Adverse outcomes increase in frequency as patients after Fontan operation approach adulthood. Cardiac magnetic resonance (CMR) imaging–derived parameters have been shown to predict death/transplant; however, limited data are available on the usefulness of echocardiography in risk stratification. We conducted a retrospective, single-center review of records of patients after Fontan operation with an echocardiogram and CMR within 1 year of each other. The primary end point was time to all-cause mortality or listing for transplant. Of the 127 eligible patients, there were 12 end points (9%; 10 deaths and 2 listing for transplant). Median age was 16.8 years (interquartile range 12 to 23.1) with a median follow-up of 3.8 years (interquartile range 2.6 to 5.7). Among clinical parameters, protein-losing enteropathy had the strongest association with the outcome. Among echocardiographic variables, global circumferential strain showed the strongest association (hazard ratio 1.3 per unit change, 95% confidence interval 1.1 to 1.5, p value 0.001, C-index 0.81), whereas among CMR variables indexed ventricular end-diastolic volume showed the strongest association with the outcome (hazard ratio 1.04 per 10 ml/BSA 1.3 increase in volume, 95% confidence interval 1.02 to 1.06, p value 0.001, C-index 0.82). Cox proportional hazards analysis revealed echocardiography and CMR models to each individually have a higher predictive ability than the clinical model; however, in direct comparison, neither technique was superior. In conclusion, both echocardiography-derived circumferential strain and CMR-derived ventricular end-diastolic volume index are associated with transplant-free survival in patients after Fontan operation. Echocardiography and CMR parameters have higher discriminative ability than clinical variables. Although neither imaging technique is superior in this cohort, both introduce important factors for risk stratification.
The Fontan circulation is the final physiological state achieved after a series of palliative procedures in patients with functional single ventricles. Perioperative morbidity and mortality have significantly decreased in children after the Fontan surgery; however, adverse outcomes are increasingly frequent as they approach adulthood. Several clinical risk factors have been associated with poor survival in this population. Protein-losing enteropathy (PLE) occurs in ∼3% to 15% of patients after Fontan operation, with high mortality. Patients with diminished exercise capacity, portal hypertension, systemic oxygen desaturation, and with functional single right ventricles have also been identified to have a higher risk of death. Despite routine interval imaging follow-up with echocardiography and/or cardiac magnetic resonance (CMR) examinations, there is limited knowledge about associations between imaging parameters and adverse outcomes, such as death or need for transplantation. We recently demonstrated that CMR-derived indexed ventricular end-diastolic volume (EDV i ) independently predicted death and transplantation in patients late after the Fontan operation and added incremental value over clinical variables alone. Myocardial strain measured by echocardiography has been studied in patients after Fontan operation, but there are no data on its utility in predicting adverse outcomes. The goal of this study was to compare the echocardiographic and CMR parameters associated with death or transplantation in patients after the Fontan operation.
Methods
We conducted a retrospective, single-center study of patients after Fontan operation who had both an echocardiogram and a CMR performed at Boston Children’s Hospital within 1 year of each other from January 1, 2005, to June 30, 2013. A minimum of 1 year of clinical follow-up after the latter of the 2 studies, or occurrence of the primary end point defined subsequently, was required for inclusion. Patients were excluded if there was a catheter or surgical intervention between echocardiogram and CMR or if images were inadequate for ventricular size and function measurements or speckle tracking (in at least 1 echocardiographic view). If multiple sets of echocardiograms and CMR examinations met inclusion criteria, the oldest available study was used for analysis. The Boston Children’s Hospital Committee on Clinical Investigation approved this study and waived the requirement for informed consent.
The primary end point was a composite of all-cause mortality or listing for heart transplantation. Dates of listing for cardiac transplantation, transplantation, or death were confirmed against the New England Organ Bank and the Social Security Death Index databases. For survival analyses, follow-up was measured from the date of echocardiogram to either the end point or the last known follow-up date with documented transplant-free survival.
Patient medical records were reviewed for the following clinical variables: date of birth, gender, age and body surface area (BSA) at testing, cardiac anatomy, and type of Fontan surgery. Ventricular morphology was classified as left ventricular, right ventricular, or mixed (eg, unbalanced atrioventricular canal), according to previously published criteria. Ventricular type was classified as mixed if both ventricles had a CMR-derived EDV z-score greater than −4. Recorded co-morbidities included sustained ventricular tachycardia (VT), significant atrial arrhythmia (documented atrial flutter, fibrillation, or other supraventricular tachycardia), successful resuscitation after cardiac arrest, history of cerebrovascular accident, seizures, and PLE. Diagnosis of PLE was made based on review of notes written by patients’ primary attending cardiologists.
All echocardiograms were obtained using Phillips IE33 machines (Philips Healthcare, Best, The Netherlands) using S8/S5/X5 transthoracic probes. Echocardiograms were reviewed by a single observer (SJG) for the following: aortic regurgitation grade, atrioventricular valve regurgitation grade, qualitative assessment of systolic function, and presence or absence of a Fontan fenestration. EDV and end-systolic (ESV) volumes by echocardiography were estimated using the modified Simpson’s biplane method as previously described ( Figure 1 ). Regardless of the dominant ventricular morphology type, when 2 ventricles contributed to the systemic circulation, ventricular volumes were added to allow for calculation of total functional EDV, ESV, and ejection fraction (EF). Ventricular volumes were indexed to BSA 1.3 as described previously. Myocardial deformation was evaluated by 2-dimensional speckled tracking using commercially available software (TomTec Imaging Systems, Unterschleissheim, Germany; Figure 2 ). The endocardial border of the dominant ventricle was manually traced and the software automatically performed tracking. If tracking was judged to be suboptimal by visual inspection, the endocardial border was retraced until either satisfactory tracking was accomplished or 5 minutes had elapsed, in which case the view was excluded from analysis. Measured deformation parameters included peak global systolic longitudinal strain (GLS, %), peak GLS rate (1/s), peak global systolic circumferential strain (GCS; %), and peak GCS rate (1/s). As both longitudinal and circumferential strain measurement represents decrease in dimension, mathematically higher strain is represented by a more negative number and lower strain is represented by a less negative number.
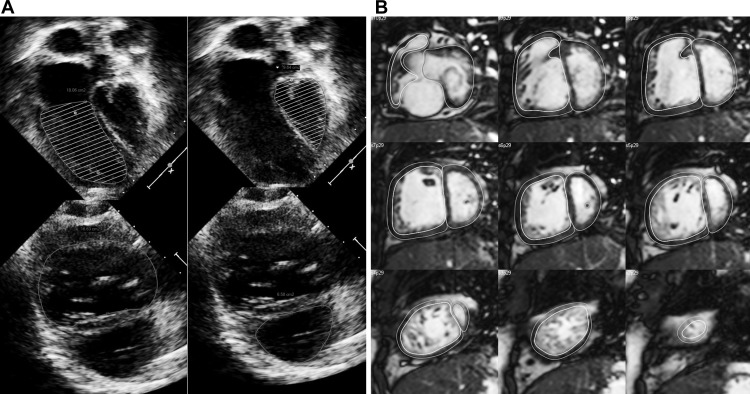
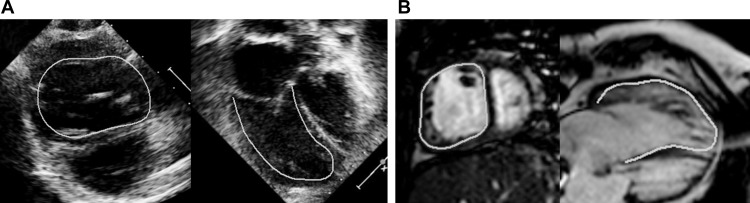
All CMR studies were performed with a 1.5 T scanner (Philips Healthcare). The details of the CMR protocols used in our laboratory for assessment of patients after the Fontan operation have been published. Briefly, ventricular mass, volumes, and EF were measured by manual tracing of endocardial and epicardial borders on each short-axis steady-state free precession cine slice at end-diastole (maximal area) and end-systole (minimal area; Figure 1 ). Analysis was performed using commercially available software (QMass; Medis Medical Imaging Systems, Leiden, The Netherlands). EDV, ESV, stroke volume, EF, mass, and mass-to-volume ratio were calculated as previously described. Similar to echocardiogram variables, ventricular volumes and mass were added when 2 contributing ventricles were present and were indexed to BSA 1.3 . Published normative data from Alfakih et al were used for ventricular z-score calculations. Feature tracking analysis was performed on the CMR images in the horizontal long-axis and short-axis planes, which are comparable with the echocardiographic apical and parasternal short-axis views ( Figure 2 ). The analysis was performed using the same software used for speckle-tracking echocardiography as noted earlier. The methodology for strain analysis on CMR images was the same as for echocardiography, and the same strain variables were recorded.
Continuous data were summarized as medians with interquartile range (IQR) unless otherwise listed. The Mann-Whitney U test was used for comparison between groups. Categorical variables were presented as percentages and compared between groups using Fisher’s exact tests. Variables with p value <0.1 on univariable analysis were considered for inclusion in the Cox proportional hazards survival models. Collinearity between variables was explored using scatter plots and Spearman and Pearson correlation tests. When collinearity was present, the candidate predictor variable with the highest discrimination by Harrell’s C-index was chosen for entry into the model. Separate Cox proportional hazards survival models were constructed for clinical, echocardiographic, and CMR predictor variables. Concordance indices, defined the proportion of patient-outcome pairs in which the outcome is concordant with the prediction produced by the model, were calculated and compared using methods described by Newson et al. A concordance index of 1.0 indicated perfect prediction and a value of 0.5 indicated no predictive discrimination. Receiver operator characteristics curves and tables were used to dichotomize continuous variables. Kaplan-Meier survival plots were used to visually depict time-dependent freedom from the composite outcome, and the log-rank test was used to compare groups. Data analysis was performed using SPSS, version 21.0 (SPSS Inc., Chicago, Illinois), Stata, version 13.1 (StataCorp LP, College Station, Texas), and R, version 3.1.2 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 127 patients met inclusion criteria. Median age at Fontan was 3.1 years (IQR 2.3 to 4.8 years) and median age at study echocardiogram was 16.8 years (IQR 12 to 23.1 years). The primary end point occurred in 12 patients (10 deaths and 2 transplant listings) during a median follow-up of 3.8 years (IQR 2.6 to 5.7 years, range 1.4 to 8.6 years). The cumulative freedom from the primary end point was 97% at 1 year and 91% at 5 years. Baseline characteristics and findings of univariable analysis of demographic and clinical predictor variables are presented in Table 1 .
| Clinical characteristic | All patients (n = 127) | Transplant free survival (n = 115) | Death or transplant (n = 12) | p value |
|---|---|---|---|---|
| Male | 83 (65) | 73 (63) | 10 (83) | 0.22 |
| Age at Fontan (years) | 3.1 [2.3, 4.8] | 3.1 [2.3, 4.8] | 3.4 [2, 4.9] | 0.89 |
| Age at echo (years) | 16.8 [12.0, 23.1] | 16.8 [12.1, 23.1] | 17.9 [8.2, 24.4] | 0.93 |
| Body surface area (m 2 ) | 1.6 [1.2, 1.9] | 1.6 [1.3, 1.9] | 1.7 [1, 1.9] | 0.88 |
| Ventricular morphology | ||||
| Left ventricle | 56 (44%) | 54 (47%) | 2 (17%) | |
| Right ventricle | 46 (36%) | 39 (34%) | 7 (58%) | 0.12 |
| Mixed | 25 (20%) | 22 (19%) | 3 (25%) | |
| Fontan Type | ||||
| Lateral tunnel | 109 (86%) | 100 (88%) | 9 (75%) | |
| Extracardiac | 6 (5%) | 6 (5%) | 0 (0%) | |
| Right atrium pulmonary artery | 10 (8%) | 9 (8%) | 1 (8%) | 0.02 |
| Right atrium right ventricle | 2 (2%) | 0 (0%) | 2 (17%) | |
| Patent fenestration | 31 (24%) | 26 (23%) | 5 (42%) | 0.33 |
| Sustained ventricular tachycardia or arrest | 19 (15%) | 14 (12%) | 5 (42%) | 0.02 |
| Significant atrial arrhythmia | 40 (31%) | 36 (31%) | 4 (33%) | 1.00 |
| Protein losing enteropathy | 7 (6%) | 4 (4%) | 3 (25%) | 0.02 |
| Seizure | 12 (9%) | 10 (9%) | 2 (17%) | 0.32 |
| Cerebro-vascular accident | 23 (18%) | 19 (17%) | 4 (33%) | 0.23 |
On univariable analysis, several echocardiographic and CMR parameters were associated with the primary end point ( Table 2 ). Of the echocardiographic variables, decreased systolic function, lower GLS and GLS rate, lower GCS and GCS rate, and increased indexed ventricular volumes (EDV i and ESV i ) were associated with the end point. Similar univariable associations regarding ventricular volumes, systolic function, and strain were noted by CMR, with the addition of increased ventricular mass being associated with the primary end point.
| Transplant free survival | Death or transplant | p value | |||
|---|---|---|---|---|---|
| n | n | ||||
| Echocardiographic variables | |||||
| ≥ Moderate aortic regurgitation | 115 | 1 (1) | 12 | 0 (0) | 1.00 |
| ≥ Moderate atrio-ventricular valve regurgitation | 115 | 3 (3) | 12 | 1 (8) | 0.33 |
| ≥ Moderate systolic dysfunction | 115 | 5 (4) | 12 | 5 (42) | 0.001 |
| Global longitudinal strain (%) | 109 | -15.6 [-17.6, -11.8] | 12 | -11.4 [-13.6, -6.3] | 0.001 |
| Global longitudinal strain rate (s -1 ) | 109 | -0.8 [-1, -0.7] | 12 | -0.7 [-0.8, -0.4] | 0.02 |
| Global circumferential strain (%) | 100 | -17.9 [-20.1, -14.3] | 10 | -12.0 [-17.6, -7.2] | 0.004 |
| Global circumferential strain rate (s -1 ) | 100 | -1 [-1.2, -0.9] | 10 | -0.6 [-0.9, -0.5] | 0.001 |
| Indexed end-diastolic volume (ml/body surface area 1.3 ) | 99 | 70.5 [53.3, 90.7] | 10 | 125.8 [76.2, 162.4] | 0.003 |
| Indexed end-systolic volume (ml/body surface area 1.3 ) | 99 | 31.1 [23.0, 46.8] | 10 | 76.0 [45.3, 123.1] | 0.001 |
| Ejection fraction (%) | 99 | 52.5 [51.4, 56.6] | 10 | 40.5 [24.1, 45.9] | 0.002 |
| Cardiac magnetic resonance imaging variables | |||||
| Global longitudinal strain (%) | 111 | -15.2 [-17.2, -12.7] | 12 | -11.7 [-15.3, -6.0] | 0.01 |
| Global longitudinal strain rate (s -1 ) | 111 | -1 [-1.1, -0.8] | 12 | -0.7 [-1.2, -0.4] | 0.04 |
| Global circumferential strain (%) | 113 | -19.7 [-22.5, -16.5] | 12 | -12.4 [-18.5, -4.3] | 0.001 |
| Global circumferential strain rate (s -1 ) | 113 | -1.1 [-1.4, -0.9] | 12 | -0.8 [-1.3, -0.3] | 0.02 |
| Indexed end-diastolic volume (ml/body surface area 1.3 ) | 115 | 97.3 [76.1, 116.3] | 12 | 153.0 [101.5, 235.0] | 0.001 |
| Indexed end-systolic volume (ml/body surface area 1.3 ) | 115 | 44.3 [33.0, 61.1] | 12 | 81.4 [38.8, 183.6] | 0.004 |
| Ejection fraction (%) | 115 | 53.8 [46.5, 58.8] | 12 | 46.7 [23.3, 54.6] | 0.04 |
| Indexed ventricular mass (g/body surface area 1.3 ) | 114 | 50.0 [41.4, 61.1] | 12 | 72.8 [46.5, 94.8] | 0.007 |
| Mass-to-volume ratio (g/ml) | 114 | 0.5 [0.4, 0.6] | 12 | 0.5 [0.4, 0.6] | 0.31 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


