Although transthoracic echocardiography (TTE) and cardiac magnetic resonance (CMR) are validated in quantitation of mitral regurgitation (MR), discrepancies may occur. This study assesses the agreement between TTE and CMR in MR and evaluates characteristics and clinical outcome of patients with discrepancy. From our institutional database, 70 subjects with MR underwent both TTE and CMR within 30 days (median 3 days). MR was evaluated semiquantitatively (n = 70) using a 4-grade scale and quantitatively (n = 60) with calculation of regurgitant volume (RVol) and regurgitant fraction (RF). Of the 70 subjects, qualitative assessment by TTE yielded 30 subjects with mild MR, 17 moderate, and 23 moderately severe or severe MR. Exact concordance in MR grade was seen in 50% and increased to 91% when considering concordance within one grade of severity (κ = 0.44). A modest correlation was observed for RVol and RF between both methods ( r = 0.59 and 0.54, respectively, p <0.0001). Ten patients had a significant discrepancy in quantitative MR (difference in RF >20%); the frequency of secondary MR was higher (100% vs 46%; p = 0.003) in patients with discrepancy. Although interobserver variability in RF was higher with TTE compared with CMR (−5.5 ± 15% vs 0.1 ± 7.3%), patients with discrepancy were equally distributed by severity and clinical outcome without an overestimation by either method. In conclusion, there is a modest agreement between TTE and CMR in assessing MR severity. In patients with discrepancy, there is a higher prevalence of functional MR, without a consistent overestimation of MR severity by either method.
The severity of mitral regurgitation (MR) is a major determinant of prognosis and management of patients with mitral valve disease. Valvular heart disease guidelines favor surgical repair in patients with asymptomatic severe MR, making the differentiation between various grades of regurgitation crucial for patient management. Evaluation of MR is typically performed first with echocardiography, using an integrative approach of qualitative and quantitative parameters. Among quantitative measurements are those of regurgitant volume (RVol) and regurgitant fraction (RF) derived with Doppler echocardiography. Cardiac magnetic resonance imaging (CMR) is an emerging method to assess MR severity. The strength of CMR is in its volumetric quantitation of RVol and RF, derived usually from left ventricular (LV) volumes and phase contrast (PC) technique. CMR is often reserved for assessment of valve regurgitation in technically difficult or inconclusive echocardiographic studies. The present study was conducted to assess first, the agreement between transthoracic echocardiography (TTE) and CMR in the clinical evaluation of patients with various degrees of MR using both an integrative and quantitative approach; second, to assess if there were particular findings on TTE associated with a discrepancy in results that would prompt referral to CMR, and finally, to evaluate the outcome of patients who had a significant discrepancy in results between the 2 methods.
Methods
From the databases of the echocardiography and CMR laboratories of Houston Methodist Hospital from 2008 to 2012, patients were identified who had MR by both methods, and no other significant valvular disease, and had undergone both TTE and CMR within 30 days of each other. All patients with more than mild MR were included, but those with mild MR were limited to not more than 40% of the cohort so as not to overweigh assessment of mild regurgitation, a clinically insignificant lesion. There were 98 subjects who fulfilled the previously mentioned criteria; 28 patients were excluded (22 because of echo and 6 because of CMR) because of the following: incomplete (n = 15) or technically difficult studies (n = 7), unavailability of PC velocity mapping data from CMR (n = 3) and others (n = 3).
The study population thus involved 70 subjects. The TTE and CMR studies were retrieved from digital storage, the original clinical evaluation of MR severity was noted, and the studies were reanalyzed by independent investigators blinded to the original data. The TTE images had standard imaging and Doppler acquisitions. The study was reinterpreted semiquantitatively and quantitatively by an independent level 3 echocardiographer blinded to the results of the CMR and TTE original reports. The cause of MR (primary or secondary) was noted. The semiquantitative and quantitative interpretation of MR severity (4 grades: mild, moderate, moderately severe, and severe) was based on the integrative approach recommended by the American Society of Echocardiography, which was used irrespective of MR mechanism. LV volumes were determined with the method of discs. Quantitation of MR severity was performed with the volumetric pulsed Doppler approach, as this method is the most comparable to the quantitative CMR method, is used more often than flow convergence in our laboratory since its early validation and has advantages in eccentric MR jets, multiple jets, and mid-to-late systolic MR. RVol was determined from the difference of stroke volumes by pulsed Doppler at the mitral annulus and the LV outflow ( Figure 1 ). The RF was calculated dividing the RVol by the stroke volume at the mitral annulus. To assess variability, another level 3 reader requantitated RVol and RF in 15% of patients. Variability in comparative measurements of stroke volume derived at the mitral annulus and LV outflow in subjects without regurgitation, that is, “pseudo regurgitation” was previously determined in our laboratory and was found to be within 20% in absolute value and reached 25% in patients with cardiomyopathy. This variability in flow measurement was also retested in this investigation in 20 additional subjects without evidence of regurgitation.
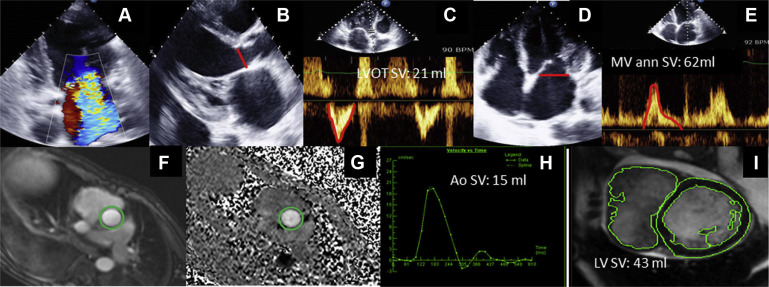
CMR studies were performed on 1.5 T Avanto or 3T Verio CMR scanner (Siemens, Erlangen, Germany) using a dedicated phased-array receiver coil placed on the chest and electrocardiographic gating. A series of steady-state free precession cine images were obtained in the short-axis orientation from mitral annulus to LV apex in 1 cm increments: slice thickness 6 mm, interslice gap of 4 mm, in-plane resolution 2.0 × 1.5 mm, parallel imaging with twofold acceleration factor, and minimum allowable repetition/echo times. To achieve high contrast between myocardium and blood cavity, the maximum allowed flip angle was used (typically 75° at 1.5 T and 50° at 3T). In addition to short-axis views, 4-, 3-, and 2-chamber long-axis views were acquired to allow for assessment of systolic mitral annular plane descent. PC images were acquired at velocity encoding 150 to 200 cm/sec (ensuring no aliasing), temporal resolution 50 ms/frame, spatial resolution of 2.5 × 2.0 mm with slice thickness of 5.0 mm. PC images were performed at the sinotubular junction to assess the systemic stroke volume. Total LV stroke volume and ejection fraction were calculated from manual planimetry of LV end-diastolic and end-systolic volumes. Aortic flow was derived by contouring of PC images with correction performed for baseline flow offset. RVol was derived by subtracting systolic forward flow across the aortic valve from LV stroke volume as per Society of Cardiovascular Magnetic Resonance position statement ( Figure 1 ). Regurgitant fraction was obtained by dividing the RVol by the LV stroke volume. MR severity by CMR was determined semiquantitatively (grades 1 to 4) and quantitatively on the basis of RF and RVol using the American Society of Echocardiography guidelines. Another level 3 CMR reader reanalyzed 15% of the patients to determine interobserver agreement. Variability in stroke volume between the LV method and PC aortic method in subjects without regurgitation (“pseudo regurgitation”) was assessed in 20 additional subjects.
Continuous parametric data were expressed as mean ± SD and nonparametric data as median (range). The agreement between the semiquantitative MR severity between TTE and CMR was assessed with linear weighted κ analysis. Agreement and correlations between the quantitative parameters were evaluated with Pearson correlation and Bland–Altman methods. Continuous parametric groups were compared using the Student t test. The Mann–Whitney test was used to compare 2 groups with continuous nonparametric data. Fisher’s exact test was used to compare categorical data. Clinically significant differences in MR severity between methods were considered to be >1 grade or a difference in RF of >20% in absolute value on the basis of variability data from our laboratory. The 20% cutoff was the more stringent criterion, rather than the 25% cutoff for functional MR. RF was chosen as the parameter to evaluate significant quantitative differences between the 2 methods because it incorporates the range in total stroke volume and RVol observed with different LV sizes and function in the population.
To identify variables that may be associated with significant discrepancies in assessment of MR severity, clinical and TTE parameters were compared in patients with and without discrepancies. Finally, to assess the clinical outcome of patients with discrepancy in MR severity, the patients’ clinical records were reviewed for the clinical opinion by the treating physicians as to whether the MR was clinically significant (grade 3 or 4) and for overall clinical outcome (need for additional testing, management, hospital admissions for heart failure, or death). Clinicians had access to both TTE and CMR clinical studies for each patient during management but not to the reinterpreted data by the investigators. The software used for statistical analysis was SSPS and Analyze-it. Statistical significance was set at p <0.05.
Results
The characteristics of the 70 patients are summarized in Table 1 . The median interval between CMR and TTE studies was 3 days (range 0 to 30) and was 1 day in the 60 patients with quantitative parameters of MR, 60% of them being done within 3 days. None of the subjects had an interim clinical change or cardiac intervention. The hemodynamics and volumetric 2D echo and CMR data were similar ( Table 2 ). By TTE, 30 patients had mild MR, 17 moderate, and 23 moderately severe or severe MR. A modest agreement in MR severity was seen between TTE and CMR ( Table 3 ; κ = 0.44). Exact concordance in MR grade was seen in 50% and improved to 91% when considering concordance to be within one grade in severity; 6 patients (9%) had discordance of 2 or more grades, without a trend favoring a greater estimation of severity by either method. All these data were slightly better compared with the original clinical read of the studies: exact concordance in 47%, increasing to 86% within one grade difference; 10 patients having a discordance of 2 or more grades (14%).
| Age (years) | 61±16 |
| Men | 36 (51%) |
| Left Ventricular Ejection Fraction (%) | 47±21 |
| Median interval between CMR and TTE (days) | 3 (0-30) |
| Secondary mitral regurgitation | 35 (50%) |
| Hypertension | 13 (19%) |
| Diabetes Mellitus | 17 (24%) |
| History of myocardial infarction | 7 (10%) |
| Diuretics | 37 (53%) |
| Beta-blockers | 16 (23%) |
| Nitrates | 13 (19%) |
| Variable | TTE | CMR | p-value |
|---|---|---|---|
| Heart rate (beat/min) | 80±15 | 82±14 | 0.53 |
| Systolic blood pressure (mmHg) | 123±24 | 119±18 | 0.33 |
| Diastolic blood pressure (mmHg) | 70±11 | 68±12 | 0.60 |
| Left ventricular end-diastolic volume (mL) | 180±74 | 200±85 | 0.19 |
| Left ventricular end-systolic volume (mL) | 104±70 | 119±88 | 0.32 |
| Regurgitant volume (mL) | 29±20 | 26±18 | 0.39 |
| Regurgitant fraction (%) | 34±17 | 32±14 | 0.49 |
| TTE | CMR | Total | |||
|---|---|---|---|---|---|
| Mild MR | Moderate MR | Moderately Severe MR | Severe MR | ||
| Mild MR | 20 | 7 | 3 | 0 | 30 |
| Moderate MR | 7 | 7 | 3 | 0 | 17 |
| Moderately Severe MR | 1 | 6 | 6 | 2 | 15 |
| Severe MR | 1 | 1 | 4 | 2 | 8 |
| Total | 29 | 21 | 16 | 4 | 70 |
Quantification of RVol and RF was feasible in 60 patients by both methods; RVol and RF were similar ( Table 2 ). A modest correlation was observed between CMR and TTE for RVol and RF ( r = 0.59 and 0.54 respectively, p <0.0001; Figures 2 and 3 ). Results were not significantly different when analysis was restricted to studies performed within 1 or 3 days. A stronger correlation was observed between LV outflow stroke volume by echo and aortic stroke volume by CMR ( r = 0.75; p <0.001) than between TTE mitral stroke volume and CMR LV stroke volume ( r = 0.66; p <0.001). Using the Bland–Altman method, the mean difference in RVol was −2 ± 17 ml and in RF −2 ± 16% ( Figures 2 and 3 ); although the mean differences were small, the limits of agreement were wide. Ten patients had a significant discrepancy in quantitative MR (>20% difference in absolute RF ; Figure 3 ). These patients encompassed the 6 patients who had significant discrepancy by semiquantitative criteria. To evaluate whether these discrepancies were due to observer variability or misinterpretation, a post hoc analysis was performed in which senior investigators in both echo and CMR reviewed the 10 discrepant subjects. Seven of 10 discrepant assessments could still not be resolved (10% of the total population) after second review.





