3 coronary arteries. Subjects were divided into 3 groups: current smokers (n = 41), former smokers (n = 67), and nonsmokers (n = 74). OCT analysis included the presence of lipid-rich plaque, thin-cap fibroatheroma (TCFA), calcification, maximum lipid arc, lipid core length, lipid index, and fibrous cap thickness. Lipid index was defined by mean lipid arc multiplied by lipid core length. Compared with former smokers and nonsmokers, the incidence of lipid plaques and TCFA was significantly higher in current smokers (lipid plaques: 68.0% vs 45.9% and 52.6%, p = 0.002; TCFA: 18.4% vs 7.6% and 9.9%, p = 0.018). There was a trend for higher plaque disruption in current smokers. Former smokers were more likely to have calcified plaques than current and nonsmokers (52.9% vs 32.0% and 38.0%, p = 0.001). In a multivariate analysis, current smoking, low-density lipoprotein, and presentation with acute coronary syndrome were independently associated with the presence of TCFAs. In conclusion, current smokers are more likely to have lipid plaques and OCT-defined vulnerable plaques (TCFAs). Former smokers have increased number of calcified plaques. These results may explain the increased risk of acute cardiac events among smokers.
Smoking is a significant contributor to cardiovascular disease and by recent estimates results in >1 million cardiovascular deaths annually worldwide. More specifically, smoking is a major risk factor for acute coronary syndrome (ACS) and sudden cardiac death. Smoking is believed to increase the burden of cardiovascular disease by inducing endothelial dysfunction, increasing the burden of coronary atherosclerosis and increasing the risk of thrombosis. Optical coherence tomography (OCT) is an intravascular imaging technique that allows visualization of coronary arteries with high resolution. OCT can provide detailed in vivo information on atherosclerotic plaques inside vessels, including tissue characteristics and fibrous cap thickness. In this study, using a data set from 182 patients who underwent OCT imaging of all 3 epicardial vessels, we sought to correlate smoking history (current, former, and never) with coronary plaque characteristics as identified by OCT.
Methods
The Massachusetts General Hospital OCT registry is a multicenter registry of patients who underwent OCT of the coronary arteries and includes 20 sites across 6 countries. From a total of 1,406 patients who were enrolled in the registry between August 2010 and May 2012, we identified 198 patients who underwent OCT imaging of all 3 major epicardial coronary arteries. From this cohort, we selected the patients who had at least 1 nonculprit or nontarget coronary plaques with area stenosis >50% as measured by OCT using the Working Group for Intravascular Optical Coherence Tomography Standardization and Validation definition for stenosis. Stenoses at sites of previous stenting and those that required balloon angioplasty before OCT imaging were excluded. Patients with incomplete clinical histories or laboratory data were also excluded. The final data set included 182 subjects with 465 nonculprit plaques. Subjects were divided into 3 groups: current active smokers (103 plaques in 41 subjects), former smokers who had quit at least 3 months before (170 plaques in 67 subjects), and those who had never smoked (192 plaques in 74 subjects). Patients with ACS included those presenting with ST-elevation myocardial infarction (STEMI), non-STEMI, and unstable angina. STEMI was defined as continuous chest pain that lasted >30 minutes, arrival at the hospital within 12 hours from the onset of chest pain, ST-segment elevation >0.1 mV in ≥2 contiguous leads, or new left bundle-branch block on the 12-lead electrocardiogram (ECG) and elevated cardiac markers (creatine kinase-MB or troponin T/I). Non-STEMI was defined as ischemic symptoms in the absence of ST elevation on ECG with elevated cardiac markers. Unstable angina was defined as angina at rest, accelerated angina, or new-onset angina.
OCT images were obtained using either the time-domain (M2/M3 Cardiology Imaging System, LightLab Imaging, Inc., Westford, MA) or frequency-domain OCT system (C7-XR OCT Intravascular Imaging System, St Jude Medical, St. Paul, MN) as previously described. All images were digitally stored, de-identified, and submitted to the Massachusetts General Hospital (Boston, MA) for analysis.
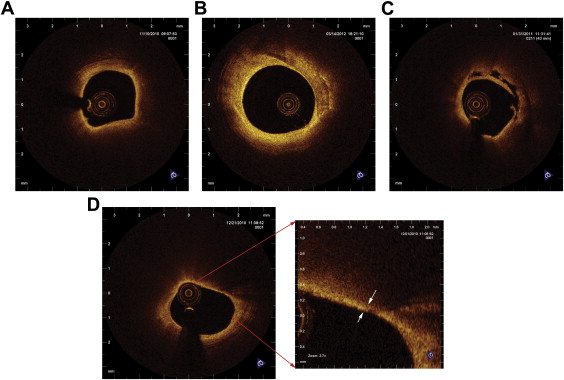
Only nonculprit and nontarget plaques were included in the analysis. Each plaque was classified as lipid-rich or fibrous plaque and was separated at least 5 mm from the edge of another plaque or from an implanted stent edge as seen on the longitudinal OCT pullback. Lipid was identified as diffusely bordered signal-poor region with signal attenuation by the overlying signal-rich layer. Lipid-rich plaque was defined as a plaque with lipid involving >90° of the vessel wall circumference (lipid arc) ( Figure 1 ). In addition, the presence or absence of thin-cap fibroatheroma (TCFA), macrophage accumulation, cholesterol crystal, plaque disruption, and microvessels were noted. The thinnest fibrous cap thickness of a lipid-rich plaque was measured as the mean of the thinnest 3 points identified by visual estimation. TCFA was defined as a lipid-rich plaque with a maximum lipid arc >90° and fibrous cap thickness ≤65 μm ( Figure 1 ). Macrophage accumulations on the OCT images were identified by increased signal intensity within the plaque, accompanied by heterogeneous backward shadows. Cholesterol crystals were characterized as thin linear regions of high intensity existing beside a lipid core. Microvessels were defined as small vesicular or tubular structures with diameters 50 to 300 μm and differentiated from any other vessel branch. Calcification was also recorded when an area with low backscatter and a sharp border was identified inside a plaque ( Figure 1 ). Plaque disruption was defined as a discontinuity of the fibrous cap with communication between the vessel lumen and the cavity ( Figure 1 ). OCT images were analyzed by 2 investigators who were blinded to the subject’s information.
Coronary angiogram was analyzed by off-line quantitative coronary angiography (CAAS 5.10.1; Pie Medical Imaging BV, Maastricht, The Netherlands). Reference diameter, minimum lumen diameter, diameter stenosis, and lesion length were measured.
For the description of subject demographic and clinical characteristics, categorical data were presented as counts or proportions and were compared using chi-square test, and continuous measurements were presented as mean ± SD and compared using ANOVA followed by post hoc tests with Bonferroni correction for multiple comparisons. Univariate and multivariate logistic regression models were applied to determine independent predictors for the presence of TCFA. Multivariate logistic regression model included age of subject, gender, presentation (ACS vs non-ACS), hypertension, hyperlipidemia, diabetes mellitus, smoking history, statin use, creatinine, and low-density lipoprotein (LDL) level. For comparisons between groups, the plaque-based analysis was carried out by means of the generalized estimating equation approach to take into account within-subject correlation because of multiple plaques analyzed within a single subject. All statistical analyses were performed with SPSS 17.0 (SPSS Inc, Chicago, IL). A p value <0.05 was considered statistically significant.
Results
Patient characteristics are summarized in Table 1 . Compared with former smokers, current smokers were significantly younger and more frequently presented with ACS. Current smokers were significantly less likely to be taking a statin than either former or never smokers. Plaque location and angiographic data are listed in Table 2 . There was no significant difference in plaque location among the 3 groups. Current smokers had larger minimum lumen diameters and reference diameters than never smokers without a significant difference in diameter stenosis.
| Variable | Current Smoker (CS) (n = 41) | Former Smoker (FS) (n = 67) | Never Smoker (NS) (n = 74) | Pearson Chi-Square or ANOVA | p Value CS vs. NS | p Value CS vs. FS | p Value FS vs. NS |
|---|---|---|---|---|---|---|---|
| Age (years) | 56.0 ± 11.7 | 61.6 ± 11.3 | 61.7 ± 9.9 | 0.014 | 0.024 | 0.025 | 1.0 |
| Men | 38 (93%) | 61 (91%) | 40 (54%) | <0.001 | <0.001 | 0.765 | <0.001 |
| Hypertension | 22 (54%) | 52 (77%) | 51 (69%) | 0.038 | 0.104 | 0.011 | 0.267 |
| Hyperlipidemia | 33 (80%) | 50 (75%) | 62 (84%) | 0.490 | |||
| Acute coronary syndrome | 26 (63%) | 18 (27%) | 33 (45%) | 0.001 | 0.053 | <0.001 | 0.029 |
| Body mass index (kg/m 2 ) | 24.7 ± 2.1 | 24.8 ± 3.2 | 24.3 ± 2.4 | 0.540 | |||
| Diabetes mellitus | 14 (34%) | 25 (37%) | 38 (51%) | 0.117 | |||
| Statin | 16 (39%) | 47 (70%) | 55 (74%) | <0.001 | <0.001 | 0.001 | 0.580 |
| Aspirin | 40 (98%) | 66 (99%) | 71 (96%) | 0.861 | |||
| ACE-I/ARB | 18 (44%) | 35 (52%) | 29 (39%) | 0.294 | |||
| Beta blocker | 17 (41%) | 31 (46%) | 39 (53%) | 0.488 | |||
| LDL-cholesterol (mg/dl) | 92.3 ± 30.1 | 91.5 ± 37.1 | 89.8 ± 33.5 | 0.924 | |||
| HDL-cholesterol (mg/dl) | 40.7 ± 8.0 | 43.5 ± 11.2 | 44.7 ± 13.1 | 0.216 | |||
| Creatinine (mg/dl) | 1.22 ± 1.08 | 1.35 ± 1.76 | 1.14 ± 1.24 | 0.696 |
| Variable | Current Smoker (CS) (n = 103) | Former Smoker (FS) (n = 170) | Never Smoker (NS) (n = 192) | p Value | p Value CS vs. NS | p Value CS vs. FS | p Value FS vs. NS |
|---|---|---|---|---|---|---|---|
| Coronary artery | |||||||
| Right | 37 (36%) | 68 (40%) | 74 (39%) | 0.970 | |||
| Left anterior descending | 38 (37%) | 61 (36%) | 69 (36%) | ||||
| Left circumflex | 28 (27%) | 41 (24%) | 49 (26%) | ||||
| Minimum lumen diameter (mm) | 1.96 ± 0.054 | 1.87 ± 0.62 | 1.71 ± 0.533 | 0.005 | 0.011 | 1.0 | 0.052 |
| Reference diameter (mm) | 2.99 ± 0.61 | 3.06 ± 0.65 | 2.76 ± 0.60 | <0.001 | 0.027 | 1.0 | <0.001 |
| Lesion length (mm) | 9.99 ± 4.49 | 10.03 ± 4.15 | 8.97 ± 4.12 | 0.068 | |||
| Diameter stenosis (%) | 34.6 ± 13.5 | 38.1 ± 16.0 | 37.4 ± 16.0 | 0.306 |
Patient-level plaque analysis is listed in Table 3 . The number of plaques per patient identified by OCT was similar in all 3 groups. Current smokers were more likely to have at least 1 lipid-rich plaque and TCFAs. Plaque-level analysis is shown in Figure 2 and listed in Supplementary Table 1 . Current smokers had significantly more lipid-rich plaques compared with former smokers and never smokers. TCFAs were also significantly more prevalent in current smokers, and there was a trend toward increased number of plaque disruptions in current smokers, but this did not reach statistical significance (p = 0.100). In contrast, calcifications were most frequently seen in the plaques of former smokers.
| Variable | Current Smoker (CS) (n = 41) | Former Smoker (FS) (n = 67) | Never Smoker (NS) (n = 74) | p Value |
|---|---|---|---|---|
| Plaques per patient | 2.93 ± 1.63 | 2.84 ± 1.43 | 2.93 ± 1.78 | 0.931 |
| Lipid rich plaque | 35 (85%) | 41 (61%) | 53 (72%) | 0.027 |
| Thin-cap fibroatheroma | 15 (37%) | 11 (16%) | 14 (19%) | 0.035 |
| Disruption | 9 (22%) | 9 (13%) | 14 (19%) | 0.490 |
| Calcium | 23 (56%) | 43 (64%) | 48 (65%) | 0.614 |
| Macrophage | 20 (49%) | 35 (52%) | 35 (47%) | 0.838 |
| Microchannels | 23 (56%) | 43 (64%) | 43 (58%) | 0.652 |
| Cholesterol crystal | 15 (37%) | 32 (47%) | 33 (45%) | 0.519 |
| Thrombus | 8 (19%) | 6 (9%) | 10 (14%) | 0.288 |
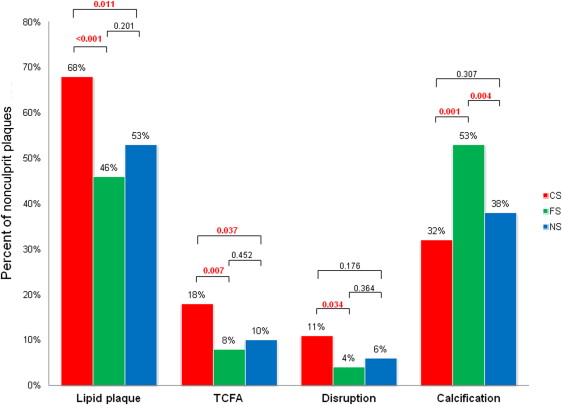
Univariate and multivariate logistic regression models are listed in Table 4 . Multivariate modeling indicated that presentation with ACS, current smoking, and increasing LDL cholesterol was independently associated with the presence of TCFAs. The presence of each of these risk factors was associated with increased prevalence of TCFAs ( Figure 3 ), which is consistent with the results of the multivariate model. To further limit possible confounding, we performed a multivariate analysis limited to patients presenting with ACS (current smokers: 62 plaques in 26 patients, former smokers: 50 plaques in 18 patients, and never smokers: 96 plaques in 33 patients). Current smoking, diabetes mellitus, and increasing levels of LDL were independently associated with the presence of TCFAs in ACS patients ( Supplementary Table 2 ).
| Variable | Univariate Logistic Regression Model | Multivariate Logistic Regression Model | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Regression Coefficient | SE | Odds Ratio | 95% Confidence Limits | p-Value | Regression Coefficient | SE | Odds Ratio | 95% Confidence Limits | p-Value | |||
| Lower | Upper | Lower | Upper | |||||||||
| Age (year) | 0.01 | 0.02 | 1.01 | 0.96 | 1.05 | 0.830 | −0.01 | 0.02 | 0.99 | 0.95 | 1.03 | 0.651 |
| Men | 0.43 | 0.50 | 1.54 | 0.57 | 4.10 | 0.392 | 0.81 | 0.56 | 2.25 | 0.74 | 6.80 | 0.151 |
| Acute coronary syndrome | 0.82 | 0.36 | 2.28 | 1.13 | 4.60 | 0.022 | 0.93 | 0.37 | 2.53 | 1.21 | 5.27 | 0.023 |
| Hypertension | −0.37 | 0.37 | 0.69 | 0.33 | 1.44 | 0.329 | −0.21 | 0.39 | 0.81 | 0.38 | 1.75 | 0.843 |
| Hyperlipidemia | 0.05 | 0.45 | 1.05 | 0.44 | 2.52 | 0.919 | 0.04 | 0.44 | 1.04 | 0.44 | 2.44 | 0.886 |
| Diabetes mellitus | 0.21 | 0.35 | 1.24 | 0.63 | 2.45 | 0.539 | 0.53 | 0.37 | 1.70 | 0.83 | 3.48 | 0.301 |
| Current Smoker ∗ | 0.85 | 0.37 | 2.33 | 1.12 | 4.86 | 0.024 | 0.89 | 0.40 | 2.44 | 1.11 | 5.40 | 0.033 |
| Former smoker ∗ | −0.28 | 0.40 | 0.76 | 0.35 | 1.63 | 0.475 | −0.39 | 0.46 | 0.68 | 0.28 | 1.66 | 0.394 |
| Statin | −0.92 | 0.34 | 0.40 | 0.21 | 0.78 | 0.007 | −0.07 | 0.43 | 0.94 | 0.40 | 2.17 | 0.879 |
| Creatinine (mg/dl) | −0.07 | 0.15 | 0.93 | 0.70 | 1.24 | 0.618 | −0.12 | 0.17 | 0.89 | 0.64 | 1.23 | 0.525 |
| LDL-cholesterol (mg/dl) | 0.01 | 0.00 | 1.01 | 1.00 | 1.02 | 0.002 | 0.01 | 0.01 | 1.01 | 1.00 | 1.02 | 0.029 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


