Comparative studies evaluating traditional versus newer antianginal (AA) medications in chronic stable angina pectoris (CSA) on cardiovascular (CV) outcomes and utilization are limited, particularly in patients with diabetes mellitus (DM). Claims data (2008 to 2012) were analyzed using a commercial database. Patients with CSA receiving a β blocker (BB), calcium channel blocker (CCB), long-acting nitrate (LAN), or ranolazine were identified and followed for 12 months after a change in AA therapy. Patients on traditional AA medications were required to have concurrent sublingual nitroglycerin. Therapy change was defined as adding or switching to another traditional AA medication or ranolazine to identify patients whose angina was inadequately controlled with previous therapy. Four groups were identified (BB, CCB, LAN, or ranolazine users) and matched on relevant characteristics. A DM subset was identified. Logistic regression compared revascularization at 30, 60, 90, 180, and 360 days. Negative binomial regression compared all-cause, CV-, and DM-related (in the DM cohort) health care utilization. A total of 8,008 patients were identified with 2,002 patients in each matched group. Majority were men (mean age 66 years). A subset of 3,724 patients with DM (BB, n = 933; CCB, n = 940; LAN, n = 937; and ranolazine, n = 914) resulted from this cohort. Compared to ranolazine in the overall cohort, traditional AA medication exhibited greater odds for revascularization and higher rates in all-cause outpatient, emergency room visits, inpatient length of stay, and CV-related emergency room visits. In the DM cohort, ranolazine demonstrated similar benefits over traditional AA medication. In conclusion, ranolazine use in patients with inadequately controlled chronic angina is associated with less revascularization and all-cause and CV-related health care utilization compared to traditional AA medication.
We hypothesize that ranolazine, compared to traditional antianginals (AA) may significantly reduce health care resource utilization, particularly in those with co-morbid diabetes mellitus (DM). Currently, limited data exist regarding the effect that various treatment strategies have on health care resource utilization in patients with chronic stable angina pectoris (CSA), particularly within a real-world setting. Given the paucity of data, as well as the considerable burden of CSA in the United States, comparative effectiveness data are needed to determine which treatment strategies can reduce health care resource utilization and improve cardiovascular (CV)–related outcomes. To address this need, we performed a retrospective, quasi-experimental study in patients with CSA to compare differences between ranolazine and traditional AA therapies (e.g., β blockers [BBs], calcium channel blockers [CCBs], and long-acting nitrates [LANs]) on health care resource utilization consisting of outpatient visits, emergency room visits, inpatient admissions, and inpatient length of stay, and need for revascularization. Additionally, we examined this effect within a cohort of patients with either type 1 or type 2 DM to evaluate whether ranolazine had similar or greater benefits in this population.
Methods
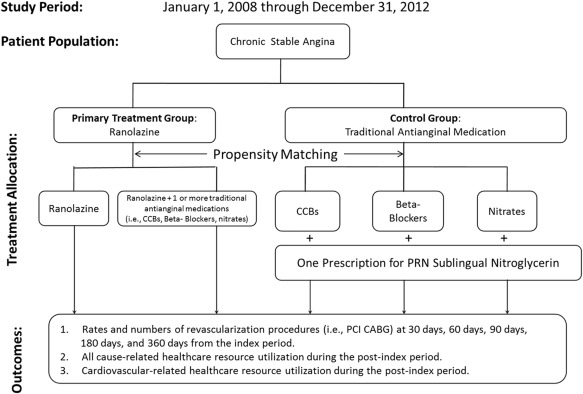
To compare differences between ranolazine and traditional AA therapies, we conducted a retrospective, quasi-experimental between-group analysis using propensity matching. The data source was the Clinformatics Data Mart representing a commercially available data source for research purposes from United Healthcare’s nationwide patient population. The patient population included United Healthcare’s fully insured, Medicaid, and Medicare Advantage population representing 49 million unique subjects. These data represent integrated enrollment, medical and prescription claims data augmented with laboratory test results data for 40% of the patient population. As United Healthcare is the largest provider nationwide of Medicare Advantage plans, the Clinformatics Data Mart represents a substantially large proportion of patients aged ≥65 years compared to other health plan data. The data were blinded to protect patient privacy but allowed for patient-linked longitudinal analysis. The study duration was a 5-year period ranging from January 1, 2008, to December 31, 2012.
Four mutually exclusive study cohorts were identified. The primary treatment cohort represented patients prescribed ranolazine. Three study control cohorts represented patients receiving traditional AA treatments (defined as a BB, CCB, or LAN, each supplemented with sublingual nitroglycerin). We identified cohorts in which an individual patient’s original AA therapy was inadequate, necessitating initiation of a second AA agent (the addition of/switch to ranolazine or a different traditional AA agent). This allowed the identification of patients whose angina was considered insufficiently controlled, requiring a change in their medication regimen. In addition to these cohorts, a DM subpopulation was identified from those with CSA who also had a diagnosis for type 1 or type 2 DM before medication change.
The primary treatment cohort consisted of patients newly initiated on ranolazine with 12 months of continuous enrollment before the first prescription for ranolazine (designated as the index date) and 12 months of continuous enrollment after the index date. The 12 months before the index date was designated as the preindex period, whereas the 12 months after the index date was designated as the postindex period. Patients newly initiated on ranolazine could have done so in the following manner: (1) a prescription of ranolazine added to existing traditional AA therapies that patients were taking during the preindex period or (2) patients could have switched to ranolazine after taking traditional AA therapies in the preindex period. Patients also were required to have an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9) code for CSA (413.xx or 414.xx) and/or chest pain (to include chest pain, unspecified: 786.50, precordial pain: 786.51; other chest pain: 786.59) at any time in the preindex period.
Control cohorts were constructed in a similar manner to the primary treatment group. The index event was defined as the date when the patient was prescribed a new AA agent (not used within the last 12 months) either by a change in or the addition of a traditional AA medication, with the additional requirement of having a prescription for sublingual nitroglycerin. Our definition of traditional AA medications included BBs, CCBs, and LANs. Patients were categorized into 3 specific control groups based on the medication addition/switch at the index date. In addition, patients were also required to have at least 1 ICD-9 code for CSA and/or chest pain at any time in the preindex period.
From the primary treatment and control cohorts, we also identified a subpopulation of patients with DM, specifically those with CSA who also had a diagnosis for type 1 or type 2 DM. The subpopulation of the diabetic cohort required patients in both the primary treatment group and each of the control groups to have at least 1 diagnosis for DM (ICD-9 250.xx) in the 12-month preindex period. Subsequently, as in the previous cohorts, there were 4 mutually exclusive diabetic cohorts: a primary DM cohort of patients with CSA (and related conditions) who had DM before their initiation of ranolazine and 3 control cohorts of patients with CSA (and related conditions) who had DM before their initiation of traditional AA therapies.
The proposed study design for the primary treatment and control cohorts is described in Figure 1 . The following outcomes were examined for the primary treatment and all 3 control groups:
- •
Revascularizations: defined as both as the number and percent of patients with percutaneous coronary interventions (PCI) or coronary artery bypass grafting (CABG) observed at 30, 60, 90, 180, and 360 days after the index date. Current Procedural Terminology, Fourth Edition, and ICD-9 codes available are available online in Supplementary Table 1 .
- •
CV-related health care resource utilization: defined as the mean number of hospitalizations, emergency room visits, outpatient visits, and average length of inpatient stay for any of the following CV-related conditions: acute coronary syndrome (ACS), cardiac dysrhythmias, deep vein thrombosis, heart failure, hypertension, hyperlipidemia, pulmonary embolism, or stroke during the postindex period. The ICD-9 codes for the CV conditions are available online in Supplementary Table 2 .
- •
All-cause related health care resource utilization: defined as the mean number of hospitalizations, emergency room visits, outpatient visits, and average length of inpatient stay for all conditions, including CV conditions during the postindex period.
In addition, we also examined similar outcomes for the DM cohort, adding
- •
DM-related health care resource utilization: defined as the number of hospitalizations, emergency room visits, outpatient visits, and length of inpatient stay for DM-related utilization.
The following demographic and clinical measurements were also examined: gender, age (in different increments from 18 to 49 years and then in 5 years increments till 80 plus years), payer type (private, public [Medicare/Medicaid], and mixed [public and private, e.g., Medicare with Medigap policies]), region of the United States (Northeast, Midwest, South, West), Chronic Condition Index (CCI, an index of co-morbidity burden), and the following co-morbidities in the preindex period: ACS, chronic kidney disease, DM, heart failure, hypertension, hyperlipidemia. These co-morbidities were chosen as they were most relevant to CSA. The CCI was used to describe each patient’s overall co-morbidity burden. Indicator variables were created for 6 categories of reported co-morbidity scores. These categories included a range from 0 to 5 or more chronic comorbidities. The CCI is a part of the family of databases and software tools developed as part of the Healthcare Cost and Utilization Project, a Federal-State-Industry partnership sponsored by the Agency for Healthcare Research and Quality.
Propensity matching was used to pair each patient on ranolazine with a patient on traditional AA therapy in each of the control groups to make groups as comparable as possible. Each patient in the primary treatment cohort was matched to a patient in each of the 3 control cohorts in a 1:1 ratio using the nearest neighbor matching method. Using the variables available in the claims data, the assumption was made that most relevant differences between the 2 groups are captured by these observable and available variables. The matching variables selected were observed in the preindex period as they are exogenous to the outcomes observed during the postindex period and included age, gender, baseline CCI, presence of ACS, hypertension, DM, hyperlipidemia, heart failure, any revascularization, DM-related complications such as ketoacidosis or end-organ damage and baseline CV-related health care costs. The ICD-9 codes for DM complications are available online in Supplementary Table 3 . These matching variables may explain why patients are prescribed ranolazine, but that a patient is prescribed ranolazine is not influenced by these variables. Note as the DM cohort was derived from the matched primary treatment and a control cohort, no further propensity matching was needed. The propensity matching was conducted in the following steps.
Both descriptive and adjusted analysis was conducted between the primary treatment and all 3 control groups. The unadjusted analysis compared means and proportions for all specified outcome variables. Proportions of patients undergoing any revascularization for a given period (30, 60, 90, 180, 360 days) were compared using formal chi-square statistics. Number of per patient revascularizations and all health care utilization including average length of stay were compared using F statistics. Depending on the type of outcome variable, different statistical models were used for the adjusted regression analysis. Logistic regression models were used for the binary outcomes of revascularization. Number of per patient revascularizations and health care utilization–based outcomes including average length of stay are count variables with several zero-count observations. A negative binomial regression model was used to model these outcomes with separate regression models for each health care resource utilization outcome (i.e., outpatient visits, emergency room visits, hospitalizations, and average length of stay). The explanatory variables for all models included age in which age <50 years was the reference group; gender in which male was the reference group; payer type in which private insurance was the reference group; CCI; and medication adherence. Adherence was measured as the proportion of days covered (PDC) in the follow-up period (after the index date) for the number of days with any therapy (ranolazine or traditional AA) during the follow-up expressed as a percentage.
Results
From January 1, 2008, through December 31, 2012, of those meeting the inclusion criteria, 8,008 were identified with CSA receiving either a BB (n = 2,002), CCB (n = 2,002), LAN (n = 2,002), or ranolazine (n = 2,002; Figure 2 ). As seen in Table 1 , baseline characteristics were well matched between groups. Most patients were men, had a mean age of 66 years, and resided within the Southern United States. The type of medical coverage varied between therapeutic treatment groups. For private and public insurance, most patients receiving LANs and ranolazine had private insurance, and the majority taking BBs and CCBs had public insurance. Co-morbidity burden was high. The mean baseline CCI was from 5.06 to 5.15 in which most patients had hypertension and hyperlipidemia followed by DM. About 1/3 of patients had a previous history of ACS with about 20% having received a revascularization procedure in the preindex period. In terms of medication adherence, measured by PDC, a statistically significant difference existed between ranolazine and those patients receiving CCBs (81.6% vs 83.2%, p = 0.012, respectively) and LANs (81.6% vs 80.1%, p = 0.030, respectively.)
| BB (N=2002) | CCB (N=2002) | LAN (N=2002) | Ranolazine (N=2002) | |
|---|---|---|---|---|
| DEMOGRAPHICS | ||||
| Female | 36.9% | 36.0% | 35.3% | 36.8% |
| Male | 63.1% | 64.0% | 64.7% | 63.2% |
| Mean Age (Years) | 66.3 | 66.3 | 66.2 | 66.3 |
| Coverage Type | ||||
| Private | 46.4% ∗∗ | 48.7% | 50.1% | 51.2% |
| Public | 53.1% ∗∗∗ | 50.8% | 49.3% | 47.8% |
| Mixed | 0.40% | 0.50% | 0.60% | 0.90% |
| Region of the United States | ||||
| Northeast | 6.50% | 8.30% ∗ | 6.90% | 6.40% |
| Midwest | 22.1% | 24.8% ∗∗ | 25.8% ∗∗∗ | 21.0% |
| South | 55.6% ∗∗ | 51.2% ∗∗∗ | 51.1% ∗∗∗ | 59.8% |
| West | 13.9% ∗ | 14.1% ∗ | 14.7% ∗∗ | 11.7% |
| Missing Data (%) | 1.80% ∗ | 1.60% | 1.40% | 1.00% |
| CLINICAL DEMOGRAPHICS | ||||
| Pre-Index Comorbidity Burden | ||||
| Mean Baseline CCI | 5.06 | 5.11 | 5.15 | 5.09 |
| Pre-Index Specific Comorbidities | ||||
| Acute Coronary Syndromes | 33.6% | 36.1% | 36.9% | 36.2% |
| Hypertension | 90.8% | 89.9% | 88.6% | 89.1% |
| Hyperlipidemia | 88.6% | 88.7% | 88.3% | 89.2% |
| Diabetes Mellitus | 46.6% | 47.0% | 46.8% | 45.7% |
| Diabetes Mellitus with Complications | 28.5% | 29.3% | 29.0% | 29.1% |
| Heart Failure | 27.4% | 27.5% | 27.1% | 27.8% |
| Revascularization | 19.8% | 21.4% | 21.2% | 20.9% |
| Pre-Index CV-Related Healthcare Costs ($) | $16,654 | $ 17,675 | $17,795 | $18,230 |
| Post-Index PDC | 80.3% | 83.2% ∗ | 80.1% ∗ | 81.6% |
The adjusted risk for revascularization procedures (PCI and CABG) was higher in all therapeutic groups at each of the study time points compared to ranolazine, with the highest risk being for those patients receiving a BB or LANs ( Table 2 ). The odds for BB users was statistically significant across all study time points (range, odds ratio [OR] 2.76 to 4.34) with the most pronounced difference in risk occurring within 30 days after the index date. LANs use, although associated with slightly lower odds for revascularization (range, OR 2.10 to 2.59), remained statistically significant across all study time points compared to ranolazine. Similar to BB users, the most pronounced odds for LAN users was within 30 days after the index date. Although CCB users also had greater odds for PCI compared to ranolazine across all study time points (range, OR 1.20 to 1.51), contrary to BB and LAN users, the highest risk and only time point to reach statistical significance was at 360 days after the index date.



